Abstract
Early arthroplasty designs were associated with a high level of anterior knee pain as they failed to cater for the patello-femoral joint. Patellar resurfacing was heralded as the saviour safeguarding patient satisfaction and success but opinion on its necessity has since deeply divided the scientific community and has become synonymous to topics of religion or politics. Opponents of resurfacing contend that the native patella provides better patellar tracking, improved clinical function, and avoids implant-related complications, whilst proponents argue that patients have less pain, are overall more satisfied, and avert the need for secondary resurfacing. The question remains whether complications associated with patellar resurfacing including those arising from future component revision outweigh the somewhat increased incidence of anterior knee pain recorded in unresurfaced patients. The current scientific literature, which is often affected by methodological limitations and observer bias, remains confusing as it provides evidence in support of both sides of the argument, whilst blinded satisfaction studies comparing resurfaced and non-resurfaced knees generally reveal equivalent results. Even national arthroplasty register data show wide variations in the proportion of patellar resurfacing between countries that cannot be explained by cultural differences alone. Advocates who always resurface or never resurface indiscriminately expose the patella to a random choice. Selective resurfacing offers a compromise by providing a decision algorithm based on a propensity for improved clinical success, whilst avoiding potential complications associated with unnecessary resurfacing. Evidence regarding the validity of selection criteria, however, is missing, and the decision when to resurface is often based on intuitive reasoning. Our lack of understanding why, irrespective of pre-operative symptoms and patellar resurfacing, some patients may suffer pain following TKA and others may not have so far stifled our efforts to make the strategy of selective resurfacing succeed. We should hence devote our efforts in defining predictive criteria and indicators that will enable us to reliably identify those individuals who might benefit from a resurfacing procedure. Level of evidence V.
Similar content being viewed by others
Introduction
The patello-femoral articulation is exposed to the highest stresses within the locomotor system with recorded peak levels of up to 20 × body weight [123, 137, 155]. It is therefore not surprising that in 1977, Matthews et al. [86] expressed the view that ‘high patello-femoral load values, small patello-femoral contact areas, and resultant high stress magnitudes indicate the need for caution in the design and development of a patello-femoral component for total joint replacement prosthesis’. Their statement remains applicable even today, as retrieval analysis of patella components and the significant failure rate of metal-backed patella designs in the 1980s underscore the extreme mechanical environment in which these implants are expected to perform [8, 27, 59, 60, 116, 124, 144] (Fig. 1).
High patello-femoral reaction forces occur during knee flexion beyond 90°, when the patellar component leaves the trochlea groove, straddling the intercondylar notch, and contact areas decrease dramatically [124]
The earliest types of total knee arthroplasties were pure tibio-femoral replacements, primarily designed to treat severe axial deformities and intractable knee pain in patients affected by either tuberculosis or rheumatoid arthritis [47, 134, 150, 152]. They frankly ignored the patello-femoral joint, and associated patellar complications were often treated rather nonchalantly with patellectomy. Arthroplasty procedure at that time was seen as an alternative to arthrodesis and performed in patients of extremely low demand, where any improvement in pain relief or mobility level was considered a success [134, 152]. Increased patello-femoral complications and extensor mechanism failures raised awareness of the short comings of available knee implants failing to provide for normal patello-femoral function [63, 93, 131]. A case in point was the Duocondylar prosthesis which initially did not cater for the PFJ, providing disappointing results with a high level of patients suffering anterior knee discomfort [108]. Changes in femoral component design through the addition of a trochlear flange (Duopatellar design) improved clinical outcome dramatically by allowing the natural patella to articulate with the femoral component throughout the whole range of flexion [108, 109]. However, clinical results remained unpredictable and encouraged clinicians to experiment with replacement of the retro-patellar surface [2, 50, 51, 53, 54, 110]. In the 1980s, the patella was eventually removed from its Cinderella status and resurfacing was heralded as the saviour safeguarding patient satisfaction and success when replacing the knee. Amstutz even considered the term total knee arthroplasty a misnomer unless it incorporates the use of a patellar component [4]. Within a short period of time, patellar resurfacing was universally accepted as an integral part of total knee arthroplasty providing an improved level of patient satisfaction [65]. Over time, patellar resurfacing, however, became associated with complications specific to the patello-femoral joint which despite improvements in surgical technique and component design have not been eradicated (Fig. 2) [17, 68, 111, 113]. Omission of the patella on the other hand was seen to be responsible for an increase in the occurrence of anterior knee pain, which unfortunately failed in a large proportion of patients to respond to secondary resurfacing. The surgical community has hence become divided on the issue of how the patella is best served when performing total knee arthroplasty, and arguments for and against resurfacing have continued into the 21st century [1, 11, 18, 125, 128]. This article tries to address some of the questions surrounding the current controversy regarding patellar resurfacing and to balance the different points of view in an attempt to define what may be considered best medical practice.
Pros and cons of patella resurfacing
In 1836, Malgaigne of Paris wrote ‘When one searches among the past or present authors for the origins of doctrines generally accepted today concerning dislocation of the patella, one is surprised to find among them such disagreement and such a dearth of facts with such an abundance of opinions’ [82]. Although focussing on a slightly different subject matter, Malgaigne’s view very much characterises the diversity of opinions expressed in the debate about the value of patella resurfacing in TKA, which according to Krackow has become analogous to topics of religion and politics [71]. For Robertsson, “the usefulness (or not) of the patellar button is mostly a matter of ‘belief’, and opinion builders (surgeons and representatives) have a good opportunity to influence this” [120].
Three basic treatment strategies pertaining to the use of patellar components have evolved so far: always to resurface, never to resurface, or to selectively resurface the patella. Clinicians who prefer patellar resurfacing claim reduced incidence of post-operative anterior knee pain (AKP), avoidance of secondary resurfacing, higher patient satisfaction, better overall function, and a low complication rate [14, 75, 110, 130, 151]. They also argue that the procedure is relatively inexpensive and not time-consuming when performed during standard TKA. The articulation between cartilage and metal is considered unphysiological, and prolonged exposure to high compressive forces is believed to cause cartilage erosion [42]. So far, however, no conclusive evidence exists that patellae affected by such changes become symptomatic [69, 75, 141]. The proportion of revisions attributable to the resurfaced patella has dropped over the past 25 years from almost 50 % in the 1980s to around 12 % today [17, 66, 132]. The prevalence of patello-femoral complications has also decreased significantly and currently remains at around 4–5 % [7, 13, 73, 91, 156].
Clinicians in support of non-resurfacing argue that clinical results between patients with and without resurfacing are broadly similar and that patellar resurfacing therefore represents an unnecessary step in performing a TKA. Other claims pertain to conservation of patellar bone, reduced likelihood of patellar osteonecrosis, more physiological patello-femoral kinematics, ability to withstand high patello-femoral forces especially in younger and more active patients without the concern of prosthetic wear or failure, and ease of resurfacing in case of recalcitrant AKP [1, 23, 37, 69]. Particular emphasis is generally placed on the avoidance of intra- and post-operative complications associated with patellar resurfacing which have been reported in 4–35 % of cases, even when using contemporary total knee designs, and which include patella mal-tracking and sub-luxation, component wear and loosening, patella fracture, extensor mechanism failure, and AKP [8, 31, 32, 68, 113].
The paradigm of selective resurfacing attempts to identify those individuals who are thought to have an improved clinical outcome with patellar resurfacing whilst avoiding potential complications associated with unnecessary resurfacing [1, 17, 55, 69, 70, 76, 107, 128, 135, 141]. Advocates of selective patellar resurfacing have based their decision on the presence of certain prerequisites pertaining mainly to patient-related and prostheses-related factors. A number of patient selection criteria which favour patella retention have been suggested and include patients below the age of 65, absence of AKP or crystalline disease, reasonably well-preserved retro-patellar cartilage (e.g. viable cartilage without evidence of eburnised bone or Outerbridge grade IV changes), anatomical normality (e.g. adequate patello-femoral congruence, normally shaped patella of adequate thickness), and normal patellar mechanics (e.g. central patellar tracking). Survival rates of up to 97.5 % at 10 years in non-resurfaced total knee arthroplasties have been reported when these selection criteria are applied [70].
Some argument exists about the indication of patellar resurfacing in patients affected by inflammatory arthropathies. Sledge and Ewald suggested that failure to resurface the patella in rheumatoid arthritis may allow continued release of sequestered antigen from the retained cartilage resulting in recurrent inflammation [136]. Concerns about an ongoing inflammatory process, however, have remained largely theoretical, and although various studies have recommended routine resurfacing on all patients with RA [7, 76, 107, 127], others have failed to notice any ill effects despite patellar retention [1, 13, 30, 36, 55, 97, 135].
