Abstract
Introduction
Extracorporeal carbon dioxide removal (ECCO2R) has been proposed for hypercapnic respiratory failure in chronic obstructive pulmonary disease (COPD) exacerbations, to avoid intubation or reduce length of invasive ventilation. Balance of risks, efficacy, and benefits of ECCO2R in patients with COPD is unclear.
Methods
We systematically searched MEDLINE and EMBASE to identify all publications reporting use of ECCO2R in COPD. We looked at physiological and clinical efficacy. A favorable outcome was defined as prevention of intubation or successful extubation. Major and minor complications were compiled.
Results
We identified 3123 citations. Ten studies (87 patients), primarily case series, met inclusion criteria. ECCO2R prevented intubation in 65/70 (93 %) patients and assisted in the successful extubation of 9/17 (53 %) mechanically ventilated subjects. One case–control study matching to noninvasively ventilated controls reported lower intubation rates and hospital mortality with ECCO2R that trended toward significance. Physiological data comparing pre- to post-ECCO2R changes suggest improvements for pH (0.07–0.15 higher), PaCO2 (25 mmHg lower), and respiratory rate (7 breaths/min lower), but not PaO2/FiO2. Studies reported 11 major (eight bleeds requiring blood transfusion of 2 units, and three line-related complications, including one death related to retroperitoneal bleeding) and 30 minor complications (13 bleeds, five related to anticoagulation, and nine clotting-related device malfunctions resulting in two emergent intubations).
Conclusion
The technique is still experimental and no randomized trial is available. Recognizing selection bias associated with case series, there still appears to be potential for benefit of ECCO2R in patients with COPD exacerbations. However, it is associated with frequent and potentially severe complications. Higher-quality studies are required to better elucidate this risk–benefit balance.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a major, worldwide health burden. It is currently the fourth leading cause of death and will likely become the third leading cause of death worldwide by 2030 [1]. The chronic and progressive nature of COPD is commonly aggravated by exacerbations. Each exacerbation reflects disease progression, decreased quality of life, and an increased risk of death [2–4]. Classically, respiratory failure in COPD has been managed with noninvasive ventilation (NIV) [5], and NIV compared to invasive mechanical ventilation has been demonstrated to reduce mortality by almost half [6]. However, approximately one-quarter to one-half of these patients will fail NIV and require invasive mechanical ventilation (IMV) [7, 8]. The need for IMV heralds a poor prognosis for COPD exacerbations with in-hospital survival rates that range from 30 to 75 % [9, 10]. The subset of patients who require IMV are also at increased risk of failed weaning and prolonged ventilation [10, 11].
Extracorporeal carbon dioxide removal (ECCO2R) devices have been proposed as an adjunct in patients with both hypoxic and hypercapnic respiratory failure. ECCO2R, as an experimental adjunct to mechanical ventilation in patients with hypercapnic acute respiratory failure secondary to COPD exacerbations, has been utilized to avoid intubation or reduce the length of invasive ventilation. The technology is not new; it was first used in patients by Gattinoni in the 1980s [12, 13], but has not achieved wide clinical use in part because of a high rate of complications. The general principle consists of an extracorporeal circuit similar to a continuous veno-venous hemofiltration circuit but with a membrane allowing the elimination of carbon dioxide (CO2) from the blood. In comparison with veno-venous extracorporeal membrane oxygenation (ECMO) (allowing blood oxygenation in addition to CO2 removal), much lower blood flows are required with ECCO2R (300–1500 mL/min vs 3–5 L/min for ECMO), which allow the use of smaller vascular cannulas (ca. 14–18 Fr). However, as a result of the high risk of clotting, anticoagulation is needed. The risks and benefits of ECCO2R in patients with COPD exacerbations are yet to be fully elucidated.
The majority of ECCO2R literature describes its use in acute respiratory distress syndrome (ARDS) to allow very small tidal volume (“ultra-protective ventilation”) [14–18]. In this situation, ECCO2R counteracts hypercapnia induced by very low minute ventilation. Limited studies have examined its efficacy and safety in hypercapnic respiratory failure secondary to COPD exacerbations. Therefore, we undertook a systematic review to identify all the publications reporting the use of ECCO2R devices in patients with exacerbations of COPD to determine the efficacy and safety of these devices in this disease.
