Abstract
Purpose
Left ventricular (LV) diastolic function is often impaired in critically ill septic patients. The peak velocity of the mitral annulus early wave during diastole (E′), measured by Doppler echocardiography, is a major tool to evaluate LV relaxation, the ATP-dependent part of diastole. The authors hypothesized that if volume expansion (VE) is followed by an increase in stroke volume (SV) (“adequate” VE), LV relaxation and consequently E′ may be increased.
Methods
This was a prospective study in which 83 mechanically ventilated septic patients with circulatory failure were enrolled. Doppler echocardiography was performed before and after the infusion of 500 ml of saline over 20 min. Patients were then classified into two groups according to their response to VE: responders (R) were those in whom SV increased by at least 15 %; all others were considered to be non-responders (NR). SV, mitral flow early wave velocity (E), E′ and the E/E′ ratio were measured before and after VE. VE-induced variations (∆) in all parameters were compared in R and NR. Patients with an E′ < 0.12 m/s were considered to have LV diastolic dysfunction.
Results
Fifty-nine patients (71 %) were R and 24 (29 %) were NR. Fifty-six percent of R patients and 58 % of NR patients had LV diastolic dysfunction. For patients with LV diastolic dysfunction (n = 47), ∆E′ was significantly higher in the R group (29 ± 5 vs. 5 ± 8 %; p = 0.01) whilst ∆E/E′ was higher in the NR group (35 ± 9 vs. 2 ± 6 %; p = 0.02).
Conclusions
E′ maximal velocity increased with adequate VE, suggesting an improvement of LV relaxation with the correction of hypovolaemia in patients with septic shock.
Similar content being viewed by others
Introduction
Diastolic function is of crucial importance in the intensive care setting [1]. Several studies have recently suggested that impaired diastolic function is a predictive factor of mortality in patients with septic shock [2]. Other studies have demonstrated that septic shock could be responsible for impaired left ventricular (LV) relaxation [3]. Impairment of diastolic function could lead to heart failure, pulmonary oedema or difficult weaning from ventilator support [1]. Doppler echocardiography is a major tool for the bedside evaluation of diastolic function [4]. The peak velocity of the mitral annulus early wave during disatole (E′), as assessed by tissue Doppler imaging, has recently been described and is considered to be an index of relaxation, i.e. the energy-dependent part of diastole, independent of loading conditions [5, 6]. During circulatory failure, volume expansion (VE) is often performed to enhance stroke volume (SV) and improve organ perfusion. We hypothesized that impaired LV relaxation during septic shock could be (at least partially) reversed by VE: if SV increases with VE, myocardial perfusion would therefore be enhanced [7], and relaxation could be increased with a limited increase in filling pressures. The aim of this study was to determine the impact of rapid VE on LV relaxation (assessed by E′ wave velocity) based on the effect of VE on SV, especially in patients with LV diastolic dysfunction.
Methods
Patients
This study was conducted in the 16-bed surgical and medical intensive care unit of the Amiens University Hospital over a 2-year period. The study was approved by the local institutional review board (CEERNI, Amiens, France), and informed consent was not required. Eligible patients were those on mechanical ventilation with circulatory failure due to sepsis for whom the physician decided to perform VE. Circulatory failure was defined as systolic blood pressure (SBP) <90 mmHg and/or persistent lactic acidosis and/or need for vasoactive drugs. The exclusion criteria were: age of <18 years, pregnancy, absence of sinus rhythm, right or left bundle branch block, known mitral or aortic valve disease, clinical signs of haemorrhage and history of cardiac or coronary artery disease.
Measurements
The following data were recorded: SAPS (Simplified Acute Physiology Score) II, age, gender, weight, body mass index, diagnosis, past medical history (hypertension, diabetes mellitus), tidal volume, respiratory rate, positive end-expiratory pressure (PEEP) and plateau pressure.
Haemodynamic parameters
All patients were monitored by a radial or femoral artery transducer. Heart rate (HR), and mean systolic and diastolic arterial pressure were recorded. Central venous pressure (CVP) was recorded via a central venous line.
Echocardiographic parameters
Transthoracic Doppler echocardiography was performed using a Philips Envisor HD (Philips Medical System, Suresnes, France) equipped with a phased array transthoracic probe (2–4 MHz). All examinations were performed by the same observer (YM) blinded to clinical data. All measurements were recorded at end-expiration over four consecutive cardiac cycles. Echocardiographic data were analysed off line.
