Abstract
Purpose
During neurally adjusted ventilatory assist (NAVA), it is difficult to quantify the relative contribution of the patient versus the ventilator to the inspiratory tidal volume (Vtinsp). To solve this problem, we developed an index, the “patient–ventilator breath contribution” (PVBC), using the inspiratory deflection of the diaphragmatic electrical activity (∆EAdi) and Vtinsp during assisted and non-assisted breaths. This study evaluated the PVBC index in an experimental setup.
Method
Nine intubated and sedated rabbits were studied during repeated ramp increases of the NAVA level. One breath was non-assisted at each NAVA level. The PVBC index was evaluated during resistive loading and after acute lung injury. PVBC was calculated by relating Vtinsp/∆EAdi of a non-assisted breath to that of the preceding assisted breath. The PVBC was compared to the relative contribution of esophageal pressure (∆Pes) to transpulmonary pressure deflections (∆P L,dyn).
Results
The relationship between PVBC and ∆Pes/∆P L,dyn was slightly curvilinear with an intercept different from zero (y = −1x 2 + 1.64x + 0.21) and a determination coefficient (R 2) of 0.95. Squaring the PVBC values resulted in a near perfect linear relationship (y = 1.02x + 0.05) between PVBC2 and ∆Pes/∆P L,dyn with an R 2 of 0.97.
Conclusion
This study shows that Vtinsp and EAdi can be used to predict the contribution of the inspiratory muscles versus that of the ventilator during NAVA. If clinically applicable, this could serve to quantify and standardize the adjustment of the level of assist, and hence reduce the risks of excessive ventilatory assist. Further studies are required to evaluate if this method is clinically applicable.
Similar content being viewed by others
Introduction
Mechanical ventilation has evolved from a treatment that overrides the patient’s breathing (controlled mechanical ventilation) into the more interactive concept of “partial ventilatory assist”, where the ventilator partially assists breathing. When synchronized, both the patient and the ventilator contribute to the lung-distending pressure necessary to overcome the inspiratory load and generate the inspiratory tidal volume (Vtinsp) [1]. However, the relative contribution of patient effort versus the ventilator contribution to Vtinsp remains unknown for all modes except for certain applications of proportional assist ventilation (PAV+) [2]. Quantification of this variable is important since inappropriate assist levels are associated with adverse effects. When assist is too low, fatigue and respiratory failure may develop [3]; when assist is set too high, diaphragm impairment may ensue [4, 5].
The introduction of neurally adjusted ventilatory assist (NAVA) [6] and measurements of diaphragm electrical activity (EAdi) has made it possible to quantify neural inspiratory drive. Yet, there is no information about the relative contribution to a breath between the patient and the ventilator during NAVA, which would help to quantify and standardize the adjustment of the level of assist. We hypothesized that a simple measurement of Vtinsp and the inspiratory change in EAdi (∆EAdi) during one non-assisted breath and one ventilator-assisted breath would allow the calculation of a patient–ventilator breath contribution (PVBC) index. The reasoning was as follows: during an inspiration without ventilator assistance, the patient’s neural inspiratory effort (reflected by ∆EAdi) generates Vtinsp. If adding synchronized assist to the patient’s neural inspiratory effort, the resulting Vtinsp depends on the sum of patient and ventilator pressure contribution. If the patient’s neural inspiratory effort remains the same during both non-assisted and assisted breaths, the ratio of Vtinsp during the non-assisted and assisted breaths should reflect the relative contribution of the patient to the inspiratory volume of the ventilator. As it is unlikely that neural inspiratory efforts are identical for two consecutive breaths, normalizing the Vtinsp to the ∆EAdi (Vtinsp/∆EAdi, in units of ml/μV) offers a potential solution. A PVBC index could be expressed by the ratio of Vtinsp/∆EAdi without assist and Vtinsp/∆EAdi with assist [i.e., (Vtinsp/∆EAdi)no-assist/(Vtinsp/∆EAdi)assist]. A PVBC index close to 1 indicates that the patient is generating the Vtinsp, with little or no contribution from the ventilator. A PVBC index close to zero indicates that the ventilator contributes to most of the Vtinsp.
The present study validates the PVBC index against directly measured pressure parameters during NAVA in rabbits during conditions of airflow obstruction and acute lung injury (ALI).