Methods
Design
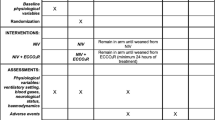
We conducted a systematic review with prespecified selection and outcome criteria. No review protocol was separately published. We systematically searched multiple sources to identify all the publications reporting the use of ECCO2R devices in patients with exacerbations of COPD. We searched the electronic databases Medline and Embase for articles and abstracts published before August 2014 using the following keywords: ECCOR, ECCO2R, CO2 removal, and extracorporeal. We also searched the bibliographies of included studies and review articles. We included articles published online at that time or published later in print. We searched the Clinical Trials Registry Database (http://clinicaltrials.gov) for registered unpublished and ongoing studies related to ECCO2R and COPD. No language restrictions were applied. We included a study or a case report if at least 1 adult (over 18 years) patient with COPD was treated using ECCO2R. Our primary outcomes of interest were the occurrence of a favorable outcome defined as the prevention of intubation in patients receiving NIV, or successful extubation when the device was implemented after intubation. Secondary clinical outcomes included ICU and hospital mortality and length of stay. Complications were classified as follows: major (death or life-threatening conditions in the absence of treatment, directly related to a device complication; transfusion of at least 2 units of packed red cells; or the need for open surgery) or minor (bleeding requiring less than 2 units of packed red cells; transient thrombocytopenia (at most 90 × 109/L) without clinical consequence; or non-life-threatening event related to catheter insertion). Physiological outcomes included changes in the respiratory parameters, including pH, arterial partial pressure of carbon dioxide (PaCO2) in mmHg, respiratory rate (RR) in breaths per minute; and changes in PaO2/FiO2 (the fraction of inspired oxygen) in mmHg as a measure of oxygenation.
Study selection
Two authors (MS and FB) independently reviewed the retrieved abstracts and assessed eligibility. Full-text review was conducted when either of the reviewers of the abstracts felt that the citations might meet inclusion criteria. Disagreement was resolved by consensus with a third author (LB).
Data extraction
Data from included studies were independently extracted by MS, FB, CK, and JF. We extracted the following data: study design, study and participant characteristics, study device, mode of extracorporeal access, device type, mode of ventilator support, study intervention, relevant outcome data, duration of ECCO2R use, and complications. All included studies were assessed for bias using the Cochrane Collaboration risk of bias tool [19].
Data analysis
Because most of the retrieved studies were case reports and case series without control patients, the proportion of ECCO2R patients with favorable clinical outcomes (prevention of intubation or successful extubation) and with complications were described but not pooled. Similarly the secondary clinical outcomes, ICU and hospital mortalities and lengths of stay, were also not pooled. Changes in physiological outcomes (pH, PaCO2, RR, PaO2/FiO2) comparing pre-initiation values separately to values at 1, 6, and 24 h after initiation of ECCO2R were pooled by calculating the differences in values for each physiological outcome for individual patients before and after ECCO2R, when available, and then calculating the means and standard deviations of these differences. When only group means and standard deviations were available for pre- and post-ECCO2R values, the difference was calculated and the standard deviation of the difference in means was calculated assuming a correlation (ρ) of 0.6. This was based on calculated ρ values ranging between 0.5 and 0.7 in the studies that provided individual patient pre- and post-ECCO2R values. Sensitivity analyses using both a high degree of correlation (ρ = 0.9) and no correlation (ρ = 0) resulted in no significant changes for any of the analyses. Medians and interquartile ranges [20] or ranges [21] were converted to means and standard deviations using previously published methods, where necessary [20]. Trial results were pooled using the generic inverse variance weighting method in Review Manager (RevMan version 5.2; Cochrane Collaboration, Oxford, UK) with a two-sided significance level of 5 %. Individual trial and summary results are reported with 95 % confidence intervals (CIs). Random effects models which incorporate between-trial heterogeneity and give wider and more conservative CIs when heterogeneity is present were used for all analyses [22]. Statistical heterogeneity among trials was assessed using the I 2 statistic, defined as the percentage of total variability across studies attributable to heterogeneity rather than chance, and using published guidelines for low (I 2 = 25–49 %), moderate (I 2 = 50–74 %), and high (I 2 ≥ 75 %) heterogeneity [23]. Z tests of interaction were used to calculate interaction p values comparing pooled changes from pre-ECCO2R between later and earlier times after ECCO2R initiation (i.e., comparing the changes from pre-ECCO2R at 6 vs 1 h, and 24 vs 6 h).