When resurfacing the patella, the surgeon is required to adhere to strict surgical principles in order to reproduce patellar thickness, preserve patellar blood supply, achieve appropriate positioning of all implant components, and balanced soft tissues to allow for central patellar tracking [71, 99, 122]. Prostheses-related factors are also critical to the success whether the patella remains resurfaced or not. The importance of femoral component design and its influence on patello-femoral performance has been highlighted by Theiss et al. [148] based on clinical results of two arthroplasty designs with distinct differences in trochlear geometry. A 14-fold decrease in patella-related complications was observed when using a patella-friendly design with an extended anterior flange, and a deeper and wider trochlea groove. The authors concluded that more proximal capture of the patella in a deeper groove with more gradual proximal-to-distal transition appeared advantageous in reducing patella morbidity. The group of Whiteside used an experimental model and was able to demonstrate that specific femoral design changes including deepening and distal extension of the trochlea groove improved patella tracking compared with an unmodified femoral component [158] (Fig. 3). The choice of prosthetic design with a patella-friendly femoral component has proven even more critical when the patella is left unresurfaced [12, 61, 81, 84, 85, 97, 147, 148]. Advocates of non-resurfacing hence favour femoral components of anatomically shaped trochlear configuration which attempt to provide a matching articulating surface to better accommodate the native patella.
Two femoral components demonstrating design changes to improve patellar function. Unmodified Ortholoc® femoral component with relatively patella unfriendly trochlea configuration (right) and modified Ortholoc® femoral component (left) with asymmetrical, anatomic femoral groove, elevated lateral trochlea flange, and elongated trochlea groove (Arthroplasty components courtesy of Leo Whiteside and associates from the Missouri Bone and Joint Research Foundation, St Louis/MO, USA)
Complications associated with patellar resurfacing
The advent of patellar resurfacing inadvertently introduced a new and different set of complications to the clinician performing TKA (Fig. 2). Failures associated with the PFJ are multifactorial and may relate to patient selection (e.g. age, BMI), surgical technique or implant design (e.g. dome, anatomic, mobile bearing) (Fig. 4) [111, 112]. The most common reason for patellar complications and premature patellar failure, however, is surgical mismanagement or misjudgement and the consequences thereof. Patellar complications include post-operative patellar mal-tracking and instability, patellar fracture, polyethylene wear, component loosening and dissociation, soft tissue impingement, and extensor mechanism disruption. Component design, material choice and the manufacturing process also appear to have a significant effect on performance, longevity and potential complications. Cases in point are the high failure rate associated with metal backing of patellar components and the use of carbon fibre re-enforced ultra-high molecular weight polyethylene (UHMWPE) in the 1980s and 1990s [78, 144]. More recently, awareness of the detrimental effects of prolonged shelf-life, problems arising through gamma sterilisation in air and post-sterilisation oxidation and degradation have been recognised and addressed through changes in the sterilisation process [28, 87, 114].
Commonly used types of patellar component design configurations [125]
Patellar fracture
Patella fractures following patellar resurfacing are generally rare, with reported figures ranging from 0.5 to 5.2 % [17, 48, 49, 90, 98, 116]. Although such fractures may result from trauma or from a complication during primary or revision surgery, the majority appear to occur spontaneously [65, 90, 129]. A compromise in patellar vascularity through medial arthrotomy combined with lateral retinacular release is thought to be a major factor in the aetiology of patellar fractures but its clinical significance remains unclear. Some series have demonstrated a relationship between avascularity and fracture [23, 64, 116], whilst others have failed to do so [41, 100, 115]. The literature conveys an array of other potential aetiological factors including technical errors (e.g. patellar mal-tracking secondary to implant mal-alignment, excessive or asymmetric patellar bone resection, thermal necrosis through cement polymerisation), patient demographics (e.g. male gender, obesity with BMI > 30 kg/m2, knee flexion beyond 95°, high activity level), and implant design (e.g. large patellar component ≥37 mm in diameter, inlay patellar design, large central fixation peg, posterior stabilising implant) [26, 34, 65, 80, 90, 98, 133, 149].
Patellar implant loosening
Loosening of the patellar component with or without displacement is reported to occur in 0.6–4.8 % of cases [17, 31, 90]. The frequency of patella component loosening has decreased significantly since the withdrawal of metal-backed patella components in the early 1990s which were notorious for developing wear and loosening [8, 78, 144]. Meding et al. [90] reviewed 8,531 total knee arthroplasties and recorded radiographic evidence of patella component loosening in 409 (4.8 %) cases at a mean of 7 years. In this series, obesity placed the patella at 6.3 times the risk of loosening, followed by lateral release at 3.8 times, elevated joint line at 2.2 times, and flexion beyond 100° at 2.1 times. Other factors identified included poor remaining bone stock, asymmetric patellar resection, small fixation pegs, inadequate implant fixation, patellar mal-tracking secondary to component mal-alignment, osteonecrosis and osteolysis [9, 79].
Patellar implant wear
Wear is a common feature in patellar implants due to the unfavourable mechanical environment of the patello-femoral articulation [27, 33, 60]. The in vivo wear pattern of patellar implants is highly dependent on the inherent mechanical properties of the materials used (e.g. polyethylene, methylemethacrylate bone cement), the interaction between patella and femoral component, and the external forces acting on them. The mechanical performance of the various designs is best assessed from observations made on retrieval components, which have shown considerable degree of wear and deformation (Fig. 5) [33, 40, 59, 89]. The level of wear damage appears to increase with patient’s weight, the post-operative range of motion, and the length of time the component has been implanted [40]. It is therefore of interest to note that despite patello-femoral compression forces exceeding the yield strength of UHMWPE, catastrophic wear or component fracture are seen infrequently and have not become a significant or endemic problem [146].
Patellar instability and dislocation
Patellar instability represents a serious problem in TKA and is responsible for a number of associated complications making it the most common reason for secondary surgery including revision [17, 24, 93]. The condition may occur in cases with and without patellar resurfacing, but is more commonly associated with the use of a patellar component. These patients often present with a plethora of symptoms, ranging from mild discomfort to pain, weakness, giving way and locking. Pavlou et al. [104] suggested patellar resurfacing in all cases where satisfactory soft tissue balance cannot be achieved, based on the ill-advised belief that resurfacing as such might overcome minor degrees of mal-tracking. The resurfaced patella, however, carries most probably a higher propensity to emphasise any mal-tracking, whilst the native patella offers at least a limited ability to adapt to adverse conditions over time [69].
The effect of implant design on patello-femoral stability is well recognised [143, 153]. Femoral components featuring a shallow and symmetric trochlea groove with abrupt changes in sagittal radius have been shown to create abnormal patellar kinematics and increase the risk of patellar mal-tracking [24, 106, 148, 158]. Campbell et al. [24] reviewed 289 knee arthroplasties with a shallow and narrow trochlea and found that out of 20 revisions 14 were required for patellar mal-tracking.
Surgical improprieties during patellar resurfacing are common reasons for patellar instability and include residual valgus limb mal-alignment, patella alta, increased internal rotation of femoral or tibial component, medial translation of the femoral component, excessive valgus alignment of the femoral component (even if the overall limb alignment appears neutral), asymmetric patellar resection, lateral placement of the patellar button, excessive patellar composite thickness, improper soft tissue balancing, and failure to perform a lateral release when required [16, 17, 24, 48, 92, 106, 112, 113].
The unresurfaced patella
Following bicompartmental knee arthroplasty, the non-resurfaced patella becomes exposed to the metallic surface of the femoral component (Fig. 6). Due to differences in modulus of elasticity, the articular surface of the patella must adapt to the geometry of the opposing surface by bedding in [69]. The process of biological remodelling, also described as ‘stress contouring’, produces a gradual adaptation of the retro-patellar surface and subchondral bone plate to the trochlea shape (Fig. 7) [140]. Keblish and Greenwald noted that minimal remodelling was required if the patella was exposed to an anatomical design with constant radius of curvature and uniform femoral geometry, whilst excessive remodelling was observed in non-anatomical designs [69]. The remodelling process was time dependent and not displayed through axial radiographs much before 2 years after implantation.