Materials and methods
The study was approved by St. Michael’s Hospital Animal Care and Use Committee. Care was performed in accordance with the Canadian Council on Animal Care.
Procedures and instrumentation
Nine sedated spontaneously breathing adult male New Zealand white rabbits weighing 2.8–3.4 kg were studied. All animals were instrumented to continuously measure arterial blood pressure (BP), transcutaneous oxygen saturation (PtcO2), Pes, gastric pressure (Pga), and EAdi as well as airway pressure (Paw), flow, and tidal volume during inspiration (Vtinsp) and expiration (Vtexp). Blood gases were obtained at the beginning and end of each protocol. Descriptions of anesthesia, instrumentation, physiological measurements, and NAVA are provided in the Electronic Supplementary Material (ESM).
Experimental protocol
First, animals breathed with NAVA set to zero, positive end-expiratory pressure (PEEP) 2 cmH2O, and a fraction of inspired oxygen (FiO2) of 40 % (baseline period).
Then, in each healthy rabbit, four consecutive ramp increases of the NAVA level were performed after the sequential application of two different resistive loads (R1 and R2). Thereafter ALI was induced in the rabbits by intratracheal installation of HCl; about 30 min later the same ramp increase in NAVA levels was performed during ALI (without resistive loading).
For all conditions (except initial baseline period), PEEP was set to 5 cmH2O and the NAVA level was increased every 20 s and repeated with two different rates of ramp increase: slow (steps of 0.2 cmH2O/µV every 20 s) and fast (steps of 0.4 cmH2O/µV every 20 s) to ensure reproducibility regardless of step changes in assist. In summary, the following conditions were tested in each animal:
-
1.
High resistance/slow ramp (R1slow)
-
2.
High resistance/fast ramp (R1fast)
-
3.
Very high resistance/low ramp (R2slow)
-
4.
Very high resistance/fast ramp (R2fast)
-
5.
ALI/slow ramp (ALIslow)
-
6.
ALI/fast ramp increase (ALIfast)
Stepwise increases in the NAVA level were performed starting from a NAVA level of zero and terminated at a NAVA level corresponding to 100 % unloading. The latter was defined as the point where the increase of the NAVA level did not further suppress the EAdi and where the negative inspiratory deflections of Pes were abolished. At each NAVA level, one non-assisted breath was obtained by automatically zeroing the NAVA level (reprogrammed algorithm that omitted the assist delivery) during a single inspiration and delivered PEEP of 5 cmH2O. At every second NAVA level (i.e., every 40 s), the non-assisted breath was followed by an end-expiratory occlusion, resulting in one inspiratory effort against occluded airways. At the end of each run, the NAVA level was returned to zero for a stabilization period in the respective condition before the next ramp increase of the NAVA level commenced. For more information see ESM.
Data analysis
Off-line breath-by-breath analysis was performed on EAdi, Pes, and Paw waveforms. Inspiratory time (Ti) and mean inspiratory deflection of ∆EAdi, ∆Paw, and ∆Pes were calculated between the onset of EAdi and the point where EAdi dropped to 70 % of peak. Transpulmonary pressure (∆P L,dyn) was calculated as ∆Paw − ∆Pes. Intrinsic PEEP (PEEPi) was measured as the increase in Paw during end-expiratory occlusion and was corrected for expiratory muscle recruitment [7].
Since the ramp increases of the NAVA level had different duration and number of step changes for each condition, the ∆Pes values of each run were normalized to baseline ∆Pes values obtained at the beginning of the run (NAVA zero level) and then divided into five parts (“quintiles of unloading”). Individual data corresponding to a quintile of unloading was sorted for each variable into the respective quintile. Finally, the average value was calculated for each quintile.
Description of PVBC and associated indices
The PVBC index was calculated as (Vtinsp/∆EAdi)no-assist/(Vtinsp/∆EAdi)assist. An index directly quantifying how much the inspiratory muscle effort contributed to the total lung-distending pressure during assisted breaths was calculated as ∆Pes/∆P L,dyn. Additional indices validating the PVBC index are presented in the ESM.