Results
Search results
Our search strategy identified 3123 citations. Of these, 2085 were removed from the analysis for not meeting screening eligibility. Thirty-eight studies were extracted for full-text analysis, of which ten studies met inclusion criteria and were subsequently analyzed in detail (Supplementary Fig. 1).
Pending and/or ongoing clinical studies
We identified five ongoing studies related to ECCO2R and COPD [24–28] on clinicaltrials.gov. A planned randomized controlled trial by Barrett [24] (target N = 24) will assess the time to cessation of NIV with the use of ECCO2R as an adjunct to NIV in acute exacerbations of COPD. Nava has two ongoing prospective cohort studies, one of which will attempt to facilitate weaning in mechanically ventilated hypercapnic respiratory failure patients with the use of carbon dioxide removal [25] (target N = 15), while the other will facilitate reduction in PaCO2 in stable COPD patients with chronic hypercapnic respiratory failure not responding to chronic NIV [26] (target N = 15). The ongoing prospective cohort ECLAIR study will use ECCO2R to prevent intubation in patients with acute hypercapnic respiratory failure failing NIV [27] (target N = 30). Finally, the PALP-COPD randomized controlled trial (target N = 120) aims to facilitate extubation of patients with COPD exacerbations with the aid of ECCO2R [28].
Characteristics of included studies
In total, ten studies reporting on 87 patients were included in this systematic review (Table 1). This included three single-patient case reports, two of which used ECCO2R in patients on NIV to avoid intubation [29, 30] and one in a mechanically ventilated patient to facilitate extubation [31]; four case series reporting on five invasively ventilated patients [32] and five [33], two [34], and six [35] patients receiving NIV, respectively. It also included three larger studies. One was a 20-patient case series that included seven patients on NIV at high likelihood of requiring mechanical ventilation, and two patients on NIV and 11 patients already on IMV who failed previous weaning attempts [36]. The other two were case control studies that compared 25 prospective ECCO2R-treated NIV patients with 21 matched NIV historical control patients [37]; and 21 retrospective ECCO2R-treated NIV patients from four centers with 21 matched control patients treated in one of the four centers over the same time period who had failed NIV and required mechanical ventilation [38].
Table 2 describes the device characteristics and the anticoagulation targets, when described. All studies implemented a pump-driven veno-venous ECCO2R device except the study by Kluge [38] that used the pumpless arteriovenous Novalung iLA device. Blood flow parameters varied significantly among the studies, ranging from several hundred milliliters per minute to several liters per minute. Vascular cannulas ranged from 13 to 23 Fr, though many used a 15.5-Fr catheter with the Hemolung device. Anticoagulation targets were measured either by the activated partial thromboplastin time test (aPTT) or the activated clotting time test (ACT). Intravenous unfractionated heparin was used for anticoagulation.
Inclusion and exclusion criteria for ECCO2R
Inclusion and exclusion criteria for ECCO2R were documented in four studies: Del Sorbo [37], Kluge [38], Burki [36], and Abrams [32] (Table 3). In general, the indications for ECCO2R included hypercapnic respiratory failure with clinical and laboratory evidence of worsening acid–base and respiratory parameters. Contraindications were more heterogeneous but included bleeding diathesis, thrombocytopenia, and inability to cannulate a central vein or central nervous system pathology.
Risk of bias
Since none of the studies meeting inclusion criteria were randomized controlled trials, the risk of bias of all studies was high with the exception of the Del Sorbo [37] trial which we graded as moderate (Supplemental Table 1).
