Abstract
Objective
Neurally adjusted ventilatory assist (NAVA) is a new mode wherein the assistance is provided in proportion to diaphragm electrical activity (EAdi). We assessed the physiologic response to varying levels of NAVA and pressure support ventilation (PSV).
Setting
ICU of a University Hospital.
Patients
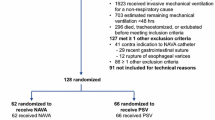
Fourteen intubated and mechanically ventilated patients.
Design and protocol
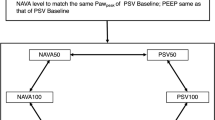
Cross-over, prospective, randomized controlled trial. PSV was set to obtain a V t/kg of 6–8 ml/kg with an active inspiration. NAVA was matched with a dedicated software. The assistance was decreased and increased by 50% with both modes. The six assist levels were randomly applied.
Measurements
Arterial blood gases (ABGs), tidal volume (V t/kg), peak EAdi, airway pressure (Paw), neural and flow-based timing. Asynchrony was calculated using the asynchrony index (AI).
Results
There was no difference in ABGs regardless of mode and assist level. The differences in breathing pattern, ventilator assistance, and respiratory drive and timing between PSV and NAVA were overall small at the two lower assist levels. At the highest assist level, however, we found greater V t/kg (9.1 ± 2.2 vs. 7.1 ± 2 ml/kg, P < 0.001), and lower breathing frequency (12 ± 6 vs. 18 ± 8.2, P < 0.001) and peak EAdi (8.6 ± 10.5 vs. 12.3 ± 9.0, P < 0.002) in PSV than in NAVA; we found mismatch between neural and flow-based timing in PSV, but not in NAVA. AI exceeded 10% in five (36%) and no (0%) patients with PSV and NAVA, respectively (P < 0.05).
Conclusions
Compared to PSV, NAVA averted the risk of over-assistance, avoided patient–ventilator asynchrony, and improved patient–ventilator interaction.




Similar content being viewed by others
References
Younes M (1991) Proportional assist ventilation and pressure support ventilation: similarities and differences. In: Marini J, Roussos C (eds) Ventilatory failure. Springer, Berlin, pp 361–380
Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M (1997) Patient–ventilator trigger asynchrony in prolonged mechanical ventilation. Chest 112:1592–1599
Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L (2006) Patient–ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med 32:1515–1522
Cereda M, Foti G, Marcora B, Gili M, Giacomini M, Sparacino ME, Pesenti A (2000) Pressure support ventilation in patients with acute lung injury. Crit Care Med 28:1269–1275
Nava S, Bruschi C, Fracchia C, Braschi A, Rubini F (1997) Patient-ventilator interaction and inspiratory effort during pressure support ventilation in patients with different pathologies. Eur Respir J 10:177–183
Younes M, Kun J, Webster K, Roberts D (2002) Response of ventilator-dependent patients to delayed opening of exhalation valve. Am J Respir Crit Care Med 166:21–30
Leung P, Jubran A, Tobin MJ (1997) Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am J Respir Crit Care Med 155:1940–1948
Younes M, Puddy A, Roberts D, Light RB, Quesada A, Taylor K, Oppenheimer L, Cramp H (1992) Proportional assist ventilation. Results of an initial clinical trial. Am Rev Respir Dis 145:121–129
Giannouli E, Webster KIM, Roberts DAN, Younes M (1999) Response of ventilator-dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med 159:1716–1725
Nava S, Bruschi C, Rubini F, Palo A, Iotti G, Braschi A (1995) Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med 21:871–879
Appendini L, Purro A, Patessio A, Zanaboni S, Carone M, Spada E, Donner CF, Rossi A (1996) Partitioning of inspiratory muscle workload and pressure assistance in ventilator-dependent COPD patients. Am J Respir Crit Care Med 154:1301–1309
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Navalesi P, Costa R (2003) New modes of mechanical ventilation: proportional assist ventilation, neurally adjusted ventilatory assist, and fractal ventilation. Curr Opin Crit Care 9:51–58
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G (2006) Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 354:1775–1786
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 131:711–717
Aldrich T, Sinderby C, McKenzie D (2002) Electrophysiologic techniques for the assessment of respiratory muscle function. In: ATS/ERS (eds) Statement on respiratory muscle testing. Am J Respir Crit Care Med 166:518–624
Allo JC, Beck JC, Brander L, Brunet F, Slutsky AS, Sinderby CA (2006) Influence of neurally adjusted ventilatory assist and positive end-expiratory pressure on breathing pattern in rabbits with acute lung injury. Crit Care Med 34:2997–3004
Foti G, Cereda M, Banfi G, Pelosi P, Fumagalli R, Pesenti A (1997) End-inspiratory airway occlusion: a method to assess the pressure developed by inspiratory muscles in patients with acute lung injury undergoing pressure support. Am J Respir Crit Care Med 156:1210–1216
(2006) Ventilate with NAVA. In: AB MCC (eds) SERVO-I V32 NAVA ventilation, user’s manual
Fauroux B, Isabey D, Desmarais G, Brochard L, Harf A, Lofaso F (1998) Nonchemical influence of inspiratory pressure support on inspiratory activity in humans. J Appl Physiol 85:2169–2175
Ramsay MA, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with alphaxalone–alphadolone. Br Med J 2:656–659
Tobin MJ, Mador MJ, Guenther SM, Lodato RF, Sackner MA (1988) Variability of resting respiratory drive and timing in healthy subjects. J Appl Physiol 65:309–317
Wrigge H, Golisch W, Zinserling J, Sydow M, Almeling G, Burchardi H (1999) Proportional assist versus pressure support ventilation: effects on breathing pattern and respiratory work of patients with chronic obstructive pulmonary disease. Intensive Care Med 25:790–798
Vitacca M, Bianchi L, Zanotti E, Vianello A, Barbano L, Porta R, Clini E (2004) Assessment of physiologic variables and subjective comfort under different levels of pressure support ventilation. Chest 126:851–859
Berger KI, Sorkin IB, Norman RG, Rapoport DM, Goldring RM (1996) Mechanism of relief of tachypnea during pressure support ventilation. Chest 109:1320–1327
Ambrosino N (1999) Apples and oranges. Comparing different modalities of mechanical ventilation. Intensive Care Med 25:775–777
Yamada Y, Du HL (2000) Analysis of the mechanisms of expiratory asynchrony in pressure support ventilation: a mathematical approach. J Appl Physiol 88:2143–2150
Sassoon CS, Foster GT (2001) Patient–ventilator asynchrony. Curr Opin Crit Care 7:28–33
Kondili E, Prinianakis G, Anastasaki M, Georgopoulos D (2001) Acute effects of ventilator settings on respiratory motor output in patients with acute lung injury. Intensive Care Med 27:1147–1157
Acknowledgments
We thank Maquet Critical Care that provided us with all the equipment used for the study. We are indebted to Jeffrey Franc-Law who carefully revised the manuscript. Last but not least, we wish to acknowledge all physicians and nurses of our Intensive Care Unit for their helpful and continuous support.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-008-1215-4.
Rights and permissions
About this article
Cite this article
Colombo, D., Cammarota, G., Bergamaschi, V. et al. Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med 34, 2010–2018 (2008). https://doi.org/10.1007/s00134-008-1208-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1208-3