Abstract
Purpose
The aim of this study was to assess the neurologic outcome following extracorporeal cardiopulmonary resuscitation (ECPR) in five European centers.
Methods
Retrospective database analysis of prospective observational cohorts of patients undergoing ECPR (January 2012–December 2016) was performed. The primary outcome was 3-month favorable neurologic outcome (FO), defined as the cerebral performance categories of 1–2. Survival to ICU discharge and the number of patients undergoing organ donation were secondary outcomes. A subgroup of patients with stringent selection criteria (i.e., age ≤ 65 years, witnessed bystander CPR, no major co-morbidity and ECMO implemented within 1 h from arrest) was also analyzed.
Results
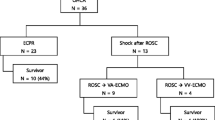
A total of 423 patients treated with ECPR were included (median age 57 [48–65] years; male gender 78%); ECPR was initiated for OHCA in 258 (61%) patients. Time from arrest to ECMO implementation was 65 [48–84] min. Eighty patients (19%) had favorable neurological outcome. ICU survival was 24% (n = 102); 23 (5%) non-survivors underwent organ donation procedures. Favorable neurological outcome rate was lower (9% vs. 34%, p < 0.01) in out-of-hospital than in-hospital cardiac arrest and was significantly associated with shorter time from collapse to ECMO. The application of stringent ECPR criteria (n = 105) resulted in 38% of patients with favorable neurologic outcome.
Conclusions
ECPR was associated with intact neurological recovery in 19% of unselected cardiac arrest victims, with 38% favorable outcome if stringent selection criteria would have been applied.



Similar content being viewed by others
References
Wong CX, Brown A, Lau DH et al (2019) Epidemiology of sudden cardiac death: global and regional perspectives. Heart Lung Circ 28(1):6–14
Bobrow BJ, Spaite DW, Berg RA et al (2010) Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA 304(13):1447–1454
Perkins GD, Handley AJ, Koster RW et al (2015) European resuscitation council guidelines for resuscitation 2015: section 2. adult basic life support and automated external defibrillation. Resuscitation 95:81–99
Reynolds JC, Grunau BE, Rittenberger JC et al (2016) Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation 134(25):2084–2094
Girotra S, Nallamothu BK, Spertus JA et al (2012) Trends in survival after in-hospital cardiac arrest. N Engl J Med 367(20):1912–1920
Reynolds JC, Frisch A, Rittenberger JC, Callaway CW (2013) Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation 128(23):2488–2494
Richardson AS, Schmidt M, Bailey M et al (2017) ECMO cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation 112:34–40
Sakamoto T, Morimura N, Nagao K et al (2014) Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation 85(6):762–768
Cardarelli MG, Young AJ, Griffith B (2009) Use of extracorporeal membrane oxygenation for adults in cardiac arrest (E-CPR): a meta-analysis of observational studies. ASAIO J 55(6):581–586
Kagawa E, Inoue I, Kawagoe T et al (2010) Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation 81(8):968–973
Chen Y-S, Chao A, Yu H-Y et al (2003) Analysis and results of prolonged resuscitation in cardiac arrest patients rescued by extracorporeal membrane oxygenation. J Am Coll Cardiol 41(2):197–203
Fagnoul D, Taccone FS, Belhaj A et al (2013) Extracorporeal life support associated with hypothermia and normoxemia in refractory cardiac arrest. Resuscitation 84(11):1519–1524
Brooks SC, Anderson ML, Bruder E et al (2015) Part 6: alternative techniques and ancillary devices for cardiopulmonary resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132(18 Suppl 2):S436–S443
Avalli L, Maggioni E, Formica F et al (2012) Favourable survival of in-hospital compared to out-of-hospital refractory cardiac arrest patients treated with extracorporeal membrane oxygenation: an Italian tertiary care centre experience. Resuscitation 83(5):579–583
Le Guen M, Nicolas-Robin A, Carreira S et al (2011) Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care 15(1):R29
Sandroni C, D’Arrigo S, Callaway CW et al (2016) The rate of brain death and organ donation in patients resuscitated from cardiac arrest: a systematic review and meta-analysis. Intensive Care Med 42(11):1661–1671
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22(7):707–710