Tanzer et al. [147] looked at the effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in TKA. The authors noted substantial alterations in patello-femoral contact areas, contact pressures and tracking at higher flexion angles when the native patella was articulating with a prosthetic femoral component. Although the percentage of patello-femoral contact area compared with the native knee reduced markedly with increasing knee flexion, with measured values of 79 % at 60°, 69 % at 90° and 65 % at 105°, it remained well above those measured for the prosthetic patella.
The surface geometries of some prosthetic femoral components, particularly those of posterior stabilised design, appear incompatible with the native patella, as the apex of the retro-patellar ridge may impinge on the prosthetic intercondylar notch at knee flexion angles beyond 90° (Fig. 1). Patella deformation and wear are likely consequences, and in the case of significant patellar tilt, displacement of the patella into the notch becomes possible [88]. Distal extension of the trochlea and shortening of the intercondylar notch have been shown to safeguard patellar support beyond 90° of knee flexion [158] (Fig. 3). Such design modifications are hence important if one considers leaving the patella unresurfaced [81]. Most current femoral components, however, present a surface geometry designed to articulate with a designated patella component but are ill equipped to accommodate the native patella [81] (Figs. 6, 8). Specific efforts are required to improve patella kinematics by creating a femoral component which conforms to the normal trochlea and intercondylar notch topography and which takes the geometry of the native patella into account [154]. Only then would we be in a position to offer prostheses dedicated to articulate against the native patella, compared with the mostly inadequate femoral designs available to date.
Various femoral arthroplasty components with their respective, designated patellar implant. Top row, left to right: AGC® (dome patella), Biomet, Warsaw, USA; Buechel-Pappas (uncemented anatomic rotating platform patella), Endotec, Orlando, USA; LCS® (anatomical fixed bearing patella), DePuy, Warsaw, USA; Medial rotating knee® (cylindrical patella), Finsbury, England. Bottom row, left to right: Journey® (off-set dome patella), Smith and Nephew, Andover, USA; PFC-Sigma® (modified dome patella), DePuy; Triathlon® (off-set dome patella), Stryker, Kalamazoo, USA; BioPro® Townley Total Knee Original (uncemented metal-backed dome patella), Biopro, Port Huron, USA
Anterior knee pain in TKA
Early arthroplasty designs were particularly prone in causing post-operative AKP as they failed to provide an appropriately shaped articulating surface for the native patella [23, 64, 110, 141]. Despite advances in engineering, modern TKA designs continue to show a wide variations in the incidence of AKP, with reported figures of 0° to 47 % in patients with patellar resurfacing [13, 19, 25, 39, 151], and of 0° to 43 % in those patients where the patella is retained [13, 19, 38, 55, 67, 75, 97, 107, 151, 157]. These variations are likely to be due to differences in pain assessment, patient selection, surgical technique and implant design. Scott and Kim indicated that regardless of the management of the patella, clinicians can expect approximately 10% of patients to be affected by significant AKP after TKA, a finding, which has been confirmed through prospective, observational studies [5, 14, 35, 58, 130].
A significant number of clinical studies have shown that patients undergoing patella resurfacing are less likely to be affected by AKP and overall more satisfied [13, 23, 36, 67, 101, 126, 151]. However, the issue whether patients with non-resurfaced patellae really suffer more pain compared with those who have been resurfaced remains a controversial one. Robertsson et al. [117] reviewed data of 27,372 patients from the Swedish Knee Register and found that 15 % of patients with resurfaced patellae were generally dissatisfied, compared with 19 % where the patella had been retained. However, patients with patellar resurfacing became less satisfied with their knee over time, whilst satisfaction rating in those without resurfacing remained unchanged. The authors concluded that the benefit of the patellar component diminishes with time and that the need for secondary resurfacing may in the longer term be balanced by the need for revision of failed patellar components [117, 118]. A recent meta-analysis of 7,075 cases found no difference regarding the incidence of AKP between resurfacing and non-resurfacing group, which invited the authors to the conclusion that the rate of re-operations in non-resurfaced patients might be artificially increased as secondary resurfacing provides the only viable surgical option for this group of patients [104].
The great debate about the pros and cons of patellar resurfacing revolves around our lack of understanding why, irrespective of pre-operative symptoms and patellar resurfacing, some patients may suffer AKP following TKA and others may not [7, 105]. Even though many clinicians believe that in the presence of pre-operative symptoms resurfacing should be considered, the scientific basis for such action is missing, as no conclusive evidence currently exists. In a randomised controlled trial, Barrack et al. [7] found that 28 % of patients without AKP before resurfacing suffered AKP after surgery. Likewise, 9 % of patients with pre-operative AKP continued having pain post-operatively despite resurfacing. In the group where the patella was retained, 23 % continued suffering pain, whilst new pain developed in 14%. Hasegawa and Ohashi followed 78 unresurfaced TKAs for 12 years. Seventeen (22 %) knees developed patella subluxation and lateral facet erosion, but only four of these (5 %) experienced pain [55].
In many ways, it is erroneous to attribute all AKP to the patella, as a variety of conditions may be responsible for the development of discomfort projected in and around the patello-femoral articulation. Soft tissue afflictions (e.g. peri-patellar tendinopathy, bursitis, impinging synovial folds and scar tissue bands, neuromas, Sudeck dystrophy, complex regional pain syndrome), bony abnormalities (e.g. Sinding-Larson-Johansson syndrome, stress fracture, retained osteophytes, impinging loose bodies), and patellar mal-tracking have all been implicated as potential causes of AKP [18, 19, 124]. Any underlying condition should hence be addressed before treatment is focussed on the patello-femoral articulation.
Predictors of anterior knee pain
A variety of predictors for post-operative AKP have been suggested but few, like obesity and flexion contracture, have been reliably identified [57, 107, 139, 141]. Most clinical studies have failed to depict differences between knees affected by AKP and those which are not [7, 25, 139, 151]. Insall was unable to define a correlation between the degree of cartilage damage and the level of pain or quality of result in patients who had been left unresurfaced [63, 64, 141]. Elson and Brenkel prospectively assessed 602 primary TKAs and found mild pain in 8 % and moderate to severe pain in 5 % of knees [35]. In their study, age was the only reliable predictor of pain, with patients below the age of 60 being more than twice as likely to be affected. Results from randomised controlled trials have failed to show any association between obesity, pre-operative AKP, degree of chondromalacia or chondrolysis, lateral release and the occurrence of post-operative AKP [7, 25, 139]. Recently, height and weight but not BMI have been delineated as being predictive of anterior pain and of revision in resurfaced patellae, which is thought to be due to increased leaver arms and raised patello-femoral forces displayed in taller and heavier individuals [19, 90, 156]. Rodriguez-Merchán and Gómez-Cardero prospectively reviewed 500 patients without patellar resurfacing whose retro-patellar cartilage had been graded intra-operatively according to Outerbridge’s classification [121]. After a minimum follow-up of 5 years, 11.6 % of patients with grade IV changes required secondary resurfacing compared to 0.6 % of those with grade I–III. The authors concluded that patients with advanced levels of cartilage degradation should be resurfaced at index procedure. In comparison, Barrack et al. [7] found that neither obesity, nor the degree of patellar chondromalacia, or the presence of pre-operative anterior knee pain predicted post-operative clinical scores and the presence of post-operative AKP. Waters and Bentley assessed 514 knees randomised for patellar resurfacing and found no difference between knees with AKP and those without regarding age, weight, gender, lateral release, cruciate retention or sacrifice and whether the knees were affected by osteoarthritis or rheumatoid arthritis [151].
Despite resurfacing or non-resurfacing of the patella, the prevalence of AKP remains high. Combined with the fact that such pain often fails to respond to secondary resurfacing is suggestive that underlying patient, implant or surgical factors, other than patellar resurfacing, may have a significant impact on the presence of AKP following TKA [7, 39, 62]. Figgie et al. [39] were able to show that AKP was present in 23 of 75 TKAs in which the implants were positioned outside the ideal alignment compared with no cases of AKP in the group of 41 knees where components were positioned correctly.
Circumferential thermocoagulation of the patellar rim with electrocautery, which is thought to create a level of sensory deprivation, was first suggested by Keblish in 1991 in an attempt to reduce the likelihood of post-operative AKP when retaining the native patella [68, 69]. Keblish used the procedure in conjunction with debridement and occasionally added transcortical Pridie drilling to areas of cartilage loss. Overall, the scientific literature on the subject is sparse and potential merits of such surgical intervention whether used in conjunction with patellar resurfacing or not remain unclear [52, 77, 105].
