Abstract
Objective
Neonatal asphyxia causes cardiogenic shock and pulmonary hypertension with decreased brain perfusion. We examined the dose-response of milrinone on systemic, pulmonary, and carotid circulations in a model of neonatal hypoxia-reoxygenation.
Design and setting
Controlled, block-randomized study in a university research laboratory.
Subjects
Mixed breed piglets (1–3 days, 1.5–2.3 kg).
Interventions
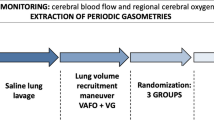
In acutely instrumented piglets normocapnic alveolar hypoxia (10–15% oxygen) was induced for 2 h followed by reoxygenation with 100% oxygen (1 h) then 21% oxygen (3 h). At 2 h of reoxygenation after a volume loading (10 ml/kg) either saline or milrinone (bolus and infusion at 0.25, 0.5, or 0.75 μg/kg per minute) was given for 2 h in a blinded-randomized fashion (n = 7/group).
Measurements and results
All milrinone-treated groups had higher cardiac output and stroke volume than those of saline-treated hypoxic controls, which showed progressive decline in these measurements. At 2 h of infusion plasma milrinone levels were significantly correlated with cardiac output (r = 0.6), which increased from pretreatment value in the group receiving 0.75 μg/kg per minute. Milrinone maintained mean arterial pressure; heart rate and pulmonary arterial pressure did not differ between groups. Milrinone prevented continued increases in systemic and pulmonary vascular resistances after hypoxia-reoxygenation. Milrinone infusion at higher doses increased common carotid flow. Milrinone-treated piglets had increased systemic and carotid oxygen delivery, with no difference in plasma and myocardial lactate levels among groups.
Conclusions
When used to treat shock in newborn piglets with hypoxia-reoxygenation, milrinone improved cardiac output and carotid flow while maintaining systemic blood pressure. Pulmonary hypertension was not aggravated. Further studies are needed to confirm these findings in asphyxiated neonates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe neonatal hypoxia can lead to left ventricular myocardial dysfunction. These sick neonates may have decreased blood flow and oxygen delivery to vital organs leading to significant morbidity and mortality [1]. Following resuscitation with 100% oxygen asphyxiated neonates are exposed to oxygen-derived free radicals and commonly have further reduced myocardial contractility and pulmonary vasoconstriction with low cardiac output (CO), systemic hypotension, and pulmonary hypertension (PHT) [1–4].
Current treatments for hypotension in asphyxiated neonates include catecholamines such as dopamine, epinephrine, and dobutamine. The stimulation of adrenoceptors by catecholamines may be associated with tachycardia, arrhythmias, vasoconstriction, fluctuating blood pressures, aggravating PHT, and increased oxygen consumption, despite inotropic effects [5–7]. The inotrope, milrinone, is a specific phosphodiesterase III inhibitor that increases myocardial contractility by elevating the intracellular cyclic adenosine monophosphate concentration through inhibiting cyclic adenosine monophosphate degradation [8]. Phosphodiesterase III inhibitors may also improve diastolic dysfunction [9], cause vasodilation [5, 10, 11], but not affect myocardial oxygen consumption [11, 12]. To date the effects of milrinone have been examined in neonates who had low CO after cardiac surgery, preterm infants at risk for low systemic blood flow, and those with unresponsive PHT [11, 13–16]. Although management strategies for these patients are similar to those for hypoxic neonates including improving cardiac function and pulmonary hemodynamics [17], doses of milrinone used and hemodynamic parameters measured are variable in these studies. To our knowledge, there is no information on the systemic and regional hemodynamic effects of milrinone in hypoxic neonates.
Using a swine model of neonatal hypoxia and reoxygenation (H-R), we primarily examined the dose-response effects of milrinone on CO and systemic blood pressure. The secondary objectives included the effects of milrinone on the pulmonary and carotid circulations as well as oxygen transport. We hypothesized that milrinone would dose-dependently improve the H-R induced cardiac dysfunction and increase blood flow to the brain without aggravating PHT and with minimal effect on systemic blood pressure in H-R piglets.