The diameter (D) of the LV outflow tract was measured from the parasternal long-axis view and the area (A) was calculated as follows: A = π D2/4. From the apical five-chamber view, the velocity–time integral of subaortic blood flow (VTIAo) was measured and SV and cardiac output (CO) were calculated as follows: SV = VTIao × A; CO = SV × HR.
From the apical four-chamber view, transmitral flow velocities were recorded with the pulse wave Doppler sample volume placed at the mitral tips. Peak early (E) and late (A) velocities were recorded, as well as E wave deceleration time (EDT). The Tei index (myocardial performance index) was measured as previously described by Tei et al. [8]. From the same view, mitral annulus velocities were obtained using tissue Doppler settings, with the Doppler sample volume placed at the lateral side of the mitral annulus. Myocardial systolic velocity (S′) and early (E′) and late (A′) diastolic velocities were measured, and the E/E′ ratio was calculated. From the same view, left ventricular end-diastolic area (LVEDA) and ejection fraction (EF) were measured according to Simpson’s method. To assess reproducibility, all Doppler echocardiographic variables were measured twice in ten patients by the same observer (YM) after a 2-min interval.
Study protocol
Doppler echocardiography was performed before and 5 min after the intravenous infusion of 500 ml of saline solution over 20 min. Ventilator parameters and/or dose of vasopressors/inotropes were not modified during the study. Patients were classified in two groups according to the percentage increase of SV in response to VE on the assumption that a 15 % increase of SV was clinically significant. Patients with an increase of SV >15 % or <15 % were classified as responders (R) and non-responders (NR), respectively.
Statistical analysis
Continuous variables were expressed as the mean ± standard deviation (SD), and qualitative variables were reported as the number and proportion. Continuous data were assessed using the Kolmogorov–Smirnov test for equality of variance. Baseline values of each parameter were compared using a t test for independent samples with a p value of <0.05 considered to be significant. The VE-induced variation (∆) of each parameter was calculated as the difference between the two values (value after VE minus the baseline value) divided by the baseline value, and presented as the mean percentage ± standard error of the mean (SEM). An analysis of covariance (ANCOVA) test was performed to compare the ∆ of each parameter between the two groups (baseline values were used as covariables). A Bonferroni corrected p value of <0.05 was considered to be statistically significant. A subgroup analysis was performed using an E′ cut-off value of 0.12 m/s [3, 9] to discriminate between patients with diastolic dysfunction at baseline (E′ < 0.12 m/s) and patients without diastolic dysfunction (E′ ≥ 0.12 m/s). Correlations between VE-induced variations of E′ and E/E′ and SV variation were established by linear regression analysis after checking the normal distribution of the data. Intra-observer reproducibility was assessed in ten patients for SV, S′, E′, A′, EDT, E, A, Tei index and LVEDA. Each variable was measured twice in ten patients by the same observer. The difference was calculated and divided by the mean of the two values. Statistical analysis was performed by MedCalc ver. 8.2.1.0 (MedCalc Software, Mariakerke, Belgium) and StatView ver. 5.0 (SAS Institute, Cary, NC).
Results
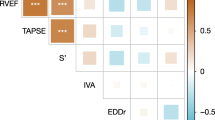
Intraobserver reproducibility was 4 ± 3, 3 ± 3, 2 ± 2, 3 ± 2, 7 ± 4, 2 ± 3, 2 ± 1, 4 ± 3, 9 ± 5 % for SV, S′, E′, A′, EDT, E, A, Tei index and LVEDA, respectively.
Ninety-four patients were initially eligible for inclusion in the study, and 83 were finally included: six patients were excluded due to poor echogenicity, four due to onset of arrhythmia during the study and one due to haemodynamic instability requiring an increased norepinephrine dose after the first echocardiography.