Statistical analysis
SigmaStat (3.10, Systat Software inc., San Jose, CA, USA) was used for statistical analysis. Values in the text and figures are mean ± SD, unless otherwise indicated. The relationship between different variables was tested with linear regression analysis. A two-way repeated measures ANOVA was performed and post hoc comparison was performed by Student–Newman–Keuls test to compare the relevant variables between the different experimental conditions and at different levels of unloading. The level of significance was p < 0.05.
Results
All nine animals completed four ramp increases in NAVA level (2 slow and 2 fast) with two different levels of resistive loading. Two animals died immediately after intratracheal instillation of HCl. Thus, seven animals underwent slow and fast ramp increases of the NAVA level after ALI.
After ALI, compliance of the respiratory system decreased by 50 % (from 5.0 ± 1.2 to 2.5 ± 0.4 ml/cmH2O). The mean PaO2/FiO2 ratio before ALI was 494 ± 42 and decreased to 128 ± 33 at 5 min post-ALI.
The NAVA levels reached higher values during R1 and R2 than during ALI (Table 1). ∆Paw and PEEPi values observed at the highest NAVA level were significantly lower for ALI than for R1 and R2. No animal showed signs of asynchrony, discomfort, or required a bolus of sedatives at higher NAVA levels. Respiratory rate, inspiratory and expiratory time are presented in Table E1 (ESM).
The rate of increase of the NAVA level did not affect any of the measured parameters. The mean duration of the increases in NAVA level for different conditions were 5.6–8.0 (fast increase) and 9.6–14.6 (slow increase) min.
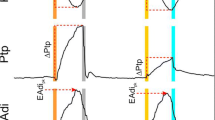
Figure 1 exemplifies a ramp increase of NAVA level during R1 load. The initial increase of NAVA level increased ∆Paw (top panels) and reduced ∆EAdi (middle panels) and ∆Pes (bottom panels). At higher NAVA levels ∆EAdi and ∆Pes continued to decrease, whereas the increase in ∆Paw became less pronounced. The right panel of Fig. 1 (sections B and C) shows that although the ∆EAdi and ∆Pes waveforms did not change much between assisted and non-assisted (arrow) breaths, Vtinsp was decreased during the non-assisted breath. Time tracings of EAdi and pressures are presented in Fig. E1 (ESM).
Response to progressive increase in neurally adjusted ventilatory assist (NAVA) level and demonstration of non-assisted breaths in one animal. Left panel From top to bottom the y-axes indicate mean inspiratory deflection in airway pressure (ΔPaw) in cmH2O, and mean inspiratory deflection in electrical activity of the diaphragm (ΔEAdi), and mean inspiratory deflection in esophageal pressure (ΔPes). ΔEAdi and ΔPes are expressed as % of respective values at zero NAVA level (% ΔEAdi@NAVA0) and % ΔPes@NAVA0). The x-axes show the progressive increase in NAVA level. Three periods (zero, intermediate, and highest NAVA level) of the titration are indicated by shaded vertical bars (A–C). Note that values pertain only to assisted breaths. Right panel Raw tracings of ΔPaw, ΔEAdi, volume, and ΔPes from the corresponding sections (A–C). The arrows indicate non-assisted breaths (NAVA zero)
A strong and near-linear relationship (R 2 = 0.96) between ∆EAdi (in μV) and ∆Pes (in cmH2O) was observed for all breaths during all conditions and levels of unloading (Fig. 2). During end-expiratory occlusions, the determination coefficients (R 2) between Paw and Pes deflections were 0.97 ± 0.03, 0.97 ± 0.01, and 0.98 ± 0.02 for R1, R2, and ALI, respectively.
Relationship between mean inspiratory deflections in electrical activity of the diaphragm (ΔEAdi, y-axis) and esophageal pressure (ΔPes, x-axis). There was a strong, near-linear relationship (R 2 = 0.96) between ΔEAdi (in μV) and ΔPes (in cmH2O). Values are depicted for all conditions and levels of unloading during acute lung injury (ALI, circles), high (R1, squares), and very high (R2, triangles) resistive loads. Blue and red symbols indicate slow and fast ramp increases of the NAVA level. Non-assisted and assisted breaths are indicated by open and filled symbols, respectively
With increasing NAVA levels, Vtinsp and ∆P L,dyn showed a close relationship for both assisted and non-assisted breaths, where ∆P L,dyn shifted towards higher values for a given Vtinsp as conditions were changing from ALI to R1 to R2 (Fig. E2 in ESM).