Materials and methods
Animal preparation
Mixed breed piglets aged 1–3 days (mean 2.0 ± 0.2) and weighing 1.5–2.3 kg (mean 1.86 ± 0.04). Four piglets were euthanised prematurely due to complications secondary to surgery (two) or severe hypoxia (two). The protocol followed the 1993 guidelines of the Canadian Council on Animal Care and was approved by the institutional Health Sciences Animal Welfare Committee. Animal preparation and H-R protocol have been previously described [7, 18]. Briefly, the piglets were anesthetized with halothane, which was then switched to intravenous midazolam (0.1–0.2 mg kg−1 h−1), fentanyl (5–15 μg kg−1 h−1), and pancuronium (0.05–0.1 mg kg−1 h−1) to provide anesthesia, analgesia, and paralysis, respectively. Fractional inspired oxygen concentration (FIO2) of 0.21–0.24 kept oxygen saturations between 90–100% as measured by pulse oximetry (Nellcor, Hayward, CA, USA). Infusions of 10% dextrose (10 ml kg−1 h−1, venous) and of 0.9% normal saline (2 ml kg−1 h−1, arterial) were maintained during the experiment. Through femoral vessels 5-F Argyle catheters (Sherwood Medical, St Louis, MO, USA) were inserted to the level of right atrium and another into the infrarenal aorta to measure central venous pressure, deliver fluids and medications, and measure mean arterial pressure (MAP). Endotracheal intubation via a tracheostomy allowed mechanical ventilation (ventilator model IV-100, Sechrist Industries, Anaheim, CA, USA) at a rate of 18–20 breaths/min and pressure of 19/4 cmH2O.
The left common carotid artery was encircled by a 2-mm Transonic flow probe (2SS, Transonic Systems, Ithaca, NY, USA) to measure blood flow. Through a left anterior thoracotomy the main pulmonary artery was exposed and cannulated with a 20-G Arrow catheter (Arrow International, Reading, PA, USA) to measure pulmonary arterial pressure (PAP). A 6-mm Transonic flow probe (6SB) was placed to monitor the blood flow as a surrogate of CO. The ductus arteriosus was ligated. Incisions were covered and kept moist to minimize evaporative losses. Body temperature was kept at 38.5–39.5 °C. Hemodynamic data were recorded and digitized by a DT2801-A analogue to digital converter board (Data Translation, ON, Canada) in a Dell 425E computer equipped with custom Asyst programming software.
Hypoxia-reoxygenation and treatment procedure
Piglets were block-randomized to four groups (n = 7/group) which underwent H-R; a sham-operated group (n = 4) had no H-R or medication delivery. There were no differences among groups regarding age, weight, mortality, or hemodynamic variables at normoxic baseline. After instrumentation the animals underwent a stabilization period for at least 40 min. Arterial PCO2 was maintained between 35–45 mmHg during the experimental period. Alveolar hypoxia was initiated with the inhalation of an oxygen/nitrogen gas mixture to provide an FIO2 of 0.10–0.15 for a PaO2 of 20–40 mmHg for 2 h. Piglets were then reoxygenated with 100% oxygen for 1 h and a further 3 h of 21% oxygen. Previous studies have determined that in this piglet model this degree of hypoxemia produces clinical hypoxia followed by significant cardiac dysfunction and systemic hypotension at 2 h of reoxygenation [7, 18]. All piglets received a 10 ml/kg lactated Ringer's bolus 30 min prior to medication delivery. At 2 h of reoxygenation piglets received an intravenous infusion of either placebo (normal saline) or milrinone (Pharmaceutical Partners of Canada, Richmond Hill, ON, Canada) at low dose (25 μg/kg loading, 0.25 μg kg−1 min−1 infusion), medium dose (50 μg/kg, 0.50 μg kg−1 min−1), or high dose (75 μg/kg, 0.75 μg kg−1 min−1) at a constant dose rate for 2 h in a blinded-randomized fashion. The drug administration was given at 6.7 ml/kg/h for 15 min (medication loading bolus) followed by 1 ml kg−1 h−1 for 2 h.
Hemodynamic and oxygen transport measurements
Heart rate, MAP, PAP, central venous pressure, pulmonary artery and left common carotid artery blood flows were recorded at normoxic baseline (0 min), at 2 h of hypoxia (120 min), at 0.5 h of reoxygenation (150 min) and 2 h of reoxygenation (240 min, pretreatment baseline), and every 30 min following medication or placebo delivery. Variables were calculated as a mean over 2 min at these time points. Simultaneous arterial and venous blood samples were taken for blood gas analyses by ABL500 and OSM3 Hemoximeter (Radiometer, Copenhagen, Denmark). To assess milrinone loading stability the highest and lowest hemodynamic parameters were recorded throughout the 15 min loading of medication. Hemodynamic variables were indexed for piglet weight. Pulmonary vascular resistance (VR) was estimated by PAP ÷ CO because the left atrial pressure was not measured.