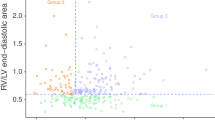
Twenty-four (29 %) patients were NR and 51 (71 %) were R based on VE. Fifty-eight (70 %) patients were treated with vasopressors. Demographic data for the two groups are presented in Table 1, and the baseline values of the two groups are compared in Table 2. At baseline, statistical differences between the two groups were observed for SV and CO, both of which were higher in the NR group, and for the Tei index, which was shorter in the NR group. Comparison of VE-induced variations (∆) between the two groups are shown in Table 3. The CVP increased in both groups, confirming that right ventricular preload increased after VE. Forty-seven patients (57 %) had a LV diastolic dysfunction, and 33 (56 %) R and 14 (58 %) NR had diastolic dysfunction. Analysis of the entire study population showed that ∆E′ was higher in R patients than in NR patients (22 ± 4 vs. 5 ± 6 %, respectively; p = 0.022), while ∆E/E′ was lower in R patients than in NR patients (8 ± 5 vs. 28 ± 8 %, respectively; p = 0.023) (Table 3). Analysis of patients with LV diastolic dysfunction showed that ∆E′ was higher in R patients than in NR patients (29 ± 5 vs. 5 ± 8 %, respectively; p = 0.01), while ∆E/E′ was higher in NR patients (35 ± 9 vs. 2 ± 6 %, respectively; p = 0.02) (Table 4; Fig. 1). In contrast, analysis of patients without LV diastolic dysfunction did not reveal any significant difference between R and NR patients for either ∆E′ (13 ± 6 vs. 6 ± 10 %, respectively; p = 0.48) or ∆E/E′ (14 ± 8 vs. 19 ± 12 %, respectively; p = 0.73) (Table 5; Fig. 1). For patients with LV diastolic dysfunction, ∆E′ was correlated with ∆SV (r = 0.37, p = 0.01), while correlation between ∆E/E′ and ∆SV did not reach significance level (r = −0.22, p = 0.13). Examples of an R patient and an NR patient with diastolic dysfunction are shown in Fig. 2.
Comparison of volume expansion-induced variations (∆) in peak velocity of the mitral annulus early wave during diastole (E′) and the ratio of mitral flow early wave velocity/E′ (E/E′) in responders and non-responders. For patients with left ventricular (LV) diastolic dysfunction at baseline, ∆E′ was greater for responders than for non-responders; in contrast, ∆E/E′ was greater for non-responders. These differences were not significant for patients without LV dysfunction. *p < 0.05
a An example of a responder patient with LV diastolic dysfunction. Stroke volume (SV) increased with volume expansion (VE) (from 48 to 56 ml). Peak E′ wave velocity increased with VE (from 0.0866 to 0.116 m/s), as did the peak E wave velocity (from 0.937 to 1.13 m/s), but the E/E′ wave did not increase (from 10.8 to 9.7). This 52-year-old patient has no history of hypertension or other cardiovascular disease. b An example of a non-responder patient with LV diastolic dysfunction. SV did not increase with VE (from 55 to 53 ml). Peak E′ velocity did not increase with VE (from 0.0782 to 0.0768 m/s), but peak E wave velocity increased (from 0.886 to 1.11 cm/s) and the E/E′ ratio also increased (from 11.3 to 14.4). This 48-year-old patient has no history of hypertension or other cardiovascular disease
Discussion
The results of this study show that VE induced a more marked increase of the E′ wave in R than in NR, especially when diastolic dysfunction was present prior to VE. In contrast, E/E′, a ratio related to LV filling pressures, was increased to a significantly greater extent in NR than in R.
Diastole is a complex mechanism during which various interrelated events lead to ventricular filling before ejection [10]. There are two major determinants of LV filling: LV relaxation and effective chamber compliance. Chamber compliance is a passive property of the left ventricle, while ventricular relaxation is the active ATP-dependent part of diastole during which myofibrils return to their precontraction state. The best approach to explore LV relaxation is to perform invasive measurement of LV pressure. As the decline in LV pressure is assumed to be exponential with time, a time constant (τ) can be calculated based on the time required for LV pressure to decrease by approximately two-thirds of its baseline value [4, 10–13]. τ has been considered to be the best index to evaluate relaxation [4, 11]. However, LV catheterization is not feasible at the bedside in the Intensive Care Unit (ICU). Doppler echocardiography techniques can be used to accurately assess LV relaxation [14, 15]. The mitral annulus early wave velocity during diastole (E′) has been recently used to assess LV relaxation, as this index is considered to be preload-independent [5]. Several studies have demonstrated that E′ is correlated with τ and that E′ does not change significantly in response to different loading conditions [5, 6, 16–18].
