Abstract
Purpose
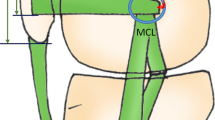
A comprehensive understanding of the biomechanical properties of the medial patellofemoral complex (MPFC) is necessary when performing an MPFC reconstruction. How components of the MPFC change over the course of flexion can influence the surgeon’s choice of location for graft fixation along the extensor mechanism. The purpose of this study was to (1) determine native MPFC length changes throughout a 90° arc using an anatomically based attachment and using Schöttle’s point, and (2) compare native MPFC length changes with different MPFC attachment sites along the extensor mechanism.
Methods
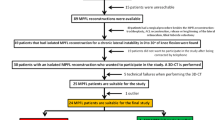
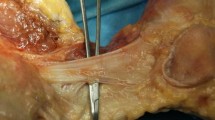
Eight fresh-frozen (n = 8), cadaveric knees were dissected of all soft tissue structures except the MPFC. The distance between the femoral footprint (identified through anatomical landmarks and Schottle’s point) and the MPFC was calculated at four attachment sites along the extensor mechanism [midpoint of the patella [MP], the center of the osseous footprint of the MPFC (FC), the superomedial corner of the patella at the quadriceps insertion (SM), and the proximal extent of the MPFC along the quadriceps tendon (QT)] at 0°, 20°, 40°, 60°, and 90° of flexion.
Results
Length changes were investigated between the MPFL femoral attachment site and the radiographic surrogate of the MPFL attachment site, Schottle’s Point (SP). Paired t tests at each of the four components showed no differences in length change from 0° to 90° when comparing SP to the anatomic MPFC insertion. MPFL length changes from 0° to 90° were greatest at the QT point (13.9 ± 3.0 mm) and smallest at the MP point (2.7 ± 4.4 mm). The FC and SM points had a length change of 6.6 ± 4.2 and 9.0 ± 3.8, respectively. Finally, when examining how the length of the MPFC components changed through flexion, the greatest differences were seen at QT where all comparisons were significant (p < 0.01) except when comparing 0° vs 20° (n.s.).
Conclusion
The MPFC demonstrates the most significant length changes between 0° and 20° of flexion, while more isometric behavior was seen during 20°–90°. The attachment points along the extensor mechanism demonstrate different length behaviors, where the more proximal components of the MPFC display greater anisometry through the arc of motion. When performing a proximal MPFC reconstruction, surgeons should expect increased length changes compared to reconstructions utilizing distal attachment sites.





Similar content being viewed by others
References
Askenberger M, Arendt EA, Ekström W, Voss U, Finnbogason T, Janarv P-M (2016) Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations. Am J Sports Med 44(1):152–158
Askenberger M, Moström EB, Ekström W, Arendt EA, Hellsten A, Mikkelsen C, Janarv P-M (2018) Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: a randomized controlled trial. Am J Sports Med 46(1):2328–2340
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation. Am J Sports Med 40(1):114–122
Camanho GL, de Viegas AC, Bitar AC, Demange MK, Hernandez AJ (2009) Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 25(6):620–625
Cofield RH, Bryan RS (1977) Acute dislocation of the patella: results of conservative treatment. J Trauma 17(7):526–531
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Huber C, Zhang Q, Taylor WR, Amis AA, Smith C, Nasab SHH (2020) Properties and function of the medial patellofemoral ligament: a systematic review. Am J Sports Med 48(3):754–766
Kernkamp WA, Wang C, Li C, Hu H, van Arkel ERA, Nelissen RGHH, LaPrade RF, van de Velde SK, Tsai T-Y (2019) The medial patellofemoral ligament is a dynamic and anisometric structure: an in vivo study on length changes and isometry. Am J Sports Med 47(7):1645–1653
Krackow KA, Thomas SC, Jones LC (1986) A new stitch for ligament-tendon fixation. Brief note. J Bone Jt Surg Am 68(5):764–766
Kruckeberg BM, Chahla J, Moatshe G, Cinque ME, Muckenhirn KJ, Godin JA, Ridley TJ, Brady AW, Arendt EA, LaPrade RF (2018) Quantitative and qualitative analysis of the medial patellar ligaments: an anatomic and radiographic study. Am J Sports Med 46(1):153–162
Oka S, Matsushita T, Kubo S, Matsumoto T, Tajimi H, Kurosaka M, Kuroda R (2014) Simulation of the optimal femoral insertion site in medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22(10):2364–2371
