Abstract
Purpose
The predictive role of patient-specific characteristics and radiographic parameters on medial unicompartmental knee arthroplasty (UKA) outcomes is well known, but knowledge of these predictors is lacking in lateral UKA. Therefore, purpose of this study was to assess the predictive role of these parameters on short-term functional outcomes of lateral UKA.
Methods
In this retrospective cohort study, Western Ontario and McMaster Universities Arthritis Index scores were collected at 2-year follow-up (median 2.2 years, range 2.0–4.0 years) in 39 patients who underwent lateral UKA. Patient-specific characteristics included age, BMI and gender, while radiographic parameters included osteoarthritis severity of all three compartments and both preoperative and postoperative hip-knee-ankle alignment.
Results
BMI, gender, age and preoperative valgus alignment were not correlated with functional outcomes, while postoperative valgus alignment was correlated with functional outcomes (0.561; p = 0.001). Postoperative valgus of 3°–7° was correlated with better outcomes than more neutral (−2° to 3° valgus) alignment (96.7 vs. 85.6; p = 0.011). Postoperative alignment was a predictor when corrected for patient-specific characteristics (regression coefficient 4.1; p < 0.001) and radiological parameters (regression coefficient 3.8; p = 0.002).
Conclusions
Postoperative valgus alignment of 3°–7° was correlated with the best short-term functional outcomes in lateral UKA surgery, while patient-specific parameters and preoperative alignment were not correlated with functional outcomes. Based on these findings, a surgeon should aim for valgus alignment of 3°–7° when performing lateral UKA surgery for optimal functional outcomes.
Level of evidence
Prognostic study, Level II.
Similar content being viewed by others
Introduction
Historically, poor results of unicompartmental knee arthroplasty (UKA) in the setting of isolated unicompartmental osteoarthritis (OA) have been reported [14]. Kozinn and Scott [20] therefore proposed strict patient selection criteria in 1989, which led to better outcomes and lower revision rates [2, 19, 33]. Nowadays, high BMI is identified as a predictor of poor functional outcomes [6, 16], while contradictory findings were reported regarding age and gender [21, 34]. It has also been shown in medial UKA slight postoperative varus of 1°–4° is correlated with better functional outcomes than neutral (−2° to 1°) or more varus (5°–7°) alignment [41].
Because several anatomic and kinematic differences between the medial and lateral compartment exist [13, 15, 25, 32, 35, 43], it is not justified to simply use these optimal alignment angles for lateral UKA. Harrington described that in patients with moderate valgus deformity, which is often the case in lateral OA [36], the mechanical load was transferred through the medial compartment during the dynamic phase [11]. Based on these findings, Ohdera et al. advised aiming for more valgus alignment (5°–7°) during lateral UKA.
To our knowledge, however, no study has assessed the role of postoperative alignment on functional outcomes besides the general statement that “overcorrection should be avoided to prevent medial OA progression” [26, 28, 31, 38]. In addition, to our knowledge no studies have assessed the influence of other patient-specific characteristics on outcomes of lateral UKA procedures. The purpose of this study therefore is to assess the role of patient-specific characteristics and radiographic parameters on short-term functional outcome in patients undergoing lateral UKA. The hypothesis of this study was that young patients with a high BMI and neutral alignment have poor functional outcomes at short-term follow-up.
Materials and methods
An electronic search was performed for all patients who underwent lateral UKA surgery between 2008 and 2013. Surgical inclusion criteria consisted of (1) isolated lateral OA as primary indication, (2) intact cruciate ligaments, (3) passively correctable valgus deformity and (4) fixed flexion-deformity <10°. All patients were included who completed minimum 2-year follow-up of patient-reported outcomes. Of the 116 patients undergoing lateral UKA, 39 patients completed minimum of 2-year follow-up and were included.
Using a robotic-assisted surgical platform (MAKO Tactile Guidance System, MAKO Surgical Corporation, Ft. Lauderdale, FL, USA), all patients received a lateral RESTORIS® MCK Onlay Tibial implant (MAKO Surgical Corporation, Ft. Lauderdale, FL, USA) as previously described [27, 30]. Surgical alignment goal was a relative undercorrection of the preoperative valgus alignment in order to avoid OA progression in the medial compartment [26, 28, 31, 38]. One author performed all surgeries (AP).