In our study, peak velocity of the E′ wave increased by about 30 % after VE in patients in the R group with pre-existing LV diastolic dysfunction (Table 4), corresponding to enhancement of relaxation. Moreover, this enhancement is negligible when LV diastolic function is not impaired.
LV diastolic dysfunction may be related to sepsis [3] or to sepsis-related hypovolaemia [19]. Enhancement of LV relaxation in the R group can be explained by the fact that, in these hypovolaemic patients with circulatory failure, VE induced an increase in stroke volume, resulting in improved coronary flow and myocardial perfusion. As relaxation is an ATP-dependent phenomenon, it is likely to be enhanced by improved perfusion. This assertion is supported by the fact that ∆E′ is correlated with ∆SV in patients with LV diastolic dysfunction. Dhainault et al. [7], studying 40 patients with septic shock, found a close curvilinear correlation between coronary blood flow and mean arterial pressure, showing that improvement in global haemodynamics may improve myocardial perfusion. In addition, D’Annunzio et al. [19] reported that an experimental haemorrhagic shock induced an impairment in LV relaxation which fully recovered with restoration of normal volaemia by blood reinfusion.
Another explanation is that enhancement of LV relaxation could be due to a decrease in HR. However, an increase in the HR rather than a decrease in the HR would enhance relaxation. When the HR increases, relaxation is enhanced to compensate for the decreased diastolic time interval: this phenomenon is called FDAR (frequency-dependent acceleration of relaxation) [20] and may be partially impaired during sepsis [21]. Moreover, in our patients, the decrease in HR was about 5 % and was similar in both groups (Table 3).
Yet another explanation is the possible decrease in afterload. Several studies have demonstrated the afterload sensitivity of relaxation [22, 23]. Increasing SV and CO by VE may have decreased the levels of endogenous vasopressors (catecholamines, vasopressin, angiotensin, endothelin), which are increased during sepsis [24]. Nevertheless, in our study, the increase in SV was followed by an increase in BP.
An alternative explanation is that, despite the fact that E′ is correlated with τ, it is also dependent on preload [25]. Firstenberg et al. [26], in an animal model, found that despite a good correlation between τ and E′ (r = 0.70, p < 0.001), the E′ was preload-dependent. Nevertheless, these authors demonstrated that, in a setting of impaired relaxation (prolonged τ), E′ was less dependent on preload. These results were confirmed by other authors [25–27]. In our study, the variation in E′ was significantly greater for R than for NR only in the presence of impaired relaxation (Tables 4, 5) when E′ is less dependent on preload.
Another index of relaxation was used in our study, which confirmed the results observed for E′. The Tei Index is an index of global myocardial function depending on both systolic and diastolic function [8]. The decrease of the Tei index in the R group of patients with diastolic dysfunction indicates enhancement of LV function (systolic, diastolic or both), but the fact that the peak velocity of the S′ wave (a parameter of systolic function) variations were not significantly higher in the R group shows that this enhancement was limited to diastolic function.
Another interesting finding of this study is that the ∆E/E′ in patients with diastolic dysfunction was significantly higher in the NR group than in the R group. Several studies conducted in cardiology or in the ICU have demonstrated that this ratio is closely correlated with pulmonary artery occlusion pressure (PAOP) [5, 28–34]. In our study, E/E′ increased significantly in patients who received inadequate VE (not followed by an increase in SV). In the R group, the left ventricle functions over the steep part of the Frank–Starling curve and the flat part of the pressure–volume relationship. Consequently, when VE increases preload (as reflected by an increase in LVEDA), SV is also increased, with no corresponding increase in E/E′ (related to PAOP). In contrast, in the NR group, the left ventricle functions over the flat part of the Frank–Starling curve and the steep part of the LV volume–pressure curve; consequently, VE does not increase either LVEDA (despite an increase in CVP) or SV, but increases PAOP. Further investigations using invasive measurements of PAOP are necessary to validate this hypothesis and especially to evaluate the E/E′ ratio as an index of fluid loading tolerance. A comparison of our results with those of previous studies analysing the influence of VE on LV filling pressures shows that in several studies PAOP increased with VE in both groups (N and NR) but that in the majority of these studies, PAOP increased to a greater extent in the NR group than in the R group [35–40]. Lamia et al. [41], who studied the effect of VE on the E/E′ ratio, found similar results: in the R group there was no increase in the E/E′ ratio despite the increase in LVEDAi, while in the NR group, the E/E′ ratio increased (from 6.8 ± 2.1 to 7.4 ± 2.0)—but not significantly, probably because of the small sample size—and LVEDAi was not significantly increased.