Kellum JA, Lameire N; KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care 17(1):204
Henrion J (2012) Hypoxic hepatitis. Liver Int 32(7):1039–1052
Taylor FB, Toh CH, Hoots WK, Wada H, Levi M, Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH) (2001) Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost 86(5):1327–1330
Thuong M, Ruiz A, Evrard P et al (2016) New classification of donation after circulatory death donors definitions and terminology. Transpl Int 29(7):749–759
Hasegawa K, Tsugawa Y, Camargo CA Jr, Hiraide A, Brown DF (2013) Regional variability in survival outcomes of out-of-hospital cardiac arrest: the All-Japan Utstein Registry. Resuscitation 84(8):1099–1107
Berdowski J, Berg RA, Tijssen JG, Koster RW (2010) Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 81(11):1479–1487
Yannopoulos D, Bartos JA, Martin C et al (2016) Minnesota resuscitation consortium’s advanced perfusion and reperfusion cardiac life support strategy for out-of-hospital refractory ventricular fibrillation. J Am Heart Assoc 5:6
Bougouin W, Dumas F, Lamhaut L et al (2019) Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. https://doi.org/10.1093/eurheartj/ehz753
D’Arrigo S, Cacciola S, Dennis M et al (2017) Predictors of favourable outcome after in-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation 121:62–70
Debaty G, Babaz V, Durand M et al (2017) Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 112:1–10
Grunau B, Reynolds J, Scheuermeyer F et al (2016) Relationship between time-to-ROSC and survival in out-of-hospital cardiac arrest ECPR candidates: when is the best time to consider transport to hospital? Prehosp Emerg Care 20(5):615–622
Taccone FS, Crippa IA, Dell’Anna AM, Scolletta S (2015) Neuroprotective strategies and neuroprognostication after cardiac arrest. Best Pract Res Clin Anaesthesiol 29(4):451–464
Sandroni C, Dell’anna AM, Tujjar O, Geri G, Cariou A, Taccone FS (2016) Acute kidney injury after cardiac arrest: a systematic review and meta-analysis of clinical studies. Miner Anestesiol 82(9):989–999
Nobile L, Taccone FS, Szakmany T et al (2016) The impact of extracerebral organ failure on outcome of patients after cardiac arrest: an observational study from the ICON database. Crit Care 20(1):368
Roberts BW, Kilgannon JH, Chansky ME et al (2013) Multiple organ dysfunction after return of spontaneous circulation in postcardiac arrest syndrome. Crit Care Med 41(6):1492–1501
Iesu E, Franchi F, Zama Cavicchi F et al (2018) Acute liver dysfunction after cardiac arrest. PLoS One 13(11):e0206655
Lee DS, Chung CR, Jeon K et al (2016) Survival after extracorporeal cardiopulmonary resuscitation on weekends in comparison with weekdays. Ann Thorac Surg 101(1):133–140
Lie SA, Hwang NC (2019) Challenges of brain death and apnea testing in adult patients on extracorporeal membrane oxygenation—a review. J Cardiothorac Vasc Anesth 33(8):2266–2272
Efendijev I, Folger D, Raj R et al (2018) Outcomes and healthcare-associated costs one year after intensive care-treated cardiac arrest. Resuscitation 131:128–134
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
FST, MB, FP, LMB, and MW conceived the study protocol; FST, LMB, FP, MB, DL, and MW participated in the design and coordination of the study; LC, EC, AMS, DP, and AP collected study data; JC, MB, FP, LMB, and MW supervised data collection; FST, DL, LMB, FP, MW, JC, and DP participated in data interpretation; LC, EC, AMS, and AP were responsible for the literature search; FST, LMB, FP, MB, JC, DL, and MW drafted the present manuscript; LC, EC, AMS, DP, and AP revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
MB, LMB, FST, and FP received honoraria from Eurosets (Medolla, Italy). The other authors have no conflict of interest to disclose.
Ethical approval
Ethical approval was obtained by the Ethics Committee of each participating center. Hôpital Erasme: P2017/263—Fondazione IRCCS Policlinico San Matteo: Prot 3RIA2 2016)—University Hospital Regensburg: 17-426-160—San Raffaele Hospital: Prot OUT IMP 17072013—Karolinska Institutet: 2016/2447-31/4.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lunz, D., Calabrò, L., Belliato, M. et al. Extracorporeal membrane oxygenation for refractory cardiac arrest: a retrospective multicenter study. Intensive Care Med 46, 973–982 (2020). https://doi.org/10.1007/s00134-020-05926-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-05926-6