Effect of interventions
Primary outcome
Eight studies presented data on intubation prevention [29, 30, 33–38] (Table 1). Seventy patients were included in the analysis on intubation prevention with an overall success rate of 65/70 (92.8 %) (Supplemental Fig. 3). The two case reports [29, 30] and three small case series [33–35] all reported a perfect success rate of preventing intubation when patients were placed on ECCO2R, as did the larger case series of Burki et al. [36]. In the study by Kluge et al. [38], 2/21 (10 %) ECCO2R-treated NIV patients required IMV, compared to 21/21 (100 %) of the control patients. Finally, in the case–control study by Del Sorbo et al. [37], only 3/25 patients (12 %, 95 % CI 3–31 %) in the NIV + ECCO2R group required intubation [due to device clotting (n = 2) or hemodynamic instability from retroperitoneal bleeding (n = 1)] vs 7/21 (33 %, 95 % CI 15–57 %) in the matched NIV-only group (HR 0.27, 95 % CI 0.07–0.98, p = 0.047).
ECCO2R was utilized in 17 patients receiving IMV across one case report [31], one case series (n = 5) [32], and 11 patients from the Burki study [36]. The rate of successful extubation in this cohort was 9/17 (52.9 %) (Supplemental Fig. 2). The single patient in the case report and all five patients in the small case series were successfully extubated following the implementation of ECCO2R, but Burki’s study successfully extubated only 3/11 (27 %).
Secondary clinical outcomes
Secondary clinical outcomes include ICU and hospital mortality and length of stay. Three studies presented data on mortality. Del Sorbo et al. [37]. found significantly reduced hospital mortality in patients receiving ECCO2R compared to controls (8 % in the ECCO2R group vs 35 % in the NIV alone group, p = 0.035). The case series by Abrams et al. [32] demonstrated a 100 % survival rate both to ICU discharge and hospital discharge in their uncontrolled series of five patients. Finally, Kluge et al. [38], in their two retrospectively compared groups, showed no significant difference in mortality at 28 days (19 % with ECCO2R vs 24 % without ECCO2R) or 6 months (both groups 33 %).
These same three studies presented length of stay data. Del Sorbo et al. [37] found nonsignificant differences in either ICU [8 (7, 10) vs 12 (6, 15); p = 0.19] or hospital length of stay [24 (21, 28) vs 22 (13, 36); p = 0.80] in their study groups (data presented as median (interquartile range), ECCO2R vs no ECCO2R). Similarly, Kluge et al. [38] found no differences in either median ICU or hospital length of stay in their ECCO2R vs invasive ventilation groups (15 vs 30 days and 23 vs 42 days, respectively). Abrams et al.’s [32] case series reported an average ± standard deviation ICU length of stay of 10.2 ± 2.5 days and a hospital length of stay of 15.6 ± 8.6 days.
Respiratory parameters
Compared to baseline, initiation of ECCO2R very quickly and significantly improved pH (Fig. 1a and Supplemental Fig. 4a), PaCO2 (Fig. 1b, Supplemental Fig. 4b), and RR (Fig. 1c, Supplemental Fig. 4c), even after the first hour; pH increased by 0.07 (95 % CI 0.06–0.09, p < 0.001; three studies [34, 37, 38], 48 patients) after 1 h, 0.11 (95 % CI 0.10–0.11, p < 0.001; three studies [34, 36, 38], 29 patients) after 6 h, and 0.15 (95 % CI 0.10–0.20, p < 0.001; four studies [32, 34, 36, 38], 33 patients) after 24 h. There was no between-study heterogeneity in the 1-h and 6-h comparisons (I 2 = 0 %), but a high degree of heterogeneity in the 24-h comparison (I 2 = 93 %). The greater increase between 1 and 6 h was statistically significant (interaction p = 0.0005) but the increase between 6 and 24 h did not achieve statistical significance (interaction p = 0.06). PaCO2 decreased around 25 mmHg similarly between 1 and 6 h, and between 6 and 24 h (interaction p > 0.05) with moderate to high heterogeneity in the 1-h and 24-h comparisons (I 2 = 55 and 77 %, respectively) (Fig. 1b). Few studies reported RR (only one study reported 6-h and 24-h data). Decreases of around 6–8 breaths per min were similar at all time points (interaction p ≥ 0.05) with high between study heterogeneity at 1 h (I 2 = 93 %), the only comparison with data from more than one study. PaO2/FiO2 was reported only in single studies at 1 h [37] and 24 h [38], thereby precluding pooling, and was not significantly changed by ECCO2R (Fig. 1d; Supplemental Fig. 4d).