There are a number of limitations to our study. First of all, we used the threshold value of 12 cm/s to define diastolic dysfunction, as previously used by Bouhemad et al. [3] in a comparable study population. One could argue that this value is higher than previously published: Nagueh et al. [5] and Sohn et al. [42] reported a threshold value for discriminating between normal and abnormal relaxation that was closer to 8.5 cm/s. Nevertheless, the control group in these studies were identified on the basis of having no symptoms or a history of heart failure rather than on objective measurements of diastolic function, and it can therefore be easily argued that despite the absence of overt symptoms, an impairment of relaxation as a result of ageing did occur. When focusing on transmitral flow pattern, the same authors [43] reported a cut-off value of 13 cm/s to discriminate between control and pseudonormal participants. Moreover, Dumesnil et al. [44], studying 40 patients classified according to the Canadian Consensus definition of diastolic function, suggested that the threshold value of E′ to identify diastolic dysfunction should be approximately 12.5 cm/s [9].
Secondly, values of SV and CO were higher in the NR group. We could hypothesize that these patients had received more fluids prior to the study. This confounding factor cannot be eliminated as data on the quantity of fluid infused prior to inclusion were not collected. Nevertheless, baseline values of E′ and E/E′ were similar in both groups. Thirdly, we did not study the E′ wave at the septal part of the mitral annulus. We only focused on the lateral part of the mitral annulus, as several studies have shown that E′ is more preload-sensitive when measured at the septal portion [6, 45, 46]. Fourthly, one could argue that the weak reproducibility of the E′ wave measurement may explain the result. We found a reproducibility of 2 ± 2 % for E′ (consistent with other studies), which is far less than the observed values of ∆E′. Finally, other parameters of diastolic function do exist but were not used in this study (e.g. flow propagation velocity at early transmitral flow or isovolumic relaxation time). We focused on the most often used parameters with the best reproducibility available.
Conclusions
To summarize, the results of our study suggest that an adequate fluid infusion (a simple and first-line treatment) enhances LV relaxation of hypovolaemic septic patients. This finding is of crucial importance as relaxation is frequently impaired in patients with septic shock. Further studies are necessary to investigate whether E′ peak velocities could be a therapeutic target and the E/E′ an index of VE tolerance in critically ill patients.
References
Pirracchio R, Cholley B, De Hert S, Solal AC, Mebazaa A (2007) Diastolic heart failure in anaesthesia and critical care. Br J Anaesth 98:707–721
Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, Stewart D, Venkatesh B (2010) Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care 14:R44
Bouhemad B, Nicolas-Robin A, Arbelot C, Arthaud M, Feger F, Rouby J-J (2008) Isolated and reversible impairment of ventricular relaxation in patients with septic shock. Crit Care Med 36:766–774
Nishimura RA, Tajik AJ (1997) Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician’s Rosetta stone. J Am Coll Cardiol 30:8–18
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Vignon P, Allot V, Lesage J, Martaillé JF, Aldigier JC, François B, Gastinne H (2007) Diagnosis of left ventricular diastolic dysfunction in the setting of acute changes in loading conditions. Crit Care 11:R43
Dhainault JF, Huyghebaert M-F, Monsallier JF, Lefevre G, Dall’ava-Santucci J, Brunet F, Villemant D, Carli A, Raichvarg D (1987) Coronary hemodynamics and myocardial metabolism of lactate, free fatty acids, glucose, and ketones in patients with septic shock. Circulation 75:533–541
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodheffer RJ, Tajik AJ, Seward JB (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 26:357–366