Patients were categorized by gender, age (i.e. <65 and ≥65 years) and BMI according to the World Health Organization (i.e. <25, 25–30 and ≥30 kg/m2) [29]. BMI was missing in nine patients. Preoperative radiographic-collected parameters included OA severity and lower limb alignment. OA severity of the medial compartment, lateral compartment and patellofemoral compartment was measured using the Kellgren–Lawrence (KL) grading system [17]. Alignment was measured preoperatively and 1 month postoperatively using weight-bearing hip-knee-ankle radiographs as described by Moreland et al. [23]. Alignment was defined as the angle between the femoral and tibial mechanical axis, and this method has a reliability measurement of <1.0° [37, 39]. The femoral axis was measured as the line from the centre of the femoral head to the centre of the femoral notch, whereas the tibial axis was measured as the line from the centre of the tibial spine to the centre of the talus. A positive angle value indicates valgus alignment, and a negative angle value indicates varus alignment. Patient-specific demographic data are displayed in Table 1 and pre- and postoperative radiographic data in Table 2.
Patient-reported outcomes were collected using the Western Ontario and McMaster Universities Arthritis Index (WOMAC). WOMAC is a questionnaire, which quantifies the functional outcome using 24 Likert-scale questions and is validated in the setting of knee OA [4, 5]. Questionnaires were collected routinely during clinic visits and by electronic mail both preoperatively and 2 years postoperatively (median 2.2 years; range 2.0–4.0 years). The Institutional Review Board of Hospital for Special Surgery approved this study (2013-056).
Statistical analysis was performed using SPSS version 21 (SPSS Inc., Armonk, NY. USA). Independent t tests and one-way analysis of variance (ANOVA) with post hoc LSD tests were used to assess differences in WOMAC scores between patient-specific demographics. Pearson correlation analysis was then used to assess correlations between pre- and postoperative radiographic parameters and postoperative WOMAC scores. A correlation coefficient <0.20 was considered as a very weak correlation, between 0.20 and 0.39 as weak, between 0.40 and 0.59 as moderate, between 0.60 and 0.79 as strong and ≥0.80 as very strong [10]. Postoperative alignment was both categorized in three groups (i.e. −2° to 1°, 1°–4° and 4°–7° as used by Vasso et al. [41]) and two groups (i.e. −2° to 3° and 3°–7°). One-way ANOVA and independent t tests were used to compare these groups. Finally, linear regression analysis was used to assess the predictive value of postoperative alignment on functional outcome using total WOMAC score. Because only 39 patients could be included, we used a maximum of four factors per linear regression analysis. All statistical tests were two-sided, and differences were considered statistically significant when p < 0.05.
Results
Patient-specific characteristics
No significant differences were found between age, BMI and gender in preoperative total WOMAC scores. Similarly, no significant differences in postoperative WOMAC scores were found in the patient-specific characteristics (Table 1).
Radiographic parameters
No correlation was found between WOMAC score and preoperative valgus. Similarly, no correlation was found between OA severity of all three compartments and the WOMAC score. Postoperatively, however, a correlation was found between postoperative valgus alignment and total WOMAC score (0.546; p = 0.001) (Table 2).
Postoperative alignment
Patients with postoperative valgus alignment between 1° and 4° (92.1 ± 10.8) and between 4° and 7° (97.1 ± 4.7) had significant better functional outcomes than with postoperative alignment between −2° and 1° (79.6 ± 17.2, respectively, p = 0.030 and p = 0.013). Furthermore, patients with postoperative valgus of 3°–7° had better outcomes (96.7 ± 4.1) than patients with postoperative valgus of −2° to 3° (85.6 ± 15.4; p = 0.011) (Table 3).
Linear regression showed that postoperative valgus was the only predictor of a higher WOMAC score. This was both seen when corrected for preoperative patient-specific characteristics (regression coefficient 4.1; p = < 0.001) and when corrected for preoperative radiographic parameters (regression coefficient 3.8; p = 0.002). The R 2 of the models were 0.459 and 0.399, respectively (Table 4).
Discussion
The most important finding of the present study was that postoperative alignment was an independent predictor of functional outcomes in lateral UKA patients. More specific, valgus alignment of 3°–7° was correlated with the best short-term functional outcomes. The patient-specific characteristics such as age, BMI and gender were not correlated with postoperative WOMAC scores at 2-year follow-up.