Implant design is known to impart a major effect on patella kinematics and it is therefore not inconceivable that such an effect may influence the development of post-operative AKP [55, 106, 147, 158]. The majority of femoral components available today are designed to articulate with their designated patellar prosthesis (Fig. 8). Articulation between native patella and prosthetic femur may induce potential problems in terms of abnormal contact and tracking characteristics [72, 147, 148, 154]. It has hence been speculated that AKP in patients where the patella has been left unresurfaced may be secondary to altered patellar biomechanics and poor femoral component design [13, 84, 85, 140].
How important design issues are has been highlighted by a group of researchers from the University of Western Australia, who conducted two randomised controlled studies with almost identical study design where the only major variable was the type of prosthesis used. In the first study conducted by Wood et al. [156], a relatively unfriendly patellar design, featuring flat-shaped condyles with a shallow and angular trochlea groove was employed. In their second study led by Smith et al. [138], a relatively patellar-friendly design, characterised by a deepened trochlea groove with curved transition toward the femoral condyles was used. Comparing the outcome of non-resurfaced patients between both studies revealed a drop in the rate of post-operative AKP from 31 to 21 %, a reduction in the re-operation rate for patello-femoral complications from 12 to 1.2 %, and an increase in Knee Society Rating Score by 11 points. The group of Beverland examined 10-year data of 600 unresurfaced TKAs utilising an anatomically shaped ‘patella-friendly’ femoral component [97]. The authors found significant AKP leading to secondary resurfacing in only 1.5% of cases and concluded that leaving the patella unresurfaced does not adversely affect the outcome when using a patella-friendly design. Hwang et al. [61] who compared 7-year results of two groups of patients who received a femoral component with patella-friendly design features were unable to detect any significant differences in terms of AKP, or revision rate between resurfaced and unresurfaced knees. A recent review study failed to observe an association between clinical outcome and prosthetic design, but the inclusion criteria used in qualifying ‘patella-friendliness’ were somewhat indiscriminate, resulting in most implants falling into this category [104].
On the basis of our current knowledge, reported results from clinical studies should probably be viewed as being design specific and reliable only for the implant studied. Some older and often retrospective studies have featured implant designs which have either been altered or discontinued, hence substantially impairing their validity. However, despite proper patient and implant selection and good surgical technique, the inability to determine with any degree of certainty, whether a patient may be affected by AKP if the patella is left unresurfaced remains a surgical conundrum and demands further investigations.
Secondary resurfacing
The number of patella-related revisions is higher if the patella is left unresurfaced and is thought to reflect the higher incidence of AKP in patients with patellar retention. Insertion of a patella component or ‘secondary resurfacing’, considered a remedial procedure to address AKP, is performed in up to 13% of cases [7, 13, 36, 107, 141]. In 1998, Insall conveyed that in his series of several hundred TKAs (IB-II®, Zimmer, Warsaw, USA), which was not a particularly patellar-friendly femoral component design, the rate of secondary resurfacing was approximately 8% [66]. In a significant proportion of these patients, however, symptoms are likely to remain unchanged despite secondary resurfacing or revision arthroplasty [94]. Satisfactory outcomes following secondary resurfacing have been reported in 30% to 80% of cases [7, 24, 45, 72, 83, 94, 102, 117, 142]. However, even if the secondary resurfacing procedure appears successful at first, recurrence of symptoms has been reported in up to 55% of patients [7]. In a recent retrospective study, Parvizi et al. [102] reviewed 39 patients at an average of 4.5 years following secondary resurfacing for AKP and encountered 8 patients who expressed their dissatisfaction with the outcome of surgery. However, 14 patients showed no improvement or deterioration in clinical outcome and 7 patients required further revision, with one for mal-tracking of the patella.
Spencer et al. [142] reviewed 28 patients who had undergone secondary patellar resurfacing for persistent AKP. Patient satisfaction was assessed at a mean of 28 months post-operatively, resulting in 59 % feeling improved, 34 % feeling the same and 7 % feeling worse. In a similar study, Garcia, Kraay and Goldberg reviewed 17 cases of isolated patellar resurfacing, of which 53 % were asymptomatic and satisfied, whilst 47 % continued to be affected by AKP and unsatisfied [45]. It would hence appear reasonable to suggest that failure of patients to improve following secondary resurfacing may point to either a multifactorial aetiology or a different cause for pain other than a problem pertaining to the PFJ.
Three-phase bone scintigraphy as an assessment tool to distinguish patients who are likely to benefit from secondary resurfacing has recently been suggested [3]. Increased tracer uptake of the patella in patients with localised AKP appeared predictive of symptomatic pain relief following secondary patellar resurfacing, but overall numbers were small; hence, further research is needed before a principle may be established.
If a patient with a non-resurfaced patella presents with AKP, secondary resurfacing despite its limited success remains an available option and potential remedy. Conversely, there are fewer options available for the treatment of those patients with AKP whose patella has already been resurfaced. Isolated patella component revision for pain is generally not recommended as the clinical outcome is uncertain [10]. Furthermore, patella revision is far from being an innocuous procedure and should be approached with utmost caution as complications are frequent and outcomes poor [10, 74]. It could therefore be argued that if this clinical situation occurs where a patient is affected by AKP following primary patellar resurfacing, the surgeon is less likely to proceed with a revision procedure, which to some extent would explain the higher proportion of revisions in non-resurfaced knee arthroplasties.
Revisions for patello-femoral symptoms are mostly performed relatively soon after the index procedure, whilst revisions for wear or loosening of the patellar implant usually occur much later on. Putting this in perspective with the finding that patients who had their patella resurfaced are at least initially more satisfied with their knee, one might suggest a more liberal use of patellar resurfacing, at least in the elderly population [117, 118, 120].
National arthroplasty registers
National joint registers are a valuable source of information as it pools data on a large number of patients. Unfortunately, data collection is of variable quality and does not cover all aspects of treatment and complications surrounding the management of the PFJ in TKA [118]. The frequency of implanting a patellar component varies greatly between countries. The Swedish Knee Arthroplasty Register has provided long-term data on the use of patellar components in TKA since 1975 [145]. Following a peak in patellar resurfacing during the 1980s, with rates of over 70 %, there has been a steady decline in the number of TKA receiving a patellar component (Fig. 9). In the most recent report published in 2010, patella resurfacing as part of a TKA was performed in just over 3% of cases [145]. Although the register revealed a higher rate of revision in unresurfaced TKAs, the difference was not statistically significant.
In comparison, data from the 2009 arthroplasty register report in Norway indicated that out of a total of 3965 TKAs, only 96 (2.4 %) received a patellar component, whilst secondary resurfacing for AKP was performed in 1.8% of all arthroplasty cases [44, 96] (Fig. 10). According to the 2010 annual report of the Danish Knee Arthroplasty Register, it was estimated that the use of patellar resurfacing in TKA had increased from 68 % in 1997–2000 to 80 % in 2009 [29] (Fig. 10). The report further revealed that of all revision procedures performed in Denmark, 9.1 % are performed for secondary patellar resurfacing and 5.1 % for polyethylene wear of patellar components. Reported figures from the 2011 Annual Australian National Joint Replacement Registry Report confirmed an increase in the rate of resurfacing from 41.5 % in 2005 to 49.5 % in 2010 [6]. If the patella was left unresurfaced, the cumulative revision rate for posterior stabilised implants at 10 years was calculated at 8.1 %, compared with 5.8 % for all others. Patello-femoral pain was listed as the reason for revision in about 13.5 % of all primary TKAs. Interestingly, the Australian figures show significant variations in the usage of patella components between States and Territories.
Robertsson et al. [119] recently analysed 10-year data from the Nordic Arthroplasty Association obtained between 1997 and 2007. To the authors it remained unclear why the use of patellar components increased in Denmark but decreased in Norway and Sweden in the given time frame and why surgical practice in these counties differs so significantly (Fig. 10). It is unlikely that the variations in the proportion of resurfaced primary patellae between National joint registers can be attributable to cultural differences alone. It may hence be assumed that surgeon’s choices must have been affected by clinical evidence, experience, education, tradition and manufacturers marketing politics or a combination thereof [120].