Figure 3 shows the mean values for variables building up to the PVBC index for breaths with and without assist for each quintile of unloading. As unloading progresses, Vtinsp/Ti, Vtinsp, and Vtexp increased during assisted breaths (solid symbols) but decreased during the non-assisted breaths (open symbols). During non-assisted breaths, unloading caused an increasing discrepancy between Vtinsp and Vtexp and this difference was smallest during ALI and largest during R2. The ∆EAdi decreased in both assisted and non-assisted breaths with higher levels of unloading. ∆EAdi consistently demonstrated slightly but significantly higher values during the non-assisted breaths (see also Fig. E1 in ESM). During assisted breaths Vtinsp/ΔEAdi increased progressively with unloading. With regard to non-assisted breaths, Vtinsp/ΔEAdi increased slightly during ALI, whereas no changes occurred during R1 and R2. During both assisted and non-assisted breaths, Vtinsp/ΔEAdi was higher during ALI than during both resistive loading runs. The PVBC index decreased during all conditions as the unloading progressed with increasing NAVA levels, the least reduction observed after ALI and the highest reduction during the highest (R2) resistive load.
Responses to increasing neurally adjusted ventilatory assist (NAVA) levels during each condition for the patient ventilator breath contribution (PVBC) index as well as the variables that the PVBC index depends on. From top to bottom, mean inspiratory flow (Vtinsp/Ti), inspiratory volume (Vtinsp) and expiratory volume (Vtexp), mean inspiratory deflection in electrical activity of the diaphragm (ΔEAdi), neuroventilatory efficiency (NVE = Vtinsp/ΔEAdi), and PVBC are plotted on the y-axes, as a function of each quintile of unloading expressed as ΔPes in % of ΔPes at zero NAVA level (%ΔPes@NAVA0), for acute lung injury (ALI), high (R1), and very high (R2) resistive load as well as fast and slow increases of the NAVA level. Inspiratory and expiratory data are denoted by circles and squares, respectively. Assisted and non-assisted breaths are plotted as filled and empty symbols. Asterisk denotes non-significant differences assisted and non-assisted breaths
The PVBC index was closely related to ΔPes/ΔP L,dyn as depicted for all conditions and unloading levels in Fig. 4. The left panel shows that the relationship between PVBC and ΔPes/ΔP L,dyn is curvilinear with a non-zero intercept (y = −1x 2 + 1.64x + 0.21, R 2 = 0.95). Squaring the PVBC values (PVBC2, right panel) resulted in a near-linear relationship between PVBC2 and ΔPes/ΔP L,dyn (y = 1.02x + 0.05; R 2 = 0.97). Additional validation of the PVBC index is presented in the ESM.
Relationship between the reference index [(ΔPes/ΔP L,dyn)assist] and the PVBC index [(Vtinsp/EAdi)no-assist/(Vtinsp/EAdi)assist]. Left panel demonstrates ΔPes/ΔP L,dyn (x-axis) and its relationship to PVBC (y-axis) during progressive increases of the NAVA level. Right panel shows the relationship of ΔPes/ΔP L,dyn to PVBC squared (PVBC2). Values are depicted for all conditions and levels of unloading during acute lung injury (ALI, circles), high (R1, squares), and very high (R2, triangles) resistive load. Blue and red symbols indicate slow and fast ramp increases of the NAVA level, respectively. ΔPes mean inspiratory deflection in esophageal pressure, ΔP L,dyn mean inspiratory deflection in transpulmonary pressure, ΔEAdi mean inspiratory deflection in electrical activity of the diaphragm, NAVA neurally adjusted ventilatory assist, and PVBC patient ventilator breath contribution
Discussion
This study shows that the ratio of Vtinsp/ΔEAdi of a non-assisted breath to that of an assisted breath, when evaluated against several indices using airway and esophageal pressures, can provide information about the relative contribution of the patient and the ventilator to the volume generated during NAVA.