Pérez-Prieto D, Capurro B, Gelber PE, Ginovart G, Reina F, Sanchis-Alfonso V, Monllau JC (2017) The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 25(8):2420–2423
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20(2):331–336
Rood A, Hannink G, Lenting A, Groenen K, Koëter S, Verdonschot N, Kampen A (2015) Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med 43(10):2538–2544
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40(8):1916–1923
Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H (2009) Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men. Am J Sports Med 37(8):1513–1521
Song SY, Pang C-H, Kim CH, Kim J, Choi ML, Seo Y-J (2015) Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med 43(5):1165–1171
Steensen RN, Dopirak RM, Mcdonald WG (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32(6):1509–1513
Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA (2012) The medial patellofemoral ligament. Am J Sports Med 40(8):1871–1879
Tanaka MJ (2016) Variability in the patellar attachment of the medial patellofemoral ligament. Arthrosc J Arthrosc Relat Surg 32(8):1667–1670
Tanaka MJ, Voss A, Fulkerson JP (2016) The Anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Jt Surg Am 98(14):1199–1205
Tateishi T, Tsuchiya M, Motosugi N, Asahina S, Ikeda H, Cho S, Muneta T (2011) Graft length change and radiographic assessment of femoral drill hole position for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19(3):400–407
Waterman B, Belmont P, Owens B (2012) Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg 25(1):51–58
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Cole is on the editorial or governing board for the American Journal of Orthopedics, American Journal of Sports Medicine, Cartilage, Journal of Shoulder and Elbow Surgery (editor only), and Journal of the American Academy of Orthopaedic Surgeons (editor only). Dr. Cole receives research support from Aesculap/B.Braun, Arthrex, Inc., National Institutes of Health (NIAMS & NICHD), and Regentis. Dr. Cole is on the board or committee member for Arthroscopy Association of North America and International Cartilage Repair Society. Dr. Cole is a paid consultant for Arthrex, Inc. and Regentis. Dr. Cole receives IP royalties from Arthrex, Inc. and Elsevier Publishing. Dr. Cole has stock or stock options in Bandgrip Inc., Ossio, and Regentis. Dr. Cole receives publishing royalties from Operative Techniques in Sports Medicine. Dr. Cole receives financial or material support from Athletico, JRF Ortho, Operative Techniques in Sports Medicine, and Smith & Nephew.
Dr. Farr is on the editorial or governing board for the American Journal of Orthopedics and Cartilage. Dr. Farr receives research support from Active Implants, Arthrex, Inc., Episurf, Fidia, JRF Ortho, Moximed, Organogenesis, Samumed, Vericel, Norvartis, and ZimmerBiomet. Dr. Farr is a paid consultant for Aesculap/B.Braun, Cartiheal, Cook Biotech, Inc., Exactech, Moximed, Organogenesis, Regentis, Samumed, and ZKR Orthopedics, Inc. Dr. Farr receives IP royalties from Arthrex, Inc., Biopoly, LLC, and Organogensis. Dr. Farr has stock or stock options in MedShape, Inc., Ortho Regenerative Tech, Inc. Dr. Farr is a paid presenter or speaker for Arthrex, Inc., Moximed, Organogenesis, and Vericel. Dr. Farr receives publishing royalties and financial or material support from Springer and Thieme Medical Publishers, Inc.
Dr. Yanke receives research support from Arthrex, Inc, Vericel, and Organogenesis. Dr. Yanke is a paid consultant for CONMED Linvatec, JRF Ortho, and Olympus and an unpaid consultant for PatientIQ, Smith & Nephew, and Sparta Biomedical. He has stock or stock options in PatientIQ.
Dr. Chahla is an unpaid consultant for Arthrex, Inc, CONMED Linvatec, and Smith & Nephew.
Funding
There is no funding source.
Ethical approval
This study did not need IRB approval due to the use of cadaveric specimen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huddleston, H.P., Campbell, K.J., Madden, B.T. et al. The quadriceps insertion of the medial patellofemoral complex demonstrates the greatest anisometry through flexion. Knee Surg Sports Traumatol Arthrosc 29, 757–763 (2021). https://doi.org/10.1007/s00167-020-05999-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05999-2