Proportion of implants types used for primary knee arthroplasty in Denmark, Norway and Sweden. Blue column demonstrates the proportion of resurfaced patellae, and green column demonstrates the proportion of patellae which have been left unresurfaced. Please note the significant differences and trends regarding patella resurfacing between the three countries [119]. Courtesy of Otto Robertsson and with kind permission of Acta Orthopaedica)
Prospective and randomised controlled trials
Unilateral trials
The controversy surrounding the need for patellar resurfacing at the time of TKA has been fuelled by differing results derived from clinical studies and historic data. Unfortunately, most studies are retrospective and utilising redundant implant designs. They are often inadvertently affected by observer bias and their methodological limitations prevent a direct comparison of like-for-like. These studies have henceforth done little to reduce the insurmountable divide between clinicians who promote resurfacing and those who do not. Randomised, controlled, prospective trials have tried to address these shortcomings, but variations in patient assessment and study design remain and continue to impair their comparability.
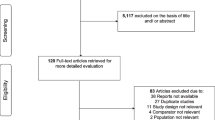
A meta-analysis of 16 randomised controlled trials (RCT) revealed a total of 1,587 knees which were treated with patellar resurfacing at the time of TKA, compared with 1,620 knees where the patella was left unresurfaced [7, 15, 19, 21, 25, 37, 38, 46, 77, 95, 101, 126, 139, 151, 156] (Table 1). The average follow-up period was 5.4 years (range 1–10.8 years). Post-operative AKP was present in 20.8 % of unresurfaced and 16.8% of resurfaced patellae. Knee Society scores of 155 in unresurfaced and 153 in resurfaced patellae were recorded. Patellar complications lead to a reoperation rate of 4.4 % in all unresurfaced and of 2.1 % in all resurfaced patellae. Overall, 9 studies were unable to define a clinically significant difference between resurfacing and non-resurfacing in patients’ function and their perception of pain, two studies showed slight preference towards non-resurfacing, whilst in five studies, resurfacing appeared superior over non-resurfacing.
Some of these studies have examined knee function in more detail by assessing the patient’s ability to climb stairs [19, 25, 37, 46, 139, 156]. Bourne et al. [11] who devised a 30s stair climbing test found no statistically significant difference at 2-year follow-up between patients with and without patellar resurfacing. The same group of patients was again reviewed at 10 years, by which time those with patella resurfacing climbed on average 20 stairs compared with 31 stairs in the non-resurfaced group, a difference which reached statistical significance [19]. Similar findings were reported by Feller et al. [37] who found that the stair climbing ability in the non-resurfaced patient group was significantly better compared with those with patella resurfacing. Two RCTs found no significant difference regarding the performance of functional tasks between resurfaced and non-resurfaced patients [46, 139], whilst two other RCTs showed a trend toward increased pain with stair ascend and descend, although values did not reach statistical significance [25, 156].
Two randomised controlled biomechanical studies looked at functional range of movement and walking gait pattern [95, 138]. Both studies were unable to delineate any clinically relevant differences between resurfaced and non-resurfaced knees, but highlighted discrepancies in kinematics compared with normal individuals.
Bilateral comparative trials
A total of 10 studies (prospective or randomised controlled) incorporating a comparative assessment of patients who received bilateral total knee arthroplasties, with patellar resurfacing performed on one side only, were identified [7, 20, 36, 69, 76, 103, 105, 135, 139, 151] (Table 2). A meta-analysis of these studies revealed a total of 299 patients, who had been followed-up between 2 and 10 years (average 5 years). Satisfaction was assessed by asking patients which knee they prefer. The resurfaced side was favoured by 35 % of all patients, the non-resurfaced side by 18 %, and 47 % expressed no preference for either knee.
Conclusion
The patella represents an integral part of any TKA and clinicians must be aware that the surgical management of the patella will not only affect patient satisfaction but occupies a pivotal role in success or failure of TKA. The appreciation of the consequences of the mechanical environment on the behaviour of the PFJ is of particular importance when contemplating patellar resurfacing. Clinicians should hence possess principle knowledge of anatomy, biomechanics and kinematics of the knee and the locomotor system, as surgically imposed changes may impart significant effects on performance and behaviour of the PFJ [123, 124]. In addition, awareness of the importance of proper component alignment and the effects of mal-positioning on the PFJ are paramount in achieving long-term success, regardless as to whether the patella is resurfaced or not. Surgical technique and implant design have been unequivocally identified as major factors in influencing clinical outcome, and their improvements have helped to reduce the incidence of AKP and patella-related complications.
The orthopaedic community, however, remains deeply divided regarding the issue of patellar resurfacing and the argument for or against continues to be unresolved. Opponents of resurfacing contend that the native patella provides better patellar tracking, improved clinical function, and avoids implant-related complications, whilst proponents of resurfacing argue that patients have less pain, are overall more satisfied, and avert the need for secondary resurfacing. Clinicians have to weigh the possible risk of secondary patella resurfacing for anterior pain against an increased probability of complications arising from patellar resurfacing and future component revision.
The scientific literature can be confusing as it offers as much evidence in support of routine resurfacing as in non-resurfacing. Recent evidence-based research and meta-analysis have failed to draw clear conclusions and therefore have been unable to provide clinicians with specific guidance [12, 22, 43, 56, 90, 104]. It is therefore not surprising that national arthroplasty register data show wide variations in the proportion of patellar resurfacing between countries, reasons for which cannot be accounted for by cultural differences alone and are likely to be multifactorial.
Available randomised controlled trials have so far only considered the ‘all-or-nothing’ approach of always or never to resurface, whilst ignoring ‘selective resurfacing’ as a possible treatment arm. The two standpoints of always to resurface or never to resurface, however, treat the patella indiscriminately based on a random choice. The paradigm of selective patellar resurfacing is attempting to identify those individuals who are thought to have an improved clinical outcome with patellar resurfacing whilst avoiding potential complications associated with unnecessary resurfacing. Selective resurfacing appears as a tempting proposition but evidence regarding the validity of selection criteria remains elusive and the decision when to resurface is often based on intuitive reasoning alone. It is therefore necessary that we define suitable indicators that will tell us who might benefit from a resurfacing procedure, in order to improve the reliability of the selection process. Our endeavours, however, remain hampered by a paucity of validated outcome measures as currently available assessment tools and scoring systems lack sensitivity to detect subtle differences in patello-femoral pain and function. Until we are able to obtain an unambiguous agreement on best practice on patella resurfacing, it may not be unreasonable to consider the compromise of selective resurfacing as middle ground between the two extreme views of always or never to resurface, or in the words of the Roman poet Ovid (43BC-18AD) “In medio tutissimus ibis”.