The ΔPes/ΔP L,dyn index was chosen as the most valid control measure of the relative contribution of inspiratory muscles and ventilator to breathing since it allows the dissociation of the relative contribution of lung distending pressures (P L,dyn = ΔPaw − ΔPes) generated by the inspiratory muscles (ΔPes) and the ventilator (ΔPaw). Most importantly the ΔPes/ΔP L,dyn index could be calculated during assisted breaths. ∆P L,dyn reflects the pressure generated by all inspiratory muscles distending the lung under dynamic conditions including static (needed to overcome lung elastance) and dynamic (needed to overcome resistance) pressure components. ∆P L,dyn does not take into account the pressure needed to expand the chest wall, whereas the EAdi may. Since chest wall compliance in the rabbit is about five times higher than lung compliance [8], this amount of pressure could be considered negligible.
Accuracy of using ratios of Vtinsp and ΔEAdi in the PVBC index depends on the relative activation of the diaphragm and other inspiratory and expiratory muscles. Studies in rats [9], rabbits [10], dogs [11], and patients with impaired respiratory function [12] and mechanically ventilated patients [13] show that the diaphragm acts as a single unit in response to increased respiratory demand. Recruitment of extradiaphragmatic inspiratory and expiratory muscles increases with increased respiratory demand [14] and can increase the efficiency of the diaphragm [15, 16]. Although respiratory drive increases proportionally to all muscle groups as exercise workload increases [15], the relative contribution of the inspiratory rib cage muscles may increase during diaphragmatic fatigue, preserving the ventilatory response to CO2 despite impaired diaphragmatic contractility [17]. In general, the intercostals and the diaphragm work synergistically in canines [18], rabbits [10], and in healthy subjects [15].
On the basis of the above, our finding that PVBC was closely but not linearly related to ΔPes/ΔP L,dyn (Fig. 4, left panel) could have been due to fatigue or rerecruitment. As depicted in Fig. 2, the relationship between ΔEAdi and ΔPes was very strong and near linear. This is in agreement with Beck et al. [19, 20], who showed in healthy volunteers that the EAdi, calculated as RMS (root mean square), remains close to linear in relation to transdiaphragmatic pressure up to about 75 % of its maximum. The near-linear relationships between [(Vtinsp/ΔPes)no-assist/(Vtinsp/ΔPes)assist] and PVBC (Fig. E3 in ESM) as well as [(ΔP L,dyn/ΔEAdi)no-assist/(ΔP L,dyn/ΔEAdi)assist] and ΔPes/ΔP L,dyn (Fig. E4 in ESM) contradict that systematic neuromechanical uncoupling would have caused a non-linear relationship. (see ESM for further details).
In patients with weak inspiratory muscles and/or increased respiratory system load, the maximal inspiratory volume is limited in proportion to the impairment [21, 22]. As well, the ΔEAdi is increased in patients with impaired respiratory function [12, 23]. Thus, it remains unlikely that acute respiratory failure patients with increased respiratory load and severely reduced inspiratory force reserve have too many degrees of freedom to alter their relative contribution between the diaphragm and other muscles.
As depicted in Fig. 3, increasing unloading caused Vtinsp and inspiratory flow to increase during the assisted breath, whereas they decreased during the non-assisted breath. Figure E2 (ESM) demonstrates that the transformation of ΔP L,dyn into Vtinsp followed different trajectories for non-assisted and assisted breaths. Hence, it is likely that the curvilinear relationship between PVBC index and the ΔPes/ΔP L,dyn ratio was due to an increasing discrepancy in respiratory system mechanics between non-assisted and assisted breaths.
It should also be noted that the ΔEAdi at 100 % unloading (ΔPes "approaches" zero ca. 0) intercepts ΔEAdi at a level of about 2 μV (Fig. 2). This agrees with previous studies in healthy subjects [1] and in critically ill patients [24] showing that NAVA can completely unload without abolishing neural respiratory drive. Also, when ΔPes/ΔP L,dyn tended towards zero, the intercepts for both [(ΔP L,dyn/ΔEAdi)no-assist/(ΔP L,dyn/ΔEAdi)assist] (Fig. E4 in ESM) and PVBC indices (Fig. 4, left panel) were above zero. The reason for this is that the EAdi contribution to pressure is nil during the assisted breath (i.e., no mechanical load = no pressure), whereas during the non-assisted breath mechanical load is present such that pressure and volume are generated. Consequently, the PVBC index underestimates the effect of unloading.