Physiological parameters, data expressed as mean ± SD. a pH Overall change in pH was 0.07–0.15 increase; p < 0.00001, *p < 0.001 at each time measurement vs pre-ECCO2R; p = 0.005 for interaction 1 vs 6 h, p = 0.06 for interaction 6 h vs 1 day. b Overall decrease in PaCO2 was 24–26 mmHg vs pre-ECCO2R, p ≤ 0.0009. c Overall change in respiratory rate was 6–8 breaths/min lower vs pre-ECCO2R, p ≤ 0.008. d No significant change in PaO2/FiO2 1 h or 1 day vs pre-ECCO2R
Only one study compared physiological values in patients treated with ECCO2R to matched controls. This matched case–control study reported statistically significant improvements at 1 h in pH by 0.06 (p = 0.0003), PaCO2 by 17 mmHg (p = 0.01), and RR by 5 breaths/min (p = 0.0002), and a worsening in PaO2/FiO2 by 57 mmHg (p = 0.0006) [37].
Complications
All but two studies [30, 35] reported on ECCO2R-related complications (these two case reports did not report any information on complications). We found a total of 11 major and 30 minor complications in the included studies (Table 1; Fig. 2). Of the major complications, 8/11 (72.7 %) (Table 1) were clinically significant bleeding episodes requiring at least 2 units of packed red cells (with one patient requiring endotracheal intubation due to hemodynamic instability from retroperitoneal bleeding). The three remaining major complications consisted of one venous perforation at the catheter insertion site, one pneumothorax, and one death related to a retroperitoneal bleed secondary to perforation of an iliac vein.
Of the 30 minor complications (Table 1) we found 13 minor bleeding episodes related either to device insertion or due to systemic anticoagulation. There were four episodes of transient thrombocytopenia and one occurrence of heparin-induced thrombocytopenia. There was one reported deep venous thrombosis, one femoral artery pseudoaneurysm, and one episode of transient systemic hypotension. Nine complications were related to device malfunction in the form of circuit clotting (n = 6), pump malfunction (n = 2), and membrane failure (n = 1), two of which resulted in emergent intubations.
Discussion
This exhaustive systematic review evaluated the efficacy and safety of the experimental use of ECCO2R in 87 patients with hypercapnic respiratory failure across ten studies, primarily from cases series and case reports [29–36], and two studies which matched patients treated with ECCO2R to historical controls [37, 38]. The overall level of evidence of the studies included is of relatively low quality, but this review still provides an estimate of ECCO2R-related physiological changes and complications. The majority of patients in this review were either successfully weaned from mechanical ventilation or sustained on NIV, avoiding intubation. These high success rates, however, must be interpreted very cautiously given the clear selection bias associated with case series data.
The data presented in the included studies were quite heterogeneous. Outside our primary outcome, only three studies presented data on ICU and hospital length of stay and mortality. The available physiological data, comparing primarily pre- to post-ECCO2R changes in the same patients, suggest rapid and sustained improvements in ventilatory parameters including pH, PaCO2, and respiratory rate, but not in oxygenation as measured using PaO2/FiO2. On the basis of limited data, pH continued to improve between 1 and 24 h post initiation, whereas PaCO2 and respiratory rate did not show significant further improvements after 1 h. If this finding based on limited data is accurate, this suggests that the improvement in pH between 1 and 24 h may be attributable to improvements in metabolic rather than respiratory acidosis which could be due to factors such as improved circulation (reducing possible elevated lactate) or administration of diuretics or buffers (e.g., citrate loading from massive blood transfusions). Unfortunately, the included studies did not provide enough additional data to test these hypotheses. It should be noted that these changes in physiological outcomes over time did not account for other ventilatory changes made by clinicians in response to the early improvements observed with ECCO2R initiation, as these were generally not provided in the study reports.