References
Abraham W, Buchanan JR, Daubert H, Greer RB III, Keefer J (1988) Should the patella be resurfaced in total knee arthroplasty? Efficacy of patellar resurfacing. Clin Orthop Relat Res 236:128–134
Aglietti P, Insall JN, Walker PS, Trent PS (1975) A new patella prosthesis: design and application. Clin Orthop Relat Res 107:175–187
Ahmad R, Kumar GS, Katam K, Pozo JL (2009) Significance of ‘hot patella’ in total knee replacement without primary patellar resurfacing. Knee 16:337–340
Amstutz HC, Finerman GAM (1973) Knee joint replacement-development and evaluation. Clin Orthop Relat Res 94:24–41
Anderson JG, Wixson RL, Tsai D, Stuhlberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11:831–840
Australian Arthroplasty register: http://www.dmac.adelaide.edu.au/aoanjrr/publications.jsp?section=reports2011
Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L (2001) Patellar resurfacing in total knee arthroplasty: A prospective randomised double blinded study with five to seven years of follow-up. J Bone Jt Surg 83-A:1376–1381
Bayley JC, Scott RD, Ewald FC, Holmes GB Jr (1988) Metal-backed patella component failure following total knee replacement. J Bone Jt Surg 70-A:668–674
Berend ME, Ritter MA, Keating EM, Faris PM, Crites BM (2001) The failure of all-polyethylene patellar components in total knee arthroplasty. Clin Orthop Relat Res 388:105–111
Berry DJ, Rand JA (1993) Isolated patellar component revision of total knee arthroplasty. Clin Orthop Relat Res 286:110–115
Bourne RB, Rorabeck CH, Vaz M, Kramer J, Hardie R, Robertson D (1995) Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res 321:156–161
Bourne RB, Burnett RSJ (2004) The consequences of not resurfacing the patella. Clin Orthop Relat Res 428:166–169
Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Jt Surg 75-A:674–681
Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, Houle T (2003) Predicting total knee replacement pain. A prospective, observational study. Clin Orthop Relat Res 416:27–36
Breeman S, Campbell M, Dakin H, Fiddian N, Fitzpatrick R, Grant A, Gray A, Johnston L, MacLennan G, Morris R, Murray D (2011) Patellar resurfacing in total knee replacement: five-year clinical and economic results of a large randomized controlled trial. J Bone Jt Surg 93-A:1473–1481
Briard J-L (1990) Patellar problems with total knee arthroplasty. In: Coombs RRH, Gristina AG, Hungerford DS (eds) Joint replacement. State of the art. Orthotext, London, pp 249–257
Brick GW, Scott RD (1988) The patellofemoral component of total knee arthroplasty. Clin Orthop Relat Res 231:163–178
Burnett RS, Bourne RB (2003) Indications for patellar resurfacing in total knee arthroplasty. Instructional course lecture. J Bone Jt Surg 85:728–745
Burnett RS, Haydon CM, Rorabeck CH, Bourne RB (2004) Patella resurfacing versus nonresurfacing in total knee arthroplasty. Clin Orthop Relat Res 428:12–25
Burnett RS, Boone JL, McCarthy KP, Rosenzweig SD, Barrack RL (2007) A prospective randomised clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res 464:65–72
Burnett RSJ, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL (2009) Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomised trial. J Bone Jt Surg 91-A:2562–2567
Calvisi V, Camillieri G, Luparelli S (2009) Resurfacing versus nonresurfacing the patella in total knee arthroplasty: a critical appraisal of the available evidence. Arch Orthop Trauma Surg 129:1261–1270
Cameron HU, Fedorkow DM (1982) The patella in total knee arthroplasty. Clin Orthop Relat Res 165:197–199
Campbell DG, Mintz AD, Stevenson TM (1995) Early patellofemoral revision following total knee arthroplasty. J Arthroplasty 10:287–291
Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM (2006) Patellar resurfacing in total knee arthroplasty: a ten year randomised prospective trial. J Bone Jt Surg 88-B:734–739
Clayton ML, Thirupathi R (1982) Patellar complications after total condylar arthroplasty. Clin Orthop Relat Res 170:152–155
Collier JP, McNamara JL, Suprenant VA, Jensen RE, Suprenant HP (1991) All-polyethylene components are not the answer. Clin Orthop Relat Res 273:198–203
Collier JP, Sperling DK, Currier JH, Sutula LC, Saum KA, Mayor MB (1996) Impact of gamma sterilisation on clinical performance of polyethylene in the knee. J Arthroplasty 11:377–389
Danish Arthroplasty Register (2010) http://www.knee.dk/groups/dkr/pdf/DKRreportEnglish2010.pdf
Deehan DJ, Phaltankar PM, Pinder IM (2008) Do we need to replace the patella in knee arthroplasty for rheumatoid disease? Acta Orthop Belg 74:478–482
Dennis DA (1997) Extensor mechanism problems in total knee arthroplasty. Instr Course Lect 46:171–180
Dennis DA (2001) Periprosthetic fractures following total knee arthroplasty. Instr Course Lect 50:379–389
DeSwart RJ, Stulberg BN, Gaisser DM, Reger SI (1989) Wear characteristics of all-polyethylene patellar components: a retrieval analysis. Trans Orthop Res Soc 14:367
Doolittle KH, Turner RH (1988) Patellofemoral problems following total knee arthroplasty. Orthop Rev 17:696–702
Elson DW, Brenkel IJ (2006) Predicting pain after total knee arthroplasty. J Arhroplasty 21:1048–1053
Enis JE, Gardner R, Robledo MA, Latta L, Smith R (1990) Comparison of patellar resurfacing versus nonresurfacing in bilateral total knee arthroplasty. Clin Orthop Relat Res 260:38–42
Feller JA, Bartlett RJ, Lang DM (1996) Patellar resurfacing versus retention in total knee arthroplasty. J Bone Jt Surg 78:226–228
Fengler H (2001) Patellaersatz—Ja oder nein? In: Eulert J, Hassenpflug J (eds) Praxis der Knieendoprothetik. Springer, Berlin, pp 149–157
Figgie HE III, Goldberg VM, Heiple KG, Moller HS III, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Jt Surg 68:1035–1040
Figgie MP, Wright TM, Santer T, Fisher D, Forbes A (1989) Performance of dome shaped patellar components in total knee arthroplasty. Trans Orthop Res Soc 14:367
Figgie HE III, Goldberg VM, Figgie MP, Inglis NE, Kelly M, Sobel M (1989) The effect of alignment of the implant in fractures of the patella after condylar total knee arthroplasty. J Bone Jt Surg 71-A:1031–1039
Forster H, Fisher J (1999) The influence of continuous sliding and subsequent surface wear on the friction of articular cartilage. Proc Inst Mech Eng 213:329–345
Fu Y, Wang G, Fu Q (2011) Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 19:1460–1466
Furnes O, Esqehaug B, Lie SA, Vollset SE, Engesæter LB, Havelin LI (2002) Early failures among 7,174 primary total knee replacements. A follow-up study from the Norwegian arthroplasty register 1994–2000. Acta Orthop Scand 73:117–129
Garcia RM, Kraay MJ, Goldberg VM (2009) Isolated resurfacing of the previously unresurfaced patella total knee arthroplasty. J Arthroplasty 25:754–758
Gildone A, Manfredini M, Biscione R, Faccini R (2005) Patellar resurfacing in posterior stabilised total knee arthroplasty: a follow-up study in 56 patients. Acta Orthop Belg 71:445–451
Gluck T (1891) Referat über die durch das modern chirurgische Experiment gewonnenen positive Resultate, betreffend die Naht und den Ersatz von Defecten höherer Gewebe, sowie über die Verwehrtung resorbirbarer und lebendiger Tampons in der Chirurgie. Langenbecks Arch Klin Chir 41:187–239
Goldberg VM, Figgie HE II, Inglis AE, Figgie MP, Sobel M, Kelly M, Kraay M (1988) Patellar fracture type and prognosis in condylar total knee arthroplasty. Clin Orthop Relat Res 236:115–122
Grace JN, Sim FH (1988) Patellar fracture complicating total knee arthroplasty. Complic Orthop 3:149–155
Groeneveld HB, Schöllner D, Bantjes A, Feijen J (1971) Eine Kniegelenkstotalendoprothese unter Erhalt der Kreuz- und Seitenbänder. [Total knee arthroplasty with preservation of cruciate and collateral ligaments]. Z Orthop 109:599–607
Groeneveld HB (1975) Total arthroplasty of the knee joint and the need for replacement of the patella. In: The medical engineering working party: total knee replacement. Mechanical Engineering Publications Limited, London, pp 50–51
Gupta S, Augustine A, Horey L, Meek RM, Hullin MG, Mohammed A (2010) Electrocautery of the patellar rim in primary total knee replacement: beneficial or unnecessary? J Bone Jt Surg 92:1259–1261
Hanslik L (1971) Das patellofemorale Gleitlager beim totalen Kniegelenksersatz. [The patello-femoral joint in total knee arthroplasty]. Z Orthop 109:435–440
Hanslik L (1973) First experience on knee joint replacement using the young hinged prosthesis combined with a modification on the McKeever patella prosthesis. Clin Orthop Relat Res 94:115–121