The slight differences for the intercepts between ALI and resistive loading observed in Figs. 4 and E4 (ESM) could suggest that hyperinflation may have induced a reduction in neuromechanical as well as neuroventilatory efficiency at increasing levels of unloading. The consequence would be that hyperinflation reduced the Vt/EAdi more during resistive loading than ALI (see ESM for further discussion).
In order to reduce the complexity of interpreting a non-linear relationship with different intercepts, applying a square of PVBC (PVBC2) resulted in a near-perfect linear 1:1 relationship to ΔPes/ΔP L,dyn (see Figs. 4 and E5 in ESM), which if applicable in critically ill patients would provide a scale between 0 and 1 for determination of “effort sharing” between patient and ventilator.
The speed of titration had no significant effect on our results and all animals had reached a stable respiratory drive at each NAVA level (Fig. E1 in ESM) which supports that respiratory drive adapts rapidly in rabbits [25]. We chose to only withdraw assist during one breath and compare it to the immediately preceding breath to avoid changes in respiratory drive as only one non-assisted breath increased ΔEAdi (Figs. 3 and E1 in ESM). The relatively small variability in ΔEAdi between assisted and non-assisted breaths suggests that we mainly corrected Vtinsp within a limited range of changes in neural respiratory drive and that ΔEAdi corrects for larger interbreath differences in neural drive. Hence, it has yet to be determined whether the EAdi should be used to either correct or limit for changes in neural efforts between assisted and non-assisted breaths. In critically ill patients with increased variability in Vt and ΔEAdi [26] there may be a need for several breaths to ensure representative measures of Vt and ΔEAdi. In humans, Viale et al. showed that several breaths are required for the respiratory drive to adjust after changing assist level [27].
It is important to keep in mind the close sensory-motor control of NAVA. As demonstrated in the present and other studies, increasing the NAVA level normally reduces the EAdi while Vtinsp is increasing or remains at a plateau [24, 25, 28]: thus for the non-assisted breath both Vtinsp and EAdi decrease and the Vtinsp/EAdi ratio remains relatively constant, whereas for the assisted breath, increased or maintained Vtinsp, decreased EAdi and improved Vtinsp/EAdi ratio (see Figs. 1, 3). Accordingly, the PVBC will decrease with increasing assist (Fig. 3). On the other hand, if the NAVA level is constant and the patient’s Vtinsp for a given EAdi improves, the patient’s breath contribution improves while that of the ventilator does not. Hence the PVBC index improves as a consequence of improved respiratory function. This new ability to study the sharing of respiratory efforts between patient and ventilator following both adjustments of the NAVA level and changes in the respiratory status opens new possibilities for studies of adjusting assist levels to optimize weaning.
Conclusions
This study shows, in an animal model of ALI and severe airflow obstruction, that measurements of inspiratory volume and diaphragm electrical activity during a simple maneuver—removing the assist for one breath and comparing it to the previous assisted breath—allows quantification of the relative contribution of the inspiratory muscles versus the ventilator to the tidal volume. If clinically applicable, this index could serve to help quantify and standardize the adjustment of the level of assist. Further studies are required to evaluate if this method is clinically applicable.