The technical characteristics of ECCO2R have potential advantages over ECMO, but these foreseeable gains may give rise to significant harm. A recent editorial by Brochard [39] highlights this controversy. The major advantage of ECCO2R compared to ECMO is the considerably lower blood flow required: several hundred milliliters per minute vs several liters per minute for ECMO. The lower flow allows for the use of vascular cannulas similar in size to those used in continuous veno-venous hemofiltration (approximately 14–18 Fr, depending on device, in ECCO2R vs upwards of 20 Fr in ECMO). However one risk of the low flow ECCO2R system is the risk of membrane and circuit clotting related to low flow and thus the need for therapeutic anticoagulation.
Eight of the ten included studies reported on complications. The types and rates of complications again varied across the studies and there were substantially more observed complications in the larger clinical trials (32 out of 41 total recorded complications), with only nine recorded in the case report and smaller case series. Almost half of the patients in this systematic review experienced an ECCO2R-related complication (41/87, 47.1 %). About half of the total complications (21/41, 51.2 %) were bleeding episodes related to anticoagulation; eight were severe hemorrhagic events while 13 were minor bleeds. Retroperitoneal bleeding following femoral cannulation led to one death [36], while another patient required intubation due to resulting hemodynamic instability [37]. Several studies in our review reported no hemorrhagic complications [30, 31, 34, 35], which highlights the small sample sizes and differing protocols in the current body of literature.
Despite full anticoagulation we found nine thrombotic complications related to device failure. As we have previously noted [39], membrane clotting or device failure during ECCO2R can be a life-threatening event, which may lead to a rapid rise in carbon dioxide and overwhelming respiratory acidosis necessitating prompt intubation of patients and/or significant changes to their respiratory support. Only in the Del Sorbo study [37] was there mention of two patients requiring intubation in the setting of decompensation secondary to membrane clotting. It is evident by the propensity for both hemorrhagic and thrombotic events that the optimal anticoagulation scheme that minimizes both of the above is yet to be fully elucidated.
The risks related specifically to central line insertion, including pneumothorax, venous perforation, accidental arterial puncture, aneurysm, hematoma formation, and infection occurred rarely in this review and this limited body of literature is insufficient to ascertain if there is an increased risk of these with ECCO2R-sized cannulas. They do not seem low, however, compared to usual complication rates of central venous access or hemodialysis access [40, 41].
In several ECCO2R studies the intravascular devices and blood flow rates are comparable to those used for continuous renal replacement therapies (CRRT). One of the ongoing studies utilizes a modified continuous veno-venous hemofiltration system to provide ECCO2R [26]. This suggests that these techniques may demonstrate similar complication rates. Direct comparison of complication rates, however, is difficult because one must consider not only technical characteristics of the system but the underlying pathobiology of the patient. The types and rates of complications among CRRT studies vary but a recent review sheds some light [42]. This group’s experience with 1809 patients found a total complication rate of 46 %. The authors found a bleeding rate of 2.3 %, thrombosis rate of 2.5 %, and 15 episodes (0.8 %) of pneumothorax. Accidental arterial puncture occurred 5.7 % of the time and there was an infection rate of 17.2 %. There was no mention of dialysis membrane or circuit failures. These authors do not comment on blood flows, cannula sizes, or anticoagulation doses. Although a similar overall complication rate was seen in this large review of CRRT when compared to our review of ECCO2R, the distribution of complications is different and the relative contribution of circuit/system complications remains unknown.
Other sources of heterogeneity include the types of ECCO2R devices, the anticoagulation schemes, sizes of the vascular cannulas, and one study [38] that used an arterio-venous pumpless system. How these factors affect the rates of hemorrhage or thrombosis and other complication risks is not known, strengthening the need for higher-quality studies.