Several authors have discussed the role of overcorrection and undercorrection of preoperative varus alignment in patients who undergo medial UKA procedure. Hernigou and Deschamps [12] performed a study in which they compared the postoperative varus angle with Knee Society Score (KSS) and Hospital for Special Surgery scores. They compared scores between patients with a postoperative valgus angle, a varus angle between 0° and 10° and a varus angle >10°. They found that a varus angle of 0°–10° was correlated with the best functional outcomes. Overcorrection of varus deformity to a valgus angle was associated with increased OA progression at the lateral compartment, while undercorrection to a varus >10° was correlated with increased polyethylene wear. Similarly, Chatellard et al. [7] showed in a retrospective study of 559 medial UKAs that a postoperative varus angle >5° was associated with mechanical failure. More recently, Vasso et al. [41] performed a retrospective study in which they compared functional outcomes in patients who had different postoperative varus angles following medial UKA surgery. Patients with a postoperative varus angle of 1°–4° reported the best outcomes and they therefore recommended aiming for slight varus.
To our knowledge, however, no studies have assessed the role of postoperative alignment on functional outcomes following lateral UKA surgery. Differences between the medial and lateral compartment exist [11, 13, 15, 25, 32, 35, 43] and simply using 1°–4° of valgus as a goal of lateral UKA surgery is therefore not likely to be appropriate [41]. Harrington assessed the load carried by the medial and lateral compartment in patients with varus or valgus deformity in both the static phase and dynamic phase [11]. He showed in his study that in patients with varus deformity the load was transferred through the medial compartment in both the static and dynamic phase. In patients with valgus deformity, the load was transferred through the lateral compartment during the static phase, but this load was surprisingly shifted through the medial compartment during the dynamic phase in patients with moderate valgus alignment. This difference in kinematics in patients with varus and valgus deformity suggests that different postoperative alignment might be necessary for lateral UKA when compared to medial UKA. Ohdera et al. [26] therefore advised to aim for 5°–7° of postoperative valgus in patients with lateral UKA. Although several authors acknowledge the avoidance of overcorrection in lateral UKA [18, 22, 28, 31, 38], this is to our knowledge the first study that quantified the influence of postoperative alignment on functional outcomes. The data confirmed the statement of Ohdera that surgeons should aim for postoperative valgus with lateral UKA. When comparing the three postoperative alignment groups, data showed that patients with a neutral alignment do significantly worse compared to patients with valgus alignment. Although patients with a postoperative alignment of 4°–7° had better functional outcomes than patients with a postoperative alignment of 1°–4°, these differences were not significant. Analysis also showed that patients with a postoperative valgus of 3°–7° had better postoperative outcomes than patients with more neutral alignment. The optimal amount of valgus alignment is different from the aforementioned optimal varus alignment that is seen in medial UKA procedures [7, 18, 41]. This is likely to be explained by the aforementioned anatomic and kinematic differences between both compartments.
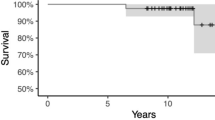
Correlation analysis and linear regression models in this study showed that postoperative alignment is a predictor for functional outcomes. Furthermore, the R 2 were high, which indicates that alignment was a strong predictor of functional outcomes. Interestingly, preoperative OA severity of the compartments was not predictive for functional outcomes at short-term follow-up even though OA progression in these compartments is considered as the most common failure mode [2, 8, 9]. It seems that, when appropriate patient selection is performed, OA progression is not related to the amount of OA severity at the time of surgery but is caused by the amount of valgus alignment. One patient in this study had a preoperative valgus of 6.7°, but alignment was overcorrected to a varus of 2.0° (measured at hip-knee-ankle radiographs). At 2.3-year follow-up, patient reported a total WOMAC score of 52 and medial OA progression was seen at radiographic follow-up (Fig. 1).
Radiographs of an 85-year-old man are shown. Preoperatively (left radiograph), a valgus angle of 6.7° was measured on hip-knee-ankle radiographs and no medial OA was seen. Unfortunately, the alignment was overcorrected to 2.0° of varus. At 2.3-year follow-up, this patient reported a total WOMAC score of 52 with medial compartment OA progression (right radiograph)
Although any differences in outcomes between younger and older patients could not be detected, some controversy exists around the role of age on functional outcomes [40, 42]. Thompson et al. [40] reported higher KSS in patients younger than 60 years, while Von Keudell et al. [42] could not find any difference in patient satisfaction between younger and older patients. With regard to BMI, several studies showed that a higher BMI is correlated with poor functional outcomes [6, 24, 40]. However, most patients in these studies underwent medial UKA and studies assessing functional outcomes following lateral UKA are lacking. In this study, patients with BMI ≥ 30 had worse functional outcomes (82.8 ± 21.1) compared to patients with a BMI < 25 (91.1 ± 8.3) and a BMI between 25 and 30 (91.6 ± 12.7), but these differences were not statistically significant. This could be explained by the fact only six patients had a BMI ≥ 30. Large studies or registries are necessary to further assess the role of these factors on outcomes due to the low frequency of lateral UKA.