Plasma lactate, troponin-I, and milrinone levels determination
Arterial plasma samples were prepared and stored at −80 °C until assay. Plasma lactate was analyzed at 0, 120, 240, and 360 min by enzyme-coupled NADH colorimetry method with spectrophotometry at 340 nm [19]. In hypoxic control and high-dose milrinone-treated groups, plasma levels of porcine cardiac-specific troponin-I were determined at 0 and 360 min using enzyme-linked immunosorbent assay (#2010-4, Life Diagnostics, West Chester, PA, USA). Using a high-performance liquid chromatographic validated method [20], plasma milrinone was determined with standards (0–2000 ng/ml) for calibration. The limit of quantification was 5 ng/ml.
Left ventricle myocardial lactate determination and histopathological examination
At study end the piglets were euthanised with intravenous pentobarbital (100 mg/kg). Left ventricle samples were snap-frozen in liquid nitrogen and stored at −80 °C whereas another sample was fixed in 10% formalin for biochemical and histopathological analysis, respectively. Frozen heart tissue (50 mg) was crushed at −80 °C, homogenized in 6% perchloric acid/0.5 mM EGTA (50 μl) on ice, and centrifuged (11,000 rpm, 2 min, 4 °C). The supernatant was weighed, 5 M potassium carbonate added (ratio 1:10 supernatant), precipitated on ice for 30 min, then centrifuged (11,000 rpm, 2 min). The supernatant was then used for lactate determination as described above. The formalin preserved specimen was stained with hematoxylin and eosin. Two pathologists (J.L., C.G.) unaware of group assignment evaluated the specimens. Pathological injury was graded based on previously established criteria [21].
Statistics
Results are expressed as mean ± SEM. Using α < 0.05 and β < 0.2, a sample size (n = 7/group) was estimated to demonstrate a statistically significant difference in CO between groups based on our previous experience [7, 18]. Hemodynamic variables were analyzed by two-way repeated measures analysis of variance or analysis of variance on ranks (Kruskal-Wallis) if normality test failed. Biochemical variables were analyzed by one-way analysis of variance. Pearson's moment correlation was used to determine the relationship between hemodynamic variables and milrinone levels. Analysis was performed using Sigma Stat (version 2.0, Jandel Scientific, San Rafael, CA, USA).
Results
2 h of hypoxia and 2 h of reoxygenation
Two hours of normocapnic alveolar hypoxia (PaO2 34 ± 1 mmHg, FIO2 0.129 ± 0.003) resulted in metabolic acidosis with pH 7.04 ± 0.04 and plasma lactate levels of 15.2 ± 0.4 mmol/. Hypoxia significantly reduced the CO to 71 ± 4 ml kg−1 min−1 with hypotension (MAP of 28 ± 2 mmHg; 41 ± 1% and 41 ± 2% of normoxic baseline, respectively; Figs. 1a, 2a, Table 1). The stroke volume was significantly decreased to 41 ± 3% of normoxic baseline (Fig. 1b). During hypoxia PAP initially increased. At 2 h of hypoxia PAP subsequently decreased to 31 ± 1 mmHg (128 ± 6% of normoxic baseline; Fig. 2b), whereas pulmonary VR progressively increased (315 ± 16% of normoxic baseline). Carotid artery blood flow (CAF) was 14 ± 1 ml kg−1 min−1 (66 ± 5% of normoxic baseline; Fig. 3).
The effect of milrinone infusion on cardiac output (a), stroke volume (b), and heart rate (c) in newborn piglets during hypoxia and reoxygenation compared to hypoxic controls (open circles): filled circles 0.25 μg kg−1 min−1; filled triangles 0.50; filled squares 0.75 (n = 7 per group); # p < 0.05 individual group vs. normoxic baseline (0 min); ## p < 0.05 groups vs. normoxic baseline; § p < 0.05 vs. pretreatment baseline (240 min); * p < 0.05 individual milrinone group vs. hypoxic controls; ** p < 0.05 all milrinone groups vs. hypoxic controls; † p = 0.07 high-dose vs. medium-dose and low-dose milrinone groups
The effect of milrinone infusion on mean arterial pressure (a) and mean pulmonary arterial pressure (b) in newborn piglets during hypoxia and reoxygenation compared to hypoxic controls (open circles): filled circles 0.25 μg kg−1 min−1; filled triangles 0.50; filled squares 0.75 (n = 7 per group); ## p < 0.05 all groups vs. normoxic baseline (0 min); Note: the administration of milrinone maintained the mean arterial pressure without causing significant hypotension
The effect of milrinone infusion on carotid artery flow in newborn piglets during hypoxia and reoxygenation compared to hypoxic controls (open circles): filled circles 0.25 μg kg−1 min−1; filled triangles 0.50; filled squares 0.75 (n = 7 per group); # p < 0.05 individual group vs. normoxic baseline (0 min); ## p < 0.05 all groups vs. normoxic baseline; § p < 0.05 vs. pretreatment baseline (240 min); * p < 0.05 individual milrinone group vs. hypoxic controls; † p = 0.09 individual milrinone group vs. hypoxic controls; ‡ p < 0.05 high-dose vs. low-dose milrinone group
Upon reoxygenation with 100% oxygen (PaO2 404 ± 16 mmHg) systemic and regional hemodynamics immediately recovered to baseline within 10 min (data not shown). At 2 h of reoxygenation (PaO2 61 ± 1 mmHg, pH 7.38 ± 0.01) MAP fell to 67 ± 3%, CO to 75 ± 3%, and CAF to 79 ± 3% of the respective normoxic baseline (all p < 0.05; Figs. 1, 2, 3). Pulmonary VR was higher and systemic VR was lower than the respective normoxic baseline (142 ± 5% and 85 ± 5%, respectively; both p < 0.05). Stroke volume but not heart rate was significantly diminished (67 ± 3% of normoxic baseline; Fig. 1b, c).
