Abstract
Purpose
The aim of this study was to assess the reliability of preoperative MRI for the staging of osteochondritis dissecans (OCD) lesions of the knee and the talus in juvenile patients, using arthroscopy as the gold standard of diagnosis.
Methods
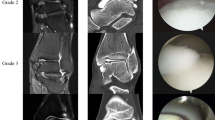
Sixty-three juvenile patients (range 8–16 years) with an OCD of the knee or the talus underwent arthroscopy after MRI. In 54/9 out of 63 cases, 1.5/3 T MR scanners were used. The OCD stage was classified according the staging criteria of Dipaola et al. Arthroscopic findings were compared with MRI reports in each patient.
Results
From the 63 juvenile patients, MRI/arthroscopy revealed a stage I OCD in 4/19 patients, stage II in 31/22 patients, stage III in 22/9 patients and stage IV in 6/6 patients. No osteochondral pathology was evident in arthroscopy in seven out of 63 patients. The overall accuracy of preoperative MRI in staging an OCD lesion of the knee or the talus was 41.3 %. In 33 out of 63 patients (52.4 %), arthroscopy revealed a lower OCD stage than in the preoperative MRI grading, and in four out of 63 cases (6.4 %), the intraoperative arthroscopic grading was worse than in preoperative MRI prior to surgery. The utilization of the 3 T MRI provided a correct diagnosis with 44.4 %.
Conclusions
Even with today’s modern MRI scanners, it is not possible to predict an accurate OCD stage in children. The children’s orthopaedist should not solely rely on the MRI when it comes to the decision to further conservative or surgical treatment of a juvenile OCD, but rather should take surgical therapy in consideration within persisting symptoms despite a low OCD stage provided by MRI.
Level of evidence
III.






Similar content being viewed by others
References
Aglietti P, Buzzi R, Bassi PB, Fioriti M (1994) Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy 10(3):286–291
Cahill BR, Berg BC (1983) 99 m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med 11(5):329–335
Chambers HG, Shea KG, Anderson AF et al (2012) American Academy of Orthopaedic Surgeons clinical practice guideline on: the diagnosis and treatment of osteochondritis dissecans. J Bone Joint Surg Am 94(14):1322–1324
Dipaola JD, Nelson DW, Colville MR (1991) Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 7(1):101–104
Guhl JF (1982) Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res 167:65–74
Hefti F, Beguiristain J, Krauspe R et al (1999) Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B 8(4):231–245
Heywood CS, Benke MT, Brindle K, Fine KM (2011) Correlation of magnetic resonance imaging to arthroscopic findings of stability in juvenile osteochondritis dissecans. Arthroscopy 27(2):194–199
Iwasaki N, Kamishima T, Kato H, Funakoshi T, Minami A (2012) A retrospective evaluation of magnetic resonance imaging effectiveness on capitellar osteochondritis dissecans among overhead athletes. Am J Sports Med 40(3):624–630
Jurgensen I, Bachmann G, Schleicher I, Haas H (2002) Arthroscopic versus conservative treatment of osteochondritis dissecans of the knee: value of magnetic resonance imaging in therapy planning and follow-up. Arthroscopy 18(4):378–386
Kijowski R, Blankenbaker DG, Shinki K, Fine JP, Graf BK, De Smet AA (2008) Juvenile versus adult osteochondritis dissecans of the knee: appropriate MR imaging criteria for instability. Radiology 248(2):571–578
Koch S, Kampen WU, Laprell H (1997) Cartilage and bone morphology in osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc 5(1):42–45
Kocher MS, DiCanzio J, Zurakowski D, Micheli LJ (2001) Diagnostic performance of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee disorders in children and adolescents. Am J Sports Med 29(3):292–296
Lefort G, Moyen B, Beaufils P et al (2006) Osteochondritis dissecans of the femoral condyles: report of 892 cases. Rev Chir Orthop Reparatrice Appar Mot 92(Suppl 5):2S97-92S141
Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M (2005) Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med 33(10):1499–1504
Mintz DN, Tashjian GS, Connell DA, Deland JT, O’Malley M, Potter HG (2003) Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy 19(4):353–359
Pascual-Garrido C, Moran CJ, Green DW, Cole BJ (2013) Osteochondritis dissecans of the knee in children and adolescents. Curr Opin Pediatr 25(1):46–51
Perumal V, Wall E, Babekir N (2007) Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop 27(7):821–825
Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM (2003) Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop 23(1):102–108
Quatman CE, Quatman-Yates CC, Schmitt LC, Paterno MV (2012) The clinical utility and diagnostic performance of MRI for identification and classification of knee osteochondritis dissecans. J Bone Joint Surg Am 94(11):1036–1044
Ragozzino A, Rossi G, Esposito S, Giovine S, Tuccillo M (1996) Computerized tomography of osteochondral diseases of the talus dome. Radiol Med 92(6):682–686
Robertson W, Kelly BT, Green DW (2003) Osteochondritis dissecans of the knee in children. Curr Opin Pediatr 15(1):38–44
Trinh TQ, Harris JD, Flanigan DC (2012) Surgical management of juvenile osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc 20(12):2419–2429
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Roßbach, B.P., Paulus, A.C., Niethammer, T.R. et al. Discrepancy between morphological findings in juvenile osteochondritis dissecans (OCD): a comparison of magnetic resonance imaging (MRI) and arthroscopy. Knee Surg Sports Traumatol Arthrosc 24, 1259–1264 (2016). https://doi.org/10.1007/s00167-015-3724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3724-3