References
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 131:711–717
Kondili E, Prinianakis G, Alexopoulou C, Vakouti E, Klimathianaki M, Georgopoulos D (2006) Respiratory load compensation during mechanical ventilation–proportional assist ventilation with load-adjustable gain factors versus pressure support. Intensive Care Med 32:692–699
Brochard L, Harf A, Lorino H, Lemaire F (1989) Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis 139:513–521
Tobin MJ, Laghi F, Jubran A (2010) Narrative review: ventilator-induced respiratory muscle weakness. Ann Intern Med 153:240–245
Jaber S, Jung B, Matecki S, Petrof BJ (2011) Clinical review: ventilator-induced diaphragmatic dysfunction—human studies confirm animal model findings! Crit Care 15:206
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindström L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Zakynthinos SG, Vassiliakopoulos T, Zakynthinos E, Roussos C, Tzelepis GE (1999) Correcting static intrinsic positive end-expiratory pressure for expiratory muscle contraction. Validation of a new method. Am J Respir Crit Care Med 160:785–790
Bennet FM, Tenney SM (1982) Comparative mechanics of mammalian respiratory system. Respir Physiol 49:131–140
Mantilla CB, Seven YB, Zhan WZ, Sieck GC (2010) Diaphragm motor unit recruitment in rats. Respir Physiol Neurobiol 173:101–106
D’Angelo E, Monaco A, D’Angelo E, Pecchiari M (2010) Motor control of the diaphragm in anesthetized rabbits. Respir Physiol Neurobiol 170:141–149
Johnson RL Jr, Hsia CC, Takeda S, Wait JL, Glenny RW (2002) Efficient design of the diaphragm: distribution of blood flow relative to mechanical advantage. J Appl Physiol 93:925–930
Sinderby C, Beck J, Spahija J, Weinberg J, Grassino A (1998) Voluntary activation of the human diaphragm in health and disease. J Appl Physiol 85:2146–2158
Beck J, Gottfried SB, Navalesi P, Strobik Y, Comtois N, Rossini M, Sinderby C (2001) Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med 164:419–424
Cohen CA, Zagelbaum G, Gross D, Roussos C, Macklem PT (1982) Clinical manifestations of inspiratory muscle fatigue. Am J Med 73:308–316
Aliverti A, Cala SJ, Duranti R, Ferrigno G, Kenyon CM, Pedotti A, Scano G, Sliwinski P, Macklem PT, Yan S (1997) Human respiratory muscle actions and control during exercise. J Appl Physiol 83:1256–1269
Finucane KE, Singh B (2009) Human diaphragm efficiency estimated as power output relative to activation increases with hypercapnic hyperpnea. J Appl Physiol 107:1397–1405
Yan S, Lichros I, Zakynthinos S, Macklem PT (1993) Effect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathing. J Appl Physiol 75:1364–1370
De Troyer A (2005) Interaction between the canine diaphragm and intercostal muscles in lung expansion. J Appl Physiol 98:795–803
Beck J, Sinderby C, Lindstrom L, Grassino A (1998) Crural diaphragm activation during dynamic contractions at various inspiratory flow rates. J Appl Physiol 85:451–458
Beck J, Sinderby C, Lindstrom L, Grassino A (1998) Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol 85:1123–1134
De Troyer A, Borenstein S, Cordier R (1980) Analysis of lung volume restriction in patients with respiratory muscle weakness. Thorax 35:603–610
Sinderby C, Weinberg J, Sullivan L, Borg J, Lindström L, Grassino A (1996) Diaphragm function in patients with cervical cord injury or prior poliomyelitis infection. Spinal Cord 34:204–213
Jolley CJ, Luo YM, Steier J, Reilly C, Seymour J, Lunt A, Ward K, Rafferty GF, Polkey MI, Moxham J (2009) Neural respiratory drive in healthy subjects and in COPD. Eur Respir J 33:289–297
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS, Sinderby C (2009) Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest 135:695–702
Lecomte F, Brander L, Jalde F, Beck J, Qui H, Elie C, Slutsky AS, Brunet F, Sinderby C (2009) Physiological response to increasing levels of neurally adjusted ventilatory assist (NAVA). Resp Physiol Neurobiol 166:117–124
Patroniti N, Bellani G, Saccavino E, Zanella A, Grasselli G, Isgrò S, Milan M, Foti G, Pesenti A (2012) Respiratory pattern during neurally adjusted ventilatory assist in acute respiratory failure patients. Intensive Care Med 38:230–239
Viale JP, Duperret S, Mahul P, Delafosse B, Delpuech C, Weismann D, Annat G (1998) Time course evolution of ventilatory responses to inspiratory unloading in patients. Am J Resp Crit Care Med 157:428–434
Allo JC, Beck J, Brander L, Brunet F, Slutsky AS, Sinderby CA (2006) Influence of neutrally adjusted ventilatory assist and positive end-expiratory pressure on breathing pattern in rabbits with acute lung injury. Crit Care Med 34:2997–3004
Acknowledgments
The authors wish to thank M. Norman Comtois for his technical assistance. CS was supported by the RS McLaughlin Foundation.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grasselli, G., Beck, J., Mirabella, L. et al. Assessment of patient–ventilator breath contribution during neurally adjusted ventilatory assist. Intensive Care Med 38, 1224–1232 (2012). https://doi.org/10.1007/s00134-012-2588-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2588-y