Hasegawa M, Ohashi T (2002) Long-term clinical results and radiographic changes in the nonresurfaced patella after total knee arthroplasty: 78 knees followed for mean 12 years. Acta Orthop Scand 73:539–545
He JY, Jiang LS, Dai LY (2011) Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee 18:137–144
Healy WL, Wasilewski SA, Takei R, Oberlander M (1995) Patellofemoral complications following total knee arthroplasty. J Arthroplasty 10:197–201
Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA (1998) Patient outcomes after knee replacement. Clin Orthop 356:93–110
Hood RW, Wright TM, Burstein AH (1983) Retrieval analysis of total knee prostheses: a methods and its application to 48 total condylar prostheses. J Biomed Mater Res 17:829–842
Hsu H-P, Walker PS (1989) Wear and deformation of patellar components in total knee arthroplasty. Clin Orthop Relat Res 246:260–265
Hwang B-H, Yang I-H, Han C-D (2012) Comparison of patellar retention versus resurfacing in LCS mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:524–531
Incavo SJ, Coughlin KM, Pappas C, Beynnon BD (2003) Anatomic rotational relationship of the proximal tibia, distal femur, and patella. J Arthroplasty 18:643–648
Insall JN, Ranawat CS, Aglietti P, Shine J (1976) A comparison of four models of total knee replacement prosthesis. J Bone Jt Surg 58-A:754–765
Insall JN, Scott WN, Ranawat CS (1979) The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Jt Surg 61:173–180
Insall JN, Lachiewicz PF, Burstein AH (1982) The posterior stabilised prosthesis. A modification of the total condylar design. A two to four year clinical experience. J Bone Jt Surg 64-A:1317–1323
Insall JN (1998) Personal communication
Kajiano A, Yoshino S, Kameyama S, Kohda M, Nagashima S (1997) Comparison of the results of bilateral total knee arthroplasty with and without patellar replacement for rheumatoid arthritis. J Bone Jt Surg 79-A:570–574
Keblish PA, Greenwald SA (1991) Patella retention vs patella resurfacing in total knee arthroplasty. The patella: the unresolved problem in TKA. Presented at the 41st annual meeting of the American academy of orthopaedic surgeons
Keblish PA, Varma AK, Greenwald SA (1994) Patellar resurfacing or retention in total knee arthroplasty: a prospective study of patients with bilateral replacement. J Bone Jt Surg 76:930–937
Kim BS, Reitman RD, Schai PA, Scott RD (1999) Selective patellar non-resurfacing in total knee arthroplasty. 10 year results. Clin Orthop Relat Res 367:81–88
Krackow KA (1990) The technique of total knee arthroplasty. Mosby, Saint Louis
Kulkarni SK, Freeman MAR, Pola-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? J Arthroplasty 15:424–429
Larson CM, Lachiewicz PF (1999) Patellofemoral complications with the Insall-Burstein II posterior stabilised total knee arthroplasty. J Arthroplasty 14:288–292
Leopold SS, Silverton CD, Barden RM, Rosenberg AG (2003) Isolated revision of patellar component in total knee arthroplasty. J Bone Jt Surg 85-A:41–47
Levani J-P, McLeod HC, Freeman MAR (1983) Why not resurface the patella? J Bone Jt Surg 65-B:448–451
Levitsky KA, Harris WJ, McManus J, Scott RD (1993) Total knee arthroplasty without patellar resurfacing. Clin Orthop Relat Res 286:116–121
Liu ZT, Fu PL, Wu HS, Zhu Y (2011) Patellar reshaping versus resurfacing in total knee arthroplasty—results of a randomized prospective trial at a minimum of 7 years’ follow-up. Knee. doi:10.1016/j.knee.2011.03.004
Lombardi AV, Engh GA, Volz RG, Albrigo JL, Brainard BJ (1988) Fracture/dissociation of the polyethylene in metal-backed patellar components in total knee arthroplasty. J Bone Jt Surg 70-A:675–679
Lonner JH, Lotke PA (1999) Aseptic complications after total knee arthroplasty. J Am Acad Orthop Surg 7:311–324
Lynch AF, Rorabeck CH, Bourne RB (1987) Extensor mechanism complications following total knee arthroplasty. J Arthroplasty 2:135–140
Ma HM, Lu YC, Kwok TG, Ho FY, Huang CY, Huang CH (2007) The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Jt Surg 89:408–412
Malgaigne JF (1836) Mémoire sur la détermination des diverses espéces de luxations de la rotule, leurs signes et leur traitement. Gaz Méd de Paris 43:673–678
Mannan K, Scott G (2009) The medial rotating total knee replacement. J Bone Jt Surg 91:750–756
Matsuda S, Ishinishi T, White SE, Whiteside LA (1997) Patellofemoral joint after total knee arthroplasty: effect on contact area and contact stress. J Arthroplasty 12:792–796
Matsuda S, Ishinishi T, Whiteside LA (2000) Contact stresses with an unresurfaced patella in total knee arthroplasty: the effect of femoral component design. Orthopedics 23:213–218
Matthews LS, Sonstegard DA, Henke JA (1977) Load bearing characteristics of the patello-femoral joint. Acta Orthop Scand 48:511–516
McGovern TF, Ammeen TJ, Collier JP, Currier BH, Engh GA (2002) Rapid polyethylene failure of unicondylar tibial components sterilised with gamma irradiation in air and implanted after a long shelf life. J Bone Jt Surg 84-A:901–906
McLain RF, Bargar WF (1986) The effect of total knee design on patellar strain. J Arthroplasty 1:91–98
McNamara JL, Collier JP, Mayor MB, Jensen RE (1994) A comparison of contact pressures in tibial and patellar total knee components before and after service in vivo. Clin Orthop Relat Res 299:104–113
Meding JB, Fish MD, Berend ME, Ritter MA, Keating EM (2008) Predicting patellar failure after total knee arthroplasty. Clin Orthop Relat Res 466:2769–2774
Meneghini RM (2008) Should the patella be resurfaced in primary total knee arthroplasty? An evidence-based analysis. J Arthroplasty 23(Suppl 1):11–14
Merkow RL, Soudry M, Insall JN (1985) Patella dislocation following total knee replacement. J Bone Jt Surg 67-A:1321–1327
Mochizuki RM, Schurman DJ (1979) Patella complications following total knee arthroplasty. J Bone Jt Surg 61-A:879–883
Mockford BJ, Beverland DE (2005) Secondary resurfacing of the patella in mobile-bearing total knee arthroplasty. J Arthroplasty 20:898–902
Myles CM, Rowe PJ, Nutton RW, Burnett R (2006) The effect of patella resurfacing in total knee arthroplasty on functional range of movement measured by flexible electrogoniometry. Clin Biomech 21:733–739
Norwegian Arthroplasty register (2010) www.haukeland.no/nrl/eng/default.htm
O’Brien S, Spence DJ, Ogonda LO, Beverland DE (2012) LCS mobile bearing total knee arthroplasty without patellar resurfacing. Does the unresurfacedpatella affect outcome? Survivorship at a minimum 10-year follow-up. Knee. doi:10.1016/j.knee.2011.07.002
Ortiguera CJ, Berry DJ (2002) Patellar fracture after total knee arthroplasty. J Bone Jt Surg 84-A:532–540
Pagnano MW, Kelly MA (2002) The intraoperative assessment of patellar tracking. In: Scuderi GR, Tria AJ Jr (eds) Surgical techniques in total knee arthroplasty. Springer, New York, pp 317–325
Pagnano MW (2003) Patellar tendon and quadriceps tendon tears after total knee arthroplasty. J Knee Surg 16:242–247
Partio E, Wirz D (1995) Comparison of patellar resurfacing and nonresurfacing in total knee arthroplasty: a prospective randomised study. J Orthop Rheumatol 8:69–74
Parvizi J, Mortazavi SM, Devulapalli C, Hozack WJ, Sharkey PF, Rothman RH (2012) Secondary resurfacing of the patella after primary total knee arthroplasty: does the anterior knee pain resolve? J Arthroplasty 27:21–26
Patel K, Raut V (2011) Patella in total knee arthroplasty: to resurface or not to—a cohort study of staged bilateral total knee arthroplasty. Int Orthop (SICOT) 35:349–353
Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E (2011) Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7,075 cases. J Bone Jt Surg 93-A:1301–1309
Peng CW, Tay BK, Lee BPH (2003) Prospective trial of resurfaced patella versus non-resurfaced patella in simultaneous bilateral total knee replacement. Singapore Med J 44:347–351
Petersilge WJ, Oishi CS, Kaufman KR, Irby SE, Colwell CW Jr (1994) The effect of trochlea design on patellofemoral shear and compressive forces in total knee arthroplasty. Clin Orthop Relat Res 309:124–130
Picetti GD, McGann WA, Welch RB (1990) The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Jt Surg 72-A:1379–1382
Ranawat CS, Insall JN, Shine J (1976) Duo-condylar knee arthroplasty. Hospital for special surgery design. Clin Orthop Relat Res 120:76–82
Ranawat CS, Sculco TP (1985) History and development of the total knee prosthesis at the Hospital of Special Surgery. In: Ranawat CS (ed) Total-condylar knee arthroplasty. Springer, New York, pp 3–6
Ranawat CS (1986) The patellofemoral joint in total condylar knee arthroplasty. Clin Orthop Relat Res 205:93–99