Limitations
Although we used rigorous systematic review and meta-analytic methods including a reproducible and comprehensive literature search strategy, clearly defined inclusion criteria, and duplicate citation review, data abstraction, and quality assessment of individual studies, a protocol for our systematic protocol was not pre-published. In addition, we identified only low-level evidence, primarily case series data. These types of reports are at high risk of selection bias since unsuccessful case reports or series are generally not published. As a result of a lack of control groups for clinical outcomes, we were limited to pooling before–after physiological outcomes, recognizing that surrogate outcomes typically overestimate benefits in clinical outcomes [43]. In particular, the reported rates of intubation prevention and earlier extubation are likely optimistic estimates. Despite these significant limitations, this review describes and highlights the paucity of data in this field and provides practitioners with a description of how this technique has been implemented, summarizing the complications that have occurred and the changes in physiological outcomes that may be expected.
Conclusion
ECCO2R is a fascinating technology that holds theoretical promise for the treatment of hypercapnic respiratory failure in the setting of COPD exacerbations. The current body of literature demonstrates that there is a paucity of high-quality data. It suggests, however, that this experimental technology may be highly efficient from a physiological standpoint but is also not without risk; in addition to the risk associated with central line insertion, there is a delicate balance between hemorrhage and thrombosis. This analysis strongly supports the need for further research with physiological and safety studies, including randomized controlled trials to more clearly elucidate the risk–benefit balance of ECCO2R in COPD exacerbations.
References
Decramer M, Janssens W, Miravitlles M (2012) Chronic obstructive pulmonary disease. Lancet 379:1341–1351
Soler-Cataluña JJ, Martínez-García MÁ, Sánchez PR et al (2005) Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 60:925–931
Connors AF, Dawson NV, Thomas C et al (1996) Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med 154:959–967
Hoogendoorn M, Hoogenveen RT, Rutten-van Mölken MP et al (2011) Case fatality of COPD exacerbations: a meta-analysis and statistical modelling approach. Eur Respir J 37:508–515
Chandra D, Stamm JA, Taylor B et al (2012) Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med 185:152–159
Brochard L, Mancebo J, Wysocki M et al (1995) Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 333:817–822
Quinnell TG, Pilsworth S, Shneerson JM, Smith IE (2006) Prolonged invasive ventilation following acute ventilatory failure in COPD: weaning results, survival, and the role of noninvasive ventilation. Chest 129:133–139
Hoo GW, Hakimian N, Santiago SM (2000) Hypercapnic respiratory failure in COPD patients: response to therapy. Chest 117:169–177
Chu CM, Chan VL, Lin AWN et al (2004) Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax 59:1020–1025
Menzies R, Gibbons W, Goldberg P (1989) Determinants of weaning and survival among patients with COPD who require mechanical ventilation for acute respiratory failure. Chest 95:398–405
Schönhofer B, Euteneuer S, Nava S et al (2002) Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med 28:908–916
Gattinoni L, Agostoni A, Pesenti A (1980) Treatment of acute respiratory failure with low-frequency positive-pressure ventilation and extracorporeal removal of CO2. Lancet 2:292–294
Gattinoni L, Pesenti A, Mascheroni D et al (1986) Low-frequency positive-pressure ventilation with extracorporeal CO2 removal in severe acute respiratory failure. JAMA 256:881–886
Terragni PP, Del Sorbo L, Mascia L et al (2009) Tidal volume lower than 6 mL/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology 111:826–835
Bein T, Weber-Carstens S, Goldmann A et al (2013) Lower tidal volume strategy (≈3 ml/kg) combined with extracorporeal CO2 removal versus conventional protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med 39:847–856
Bein T, Weber F, Philipp A et al (2006) A new pumpless extracorporeal interventional lung assist in critical hypoxemia/hypercapnia. Crit Care Med 34:1372–1377