Dumesnil JG, Paulin C, Pibarot P, Coulombe D, Arsenault M (2002) Mitral annulus velocities by Doppler tissue imaging: practical implications with regard to preload alterations, sample position, and normal values. J Am Soc Echocardiogr 15:1226–1231
Brutsaert DL, Rademakers FE, Sys SU (1984) Triple control of relaxation: implications in cardiac disease. Circulation 69:190–196
Zile MR, Brutsaert DL (1997) New concepts in diastolic dysfunction and diastolic heart failure: Part I. Circulation 105:1387–1393
Weiss JL, Fredericksen JW, Weisfeldt ML (1976) Hemodynamic determinants of the time course of fall in canine left ventricular pressure. J Clin Invest 58:83–95
Mahjoub Y, Lorne E, Maizel J, Plantefève G, Massy ZA, Dupont H, Slama M (2011) Effect of intra-abdominal hypertension on left ventricular relaxation: a preliminary animal study. Br J Anaesth 108:211–215
Appleton CP, Hatle CK (1992) The natural history of left ventricular filling abnormalities: assessment of two-dimensional and Doppler echocardiography. Echocardiography 9:437–457
Nishimura RA, Abel MD, Hatle LK, Tajik AJ (1989) Assessment of diastolic function of the heart: background and current applications of Doppler echocardiography. Part II: clinical studies. Mayo Clin Proc 64:181–204
Choong CY, Herrmann HC, Weyman AE, Fifer MA (1987) Preload dependence of Doppler-derived indexes of left ventricular diastolic function in humans. J Am Coll Cardiol 10:800–808
Oki T, Tabata T, Yamada H, Wakatsuki T, Shinohara H, Nishikado A, Iuchi A, Fukuda N, Ito S (1997) Clinical application of pulsed Doppler tissue imaging for assessing abnormal left ventricular relaxation. Am J Cardiol 79:921–928
Aranda JM Jr, Weston MW, Puleo JA, Fontanet HL (1998) Effect of loading conditions on myocardial relaxation velocities determined by Doppler tissue imaging in heart transplant recipients. J Heart Lung Transpl 17:693–697
D’annunzio V, Donato M, Fellet A, Buchholz B, Antico Arciuch VG, Carreras MC, Valdez LB, Zaobornyj T, Morales C, Boveris A, Poderoso JJ, Balaszczuk AM, Gelpi RJ (2012) Diastolic function during hemorrhagic shock in rabbits. Mol Cell Biochem 359:169–176
Janssen PM, Periasamy M (2007) Determinants of frequency-dependent contraction and relaxation of mammalian myocardium. J Mol Cell Cardiol 43:523–531
Joulin O, Marechaux S, Hassoun S, Montaigne D, Lancel S, Neviere R (2009) Cardiac force-frequency relationship and frequency-dependent acceleration of relaxation are impaired in LPS-treated rats. Crit Care 13:R14
Karliner JS, LeWinter MM, Mahler F, Engler R, O’Rourke RA (1977) Pharmacologic and hemodynamic influences on the rate of isovolumic left ventricular relaxation in the normal conscious dog. J Clin Invest 60:511–521
Raff GL, Glantz SA (1981) Volume loading slows left ventricular isovolumic relaxation rate. Evidence of load-dependent relaxation in the intact dog heart. Circ Res 48:813–824
Abboud I, Lerolle N, Urien S, Tadié J-M, Leviel F, Fagon J-Y, Faisy C (2009) Pharmacokinetics of epinephrine in patients with septic shock: modelization and interaction with endogenous neurohormonal status. Crit Care 13:R120
Jacques DC, Pinsky MR, Severyn D, Gorcsan J III (2004) Influence of alterations in loading on mitral annular velocity by tissue Doppler echocardiography and its associated ability to predict filling pressures. Chest 126:1910–1918
Firstenberg MS, Greenberg NL, Main ML, Drinko JK, Odabashian JA, Thomas JD, Garcia MJ (2001) Determinants of diastolic myocardial tissue Doppler velocities: influences of relaxation and preload. J Appl Physiol 90:299–307
Ruan Q, Rao L, Middleton KJ, Khoury DS, Nagueh SF (2006) Assessment of left ventricular diastolic function by early diastolic mitral annulus peak acceleration rate: experimental studies and clinical application. J Appl Physiol 100:679–684
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and Doppler tissue imaging in the estimation of left ventricular filling pressures. Circulation 102:1788–1794
Seo Y, Ishimitsu T, Ishizu T, Obara K, Moriyama N, Sakane M, Maeda H, Watanabe S, Yamaguchi I (2004) Preload-dependent variation of the propagation velocity in patients with congestive heart failure. J Am Soc Echocardiogr 17:432–438