This study has several limitations. As previously mentioned, the number of patients with preoperative data (n = 25) and follow-up (n = 39) is relatively small. Therefore, future studies are necessary to show differences in functional outcome between BMI ≥ 30 and <30. This low number of patients is seen in the literature due to the low frequency of UKA procedure at the lateral compartment (5–10 %) [1, 3]. Another limitation is that no optimal upper limit of postoperative valgus alignment could be found. Due to the tight control of alignment afforded by the robotic-assisted system, the largest postoperative valgus was 7° and therefore studies with larger differences in postoperative alignment are needed to assess the optimal upper limit of postoperative valgus alignment in lateral UKA. Finally, this study reported patient-reported functional outcomes and did therefore not report objective clinical results.
The findings of this study showed that postoperative alignment is correlated with short-term functional outcomes. Based on these findings, a surgeon should aim for an undercorrection of 3°–7° of valgus, when performing lateral UKA surgery, in order to achieve optimal short-term functional outcomes.
Conclusions
In lateral UKA, postoperative alignment appears to be a key predictor of early functional outcomes. As in medial UKA, functional outcome is sensitive to postoperative alignment; interestingly, however, more undercorrection appears to be necessary in lateral UKA (3°–7° of undercorrection) compared to medial UKA (1°–4° of undercorrection). Future studies are needed to evaluate the effect of valgus alignment on both long-term functional outcomes and revision rates.
References
Annual Report 2014 Australian Hip and Knee Arthroplasty Register (2014). https://aoanjrr.dmac.adelaide.edu.au/documents/10180/172286/AnnualReport2014
Ashraf T, Newman JH, Evans RL, Ackroyd CE (2002) Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Joint Surg Br 84(8):1126–1130
Baker PN, Jameson SS, Deehan DJ, Gregg PJ, Porter M, Tucker K (2012) Mid-term equivalent survival of medial and lateral unicondylar knee replacement: an analysis of data from a National Joint Registry. J Bone Joint Surg Br 94(12):1641–1648
Bellamy N, Campbell J, Hill J, Band P (2002) A comparative study of telephone versus onsite completion of the WOMAC 3.0 osteoarthritis index. J Rheumatol 29(4):783–786
Bellamy N, Campbell J, Stevens J, Pilch L, Stewart C, Mahmood Z (1997) Validation study of a computerized version of the Western Ontario and McMaster Universities VA3.0 Osteoarthritis Index. J Rheumatol 24(12):2413–2415
Bonutti PM, Goddard MS, Zywiel MG, Khanuja HS, Johnson AJ, Mont MA (2011) Outcomes of unicompartmental knee arthroplasty stratified by body mass index. J Arthroplasty 26(8):1149–1153
Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J, Societe d’Orthopedie de Traumatologie de lO (2013) Medial unicompartmental knee arthroplasty: Does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 99(4 Suppl):S219–S225
Cheng T, Chen D, Zhu C, Pan X, Mao X, Guo Y, Zhang X (2013) Fixed- versus mobile-bearing unicondylar knee arthroplasty: Are failure modes different? Knee Surg Sports Traumatol Arthrosc 21(11):2433–2441
Citak M, Cross MB, Gehrke T, Dersch K, Kendoff D (2015) Modes of failure and revision of failed lateral unicompartmental knee arthroplasties. Knee 22(4):338–340
Evans JD (1996) Straightforward statistics for the behavioral sciences. Brooks/Cole Publishing, Pacific Grove
Harrington IJ (1983) Static and dynamic loading patterns in knee joints with deformities. J Bone Joint Surg Am 65(2):247–259
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res 423:161–165
Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br 82(8):1196–1198
Insall J, Aglietti P (1980) A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am 62(8):1329–1337
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82(8):1189–1195
Kandil A, Werner BC, Gwathmey WF, Browne JA (2015) Obesity, morbid obesity and their related medical comorbidities are associated with increased complications and revision rates after unicompartmental knee arthroplasty. J Arthroplasty 30(3):456–460