Nierhaus A, Frings D, Braune S et al (2011) Interventional lung assist enables lung protective mechanical ventilation in acute respiratory distress syndrome. Minerva Anestesiol 77:797–801
Fitzgerald M, Millar J, Blackwood B et al (2014) Extracorporeal carbon dioxide removal for patients with acute respiratory failure secondary to the acute respiratory distress syndrome: a systematic review. Crit Care 18:222
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions. Wiley, USA
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Barrett N, Camporota L, Hart N (2014) ECCO2R as an adjunct to NIV in AECOPD. http://ClinicalTrials.gov. NCT02086084
Nava S (2014) Weaning form mechanical ventilation using extracorporeal CO2 removal (WeanPRO). http://ClinicalTrials.gov. NCT02259335
Nava S (2014) Effect of extracorporeal CO2 removal in stable hypercapnic COPD patients. http://Clinicaltrials.gov. NCT02260583
Kluge S (2013) Extracorporeal lung assist to avoid intubation in patients failing noninvasive ventilation for acute hypercapnic respiratory Failure (ECLAIR). http://Clinicaltrials.gov. NCT01784367
Ranieri VM (2014) The PALP™-COPD trial (Low-flow CO2-removal (ECCO2-R) in exacerbated COPD) (PALP-COPD). http://Clinicaltrials.gov. NCT02107222
Bonin F, Sommerwerck U, Lund LW, Teschler H (2013) Avoidance of intubation during acute exacerbation of chronic obstructive pulmonary disease for a lung transplant candidate using extracorporeal carbon dioxide removal with the Hemolung. J Thorac Cardiovasc Surg 145:e43–e44
Crotti S, Lissoni A, Tubiolo D et al (2012) Artificial lung as an alternative to mechanical ventilation in COPD exacerbation. Eur Respir J 39:212–215
Cardenas VJ Jr, Lynch JE, Ates R et al (2009) Venovenous carbon dioxide removal in chronic obstructive pulmonary disease experience in one patient. ASAIO J 55:420–422
Abrams DC, Brenner K, Burkart KM et al (2013) Pilot study of extracorporeal carbon dioxide removal to facilitate extubation and ambulation in exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc 10:307–314
Burki N, Mani R, Herth F, Schmidt W, Teschler H, Bonin F (2011) A novel extracorporeal CO2 removal system: application of the hemolung in patients with hypercapnic respiratory failure. Am J Respir Crit Care Med 183:A1697
Mani RK, Schmidt W, Lund LW, Herth FJF (2013) Respiratory dialysis for avoidance of intubation in acute exacerbation of COPD. ASAIO J 59:675–678
Spinelli E, Crotti S, Zacchetti L et al (2013) Effect of extracorporeal CO2 removal on respiratory rate in spontaneously breathing patients with chronic obstructive pulmonary disease exacerbation. Crit Care 17:S48
Burki NK, Mani RK, Herth FJF et al (2013) A novel extracorporeal CO(2) removal system: results of a pilot study of hypercapnic respiratory failure in patients with COPD. Chest 143:678–686
Del Sorbo L, Pisani L, Filippini C et al (2014) Extracorporeal CO2 Removal in hypercapnic patients at risk of noninvasive ventilation failure: a matched cohort study with historical control. Crit Care Med 43:120–127
Kluge S, Braune SA, Engel M et al (2012) Avoiding invasive mechanical ventilation by extracorporeal carbon dioxide removal in patients failing noninvasive ventilation. Intensive Care Med 38:1632–1639
Beloncle F, Brochard L (2015) Extracorporeal CO2 removal for chronic obstructive pulmonary disease: too risky or ready for a trial? Crit Care Med 43:245–246
Roux D, Reignier J, Thiery G et al (2014) Acquiring procedural skills in ICUs: a prospective multicenter study. Crit Care Med 42:886–895
Ruesch S, Walder B, Tramèr MR (2002) Complications of central venous catheters: internal jugular versus subclavian access–a systematic review. Crit Care Med 30:454–460
Bambauer R, Latza R (2004) Complications in large-bore catheters for extracorporeal detoxification methods. Artif Organs 28:629–633
Ciani O, Buyse M, Garside R et al (2013) Comparison of treatment effect sizes associated with surrogate and final patient relevant outcomes in randomised controlled trials: meta-epidemiological study. BMJ 346:f457
Conflicts of interest
No author identifies a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sklar, M.C., Beloncle, F., Katsios, C.M. et al. Extracorporeal carbon dioxide removal in patients with chronic obstructive pulmonary disease: a systematic review. Intensive Care Med 41, 1752–1762 (2015). https://doi.org/10.1007/s00134-015-3921-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3921-z