Rand JA (1994) Current concept review: the patello-femoral joint in total knee arthroplasty. J Bone Jt Surg 76:612–620
Rand JA (2004) Extensor mechanism complications following total knee arthroplasty. J Bone Jt Surg 86-A:2062–2072
Rand JA (2005) Failures in patellar replacement in total knee arthroplasty. In: Bellemans J, Ries MD, Victor JMK (eds) Total knee arthroplasty. Springer, Berlin, pp 57–64
Rimnac CM, Klein RW, Betts F, Wright TM (1994) Post-irradiation aging of ultra high molecular weight polyethylene. J Bone Jt Surg 76-A:1052–1056
Ritter MA (1990) Patellar problems with total knee replacement. In: Coombs RRH, Gristina AG, Hungerford DS (eds) Joint replacement. State of the art. Orthotext, London, pp 259–262
Ritter MA, Pierce MJ, Zhou H (1999) Patellar complications. Clin Orthop Relat Res 367:149–157
Robertsson O, Dunbar M, Phersson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71:262–267
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The Swedish knee arthroplasty register 1975–1997: an update with special emphasis on 41,223 knees operated on in 1988–1997. Acta Orthop Scand 72:503–513
Robertsson O, Bizjajeva S, Fenstad AM, Furnes O, Lidgren L, Mehnert F, Odgaard A, Pedersen AB, Havelin LI (2010) Knee arthroplasty in Denmark, Norway and Sweden. A pilot study from the Nordic Arthroplasty register Association. Acta Orthop 81:82–89
Robertsson O (2011) Personal communication
Rodriguez-Merchán E, Gómez-Cardero P (2010) The Outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res 468:1254–1257
Rosenberg AG (1993) Surgical technique of posterior cruciate sacrificing, and preserving total knee arthroplasty. In: Rand JA (ed) Total knee arthroplasty. Raven Press, New York, pp 115–153
Schindler OS, Scott WN (2011) Basic kinematics and biomechanics of the patello-femoral joint. Part I: the native patella. Acta Orthop Belg 77:421–431
Schindler OS (2012) Basic kinematics and biomechanics of the patello-femoral joint. Part II: the patella in total knee arthroplasty. Acta Orthop Belg 78:11–29
Schindler OS (2012) Patellar resurfacing in total knee arthroplasty. In: Scott WN (ed) Insall and Scott Surgery of the Knee, 5th edn. Elsevier, Churchill Livingstone, pp 1161–1190
Schroeder-Boersch H, Scheller G, Fischer J, Jani L (1998) Advantages of patellar resurfacing in total knee arthroplasty. Two year results of a prospective randomised study. Arch Orthop Trauma Surg 117:73–78
Scott RD (1979) Prosthetic replacement of the patellofemoral joint. Orthop Clin North Am 10:129–137
Scott RD, Reilly DT (1980) Pros and cons of patellar resurfacing in total knee replacement. Orthop Trans 4:328–329
Scott RD, Turoff N, Ewald FC (1982) Stress fracture of the patella following duopatellar total knee arthroplasty with patellar resurfacing. Clin Orthop Relat Res 170:147–151
Scott WN, Kim H (2000) Resurfacing the patella offers lower complication and revision rates. Orthopedics 24:24
Seedhom BB (1975) The patellar surface of femoral components. In: The medical engineering working party (ed) Total knee replacement. Mechanical Engineering Publications Limited, London, pp 176–178
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Sheth NP, Pedowitz DI, Lonner JH (2007) Current concepts review. Periprosthetic patellar fracture. J Bone Jt Surg 89-A:2285–2296
Shiers LGP (1975) Total knee hinge replacement. In: The Medical Engineering Working Party (ed) Total knee replacement. Mechanical Engineering Publications Limited, London, pp 44–49
Shoji H, Yoshino S, Kajino A (1989) Patellar replacement in bilateral total knee arthroplasty. J Bone Jt Surg 71-A:853–856
Sledge CB, Ewald FC (1979) Total knee arthroplasty experience at the Robert Breck Brigham Hospital. Clin Orthop Relat Res 145:78–84
Smith AJ (1972) A study of force on the body in athletic activities with particular reference to jumping. PhD thesis. England, Leeds. University of Leeds Library link: http://lib.leeds.ac.uk/record=b1472135
Smith AJ, Lloyd DG, Wood DJ (2006) A kinematic analysis of walking after total knee arthroplasty with and without patellar resurfacing. Clin Biochem 21:379–386
Smith AJ, Wood DJ, Li M-G (2008) Total knee replacement with and without patellar resurfacing: a prospective randomised trial using the profix total knee system. J Bone Jt Surg 90-B:43–49
Smith SR, Stuart P, Pinder IM (1989) Non-resurfaced patella in total knee arthroplasty. J Arthroplasty 4(Suppl):81–86
Soudry M, Mestriner LA, Binazzi R, Insall JN (1986) Total knee arthroplasty without patellar resurfacing. Clin Orthop Relat Res 205:166–170
Spencer SJ, Young D, Blyth MJ (2010) Secondary resurfacing of the patella in total knee arthroplasty. Knee 17:187–190
Steubben CM, Postak PD, Greenwald AS (1993) Mechanical characteristics of patello-femoral replacements. Presented at the 43rd annual meeting of the American academy of orthopaedic surgeons, San Francisco
Stulberg SD, Stulberg BN, Hamati Y, Tsao A (1988) Failure mechanism of metal-backed patellar components. Clin Orthop Relat Res 236:88–105
Swedish Knee Arthroplasty Register (2011) www.knee.nko.se/english/online/thePages/index.php
Takeuchi T, Lathi VK, Khan AM, Hayes WC (1995) Patellofemoral contact pressure exceed the compressive yield strength of UHMWPE in total knee arthroplasties. J Arthroplasty 10:363–368
Tanzer M, McLean CA, Laxer E, Casey J, Ahmed AM (2001) Effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in total knee arthroplasty. Canadian J Surg 44:127–133
Theiss SM, Kitziger KJ, Lotke PS, Lotke PA (1996) Component design affecting patellofemoral complications after total knee replacement. Clin Orthop Relat Res 326:183–187
Tria AJ, Harwood DA, Alicea JA, Cody RP (1994) Patellar fractures in posterior stabilised total knee arthroplasties. Clin Orthop Relat Res 299:131–139
Walldius B (1957) Arthroplasty of the knee joint using endoprosthesis. Acta Orthop Scand Suppl 24:1–112
Waters TS, Bentley G (2003) Patellar resurfacing in total knee arthroplasty. J Bone Jt Surg 85-A:212–217
Waugh TR, Smith RC, Orofino CF, Anzel SM (1973) Total knee replacement. Clin Orthop Relat Res 94:196–201
Whiteside LA, Kasselt MR, Haynes DW (1987) Varus-valgus and rotational stability in rotationally unconstrained total knee arthroplasty. Clin Orthop Relat Res 219:147–157
Whiteside LA, Nakamaura T (2003) Effect of femoral component design on unresurfaced patellas in knee arthroplasty. Clin Orthop Relat Res 410:189–198
Winter DA (1983) Moments of force and mechanical power in jogging. J Biomech 16:91–97
Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK (2002) Patellar resurfacing in total knee arthroplasty: a prospective randomised trial. J Bone Jt Surg 84-A:187–193
Yamamoto S, Nakata S, Kondoh Y (1989) A follow-up study of an uncemented knee replacement. The results of 312 knees using the Kodama-Yamamoto prosthesis. J Bone Jt Surg 71-A:505–508
Yoshii T, Whiteside LA, Anouchi YS (1992) The effect of patella button placement and femoral design on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 275:211–219
Acknowledgments
The author is indebted to W Norman Scott and Giles Scuderi of the Insall Scott Kelly Institute in New York and Arlen Hanssen of the Mayo Clinic in Rochester/MI for their inspiration and for inviting him to contribute to the new edition of ‘Insall & Scott Surgery of the Knee’. Special thanks go to Steve Burnett of Victoria/British Columbia, Doug Naudie of London/Ontario and Andrea Baldini of Florence/Italy for the many happy discussions on the merits of patellar resurfacing during the Knee Society Insall Travelling Fellowship, which often progressed into the small hours of the morning. Furthermore, gratitude is extended to Otto Robertsson of Sweden for conveying his wisdom on the topic of patellar resurfacing and for allowing the author to reproduce some illustrations and data from the Nordic arthroplasty register. Last but not least, the author would like to acknowledge the kindness of Lesley Greig and her team at the Medical Library at Southmead Hospital, Jenny Arnott of the Bristol University Library and the team at the Wellcome Library in London who always went the extra mile.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dedicated to the loving memory of my dear mother, Karin Christa Schindler-Rohr.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Schindler, O.S. The controversy of patellar resurfacing in total knee arthroplasty: Ibisne in medio tutissimus?. Knee Surg Sports Traumatol Arthrosc 20, 1227–1244 (2012). https://doi.org/10.1007/s00167-012-1985-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1985-7