Vignon P, AitHssain A, François B, Preux PM, Pichon N, Clavel M, Frat JP, Gastinne H (2008) Echocardiographic assessment of pulmonary artery occlusion pressure in ventilated patients: a transoesophageal study. Crit Care 12:R18
Nagueh SF, Mikati I, Kopelen HA, Middleton KJ, Quiñones MA, Zoghbi WA (1998) Doppler estimation of left ventricular filling pressure in sinus tachycardia. A new application of tissue Doppler imaging. Circulation 98:1644–1650
Bouhemad B, Nicolas-Robin A, Benois A, Lemaire S, Goarin JP, Rouby JJ (2003) Echocardiographic Doppler assessment of pulmonary capillary wedge pressure in surgical patients with postoperative circulatory shock and acute lung injury. Anesthesiology 98:1091–1100
Combes A, Arnoult F, Trouillet JL (2004) Tissue Doppler imaging estimation of pulmonary artery occlusion pressure in ICU patients. Intensive Care Med 30:75–81
Tousignant CP, Walsh F, Mazer DC (2000) The use of transesophageal echocardiography for preload assessment in critically ill patients. Anesth Analg 90:351–355
Bendjelid K, Suter PM, Roman JA (2004) The respiratory change in preejection period: a new method to predict fluid responsiveness. J Appl Physiol 96:337–342
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL (2005) Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 31:517–523
Reuter DA, Kirchner A, Felbinger TW, Weis FC, Kilger E, Lamm P, Goetz AE (2003) Usefulness of left ventricular stroke volume variation to assess fluid responsiveness in patients with reduced cardiac function. Crit Care Med 31:1399–1404
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL (2007) Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med 35:64–68
Wyffels PAH, Durnez PJ, Helderweirt J, Stockman WM, De Kegel D (2007) Ventilation-induced plethysmographic variations predict fluid responsiveness in ventilated postoperative cardiac surgery patients. Anesth Analg 105:448–452
Natalini G, Rosano A, Taranto M, Faggian B, Vittorielli E, Bernardini A (2006) Arterial versus plethysmographic dynamic indices to test responsiveness for testing fluid administration in hypotensive patients: a clinical trial. Anesth Analg 103:1478–1484
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL (2007) Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33:1125–1132
Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW (1997) Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 30:474–480
Nagueh SF, Bachinski LL, Meyer D, Hill R, Zoghbi WA, Tam JW, Quinones MA, Roberts R, Marian AJ (2001) Tissue Doppler imaging consistently detects myocardial abnormalities in patients with hypertrophic cardiomyopathy and provides a novel means for an early diagnosis before and independently of hypertrophy. Circulation 104:128–130
Rakowski H, Appleton C, Chan KL, Dumesnil JG, Honos G, Jue J, Koilpillai C, Lepage S, Martin RP, Mercier LA, O’Kelly B, Prieur T, Sanfilippo A, Sasson Z, Alvarez N, Pruitt R, Thompson C, Tomlinson C (1996) Canadian consensus recommendations for the measurement and reporting of diastolic dysfunction by echocardiography: from the Investigators of Consensus on Diastolic Dysfunction by Echocardiography. J Am Soc Echocardiogr 9:736–760
Ie EH, Vletter WB, ten Cate FJ, Nette RW, Weimar W, Roelandt JR, Zietse R (2003) Preload dependence of new Doppler techniques limits their utility for left ventricular diastolic function assessment in hemodialysis patients. J Am Soc Nephrol 14:1858–1862
Oguzhan A, Arinç H, Abaci A, Topsakal R, Kemal Eryol N, Ozdogru I, Basar E, Ergin A (2005) Preload dependence of Doppler tissue imaging derived indices of left ventricular diastolic function. Echocardiography 22:320–325
Acknowledgments
The authors would like to thank Mr. M. Diouf for his assistance with statistical methodology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mahjoub, Y., Benoit-Fallet, H., Airapetian, N. et al. Improvement of left ventricular relaxation as assessed by tissue Doppler imaging in fluid-responsive critically ill septic patients. Intensive Care Med 38, 1461–1470 (2012). https://doi.org/10.1007/s00134-012-2618-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2618-9