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Khamaisy S, Gladnick BP, Nam D, Reinhardt KR, Heyse TJ, Pearle AD (2015) Lower limb alignment control: Is it more challenging in lateral compared to medial unicondylar knee arthroplasty? Knee 22(4):347–350
Kozinn SC, Marx C, Scott RD (1989) Unicompartmental knee arthroplasty. A 4.5–6-year follow-up study with a metal-backed tibial component. J Arthroplasty 4(Suppl):S1–S10
Kozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71(1):145–150
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17(1):48–52
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21(S1):S26–S32
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69(5):745–749
Murray DW, Pandit H, Weston-Simons JS, Jenkins C, Gill HS, Lombardi AV, Dodd CA, Berend KR (2013) Does body mass index affect the outcome of unicompartmental knee replacement? Knee 20(6):461–465
Nakagawa S, Kadoya Y, Todo S, Kobayashi A, Sakamoto H, Freeman MA, Yamano Y (2000) Tibiofemoral movement 3: full flexion in the living knee studied by MRI. J Bone Joint Surg Br 82(8):1199–1200
Ohdera T, Tokunaga J, Kobayashi A (2001) Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty 16(2):196–200
Pearle AD, O’Loughlin PF, Kendoff DO (2010) Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty 25(2):230–237
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2006) Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty 21(1):13–17
World Health Organization (1995) Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organization Technical Report, Series 854, pp 1–452
Roche M, O’Loughlin PF, Kendoff D, Musahl V, Pearle AD (2009) Robotic arm-assisted unicompartmental knee arthroplasty: preoperative planning and surgical technique. Am J Orthop (Belle Mead NJ) 38(2 Suppl):10–15
Sah AP, Scott RD (2007) Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Joint Surg Am 89(9):1948–1954
Scott RD (2005) Lateral unicompartmental replacement: a road less traveled. Orthopedics 28(9):983–984
Scott RD, Cobb AG, McQueary FG, Thornhill TS (1991) Unicompartmental knee arthroplasty: eight- to 12-year follow-up evaluation with survivorship analysis. Clin Orthop Relat Res 271:96–100
Sebilo A, Casin C, Lebel B, Rouvillain JL, Chapuis S, Bonnevialle P, members of the Societe d’Orthopedie et de Traumatologie de lO (2013) Clinical and technical factors influencing outcomes of unicompartmental knee arthroplasty: retrospective multicentre study of 944 knees. Orthop Traumatol Surg Res 99(4 Suppl):S227–S234
Servien E, Saffarini M, Lustig S, Chomel S, Neyret P (2008) Lateral versus medial tibial plateau: morphometric analysis and adaptability with current tibial component design. Knee Surg Sports Traumatol Arthrosc 16(12):1141–1145
Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286(2):188–195
Skytta ET, Haapamaki V, Koivikko M, Huhtala H, Remes V (2011) Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplasty. Acta Orthop Belg 77(3):329–335
Smith JR, Robinson JR, Porteous AJ, Murray JR, Hassaballa MA, Artz N, Newman JH (2014) Fixed bearing lateral unicompartmental knee arthroplasty-Short to midterm survivorship and knee scores for 101 prostheses. Knee 21(4):843–847
Specogna AV, Birmingham TB, DaSilva JJ, Milner JS, Kerr J, Hunt MA, Jones IC, Jenkyn TR, Fowler PJ, Giffin JR (2004) Reliability of lower limb frontal plane alignment measurements using plain radiographs and digitized images. J Knee Surg 17(4):203–210
Thompson SA, Liabaud B, Nellans KW, Geller JA (2013) Factors associated with poor outcomes following unicompartmental knee arthroplasty: redefining the “classic” indications for surgery. J Arthroplasty 28(9):1561–1564
Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Panni AS (2015) Minor varus alignment provides better results than neutral alignment in medial UKA. Knee 22(2):117–121
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH (2014) Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 21(1):180–184
Weidow J, Pak J, Karrholm J (2002) Different patterns of cartilage wear in medial and lateral gonarthrosis. Acta Orthop Scand 73(3):326–329
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
van der List, J.P., Chawla, H., Villa, J.C. et al. Early functional outcome after lateral UKA is sensitive to postoperative lower limb alignment. Knee Surg Sports Traumatol Arthrosc 25, 687–693 (2017). https://doi.org/10.1007/s00167-015-3877-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3877-0