No significant differences in hemodynamic and physiological parameters were found between groups at the end of hypoxia and after 2 h of reoxygenation prior to medication delivery. Normoxic sham-operated piglets showed no significant change in hemodynamic and physiological parameters throughout the experimental period.
Systemic hemodynamics after milrinone or placebo infusion
The loading dose of milrinone did not cause significant changes in CO, heart rate, MAP, PAP, and CAF or arrhythmias. All milrinone-treated groups had higher CO and stroke volume after 2 h of infusion than placebo-treated hypoxic controls (p < 0.001 and p = 0.01, respectively; Fig. 1a, b). In hypoxic controls CO significantly decreased further over the next 2 h, but it was maintained in the low and medium-dose milrinone-treated groups and significantly increased over pretreatment baseline to a value not significantly different from normoxic baseline after high-dose milrinone infusion. The heart rate was not different between groups during infusion (Fig. 1c). Mean arterial pressure was not affected with milrinone infusion (vs. hypoxic controls or pretreatment baseline, both p > 0.05; Fig. 2a). Systemic VR remained low in the high-dose and medium-dose milrinone-treated groups compared to the continued increase found in hypoxic controls (0.26 ± 0.01 and 0.27 ± 0.01 vs. 0.37 ± 0.04 mmHg ml−1 kg−1 min−1, respectively, p < 0.05).
Pulmonary hemodynamics after milrinone or placebo infusion
No effect was found on PAP during milrinone infusion (vs. hypoxic controls or pretreatment baseline, both p > 0.05; Fig. 2b). At 4 h of reoxygenation there was a continued increase in pulmonary VR in hypoxic controls (0.37 ± 0.03 vs. 0.16 ± 0.02 mmHg ml−1 kg−1 min−1 at normoxic baseline, p < 0.05) while pulmonary VR of milrinone-treated animals remained significantly lower than hypoxic controls (0.20 ± 0.02, 0.20 ± 0.02, and 0.24 ± 0.02 mmHg ml−1 kg−1 min−1 for high-dose, medium-dose, and low-dose milrinone-treated groups, respectively, p < 0.05).
Carotid hemodynamics after milrinone or placebo infusion
CAF of hypoxic controls was significantly lower than normoxic baseline after 4 h of reoxygenation (Fig. 3). High-dose milrinone infusion increased CAF significantly (vs. hypoxic controls or pretreatment baseline, both p < 0.05) and the effect of medium-dose milrinone infusion was modest (p = 0.09, β = 0.4; Fig. 3). No significant change in the carotid VR was found (data not shown).
Oxygen transport after milrinone or placebo infusion
Compared to hypoxic controls, all milrinone-treated groups had higher systemic oxygen delivery (Fig. 4a) and consumption (6.3 ± 0.4, 6.3 ± 0.2, and 5.6 ± 0.5 ml O2 kg−1 min−1 in high-dose, medium-dose, and low-dose milrinone-treated groups vs. 3.8 ± 0.4 ml O2 kg−1 min−1 in hypoxic controls, respectively, p < 0.05). Carotid artery oxygen delivery was higher in high-dose and medium-dose milrinone groups (vs. hypoxic controls, p < 0.05; Fig. 4b). High-dose milrinone increased carotid oxygen delivery over pretreatment baseline (p < 0.05). There was no difference in plasma lactate levels at 2 h of infusion between groups (3.0 ± 0.4, 2.7 ± 0.3, and 2.8 ± 0.7 mmol/l in low-dose, medium-dose, and high-dose milrinone-treated groups vs. 4.7 ± 1.1 mmol/l in hypoxic controls, respectively).
The effect of milrinone infusion on systemic oxygen delivery (a) and carotid artery oxygen delivery (b) in newborn piglets during hypoxia and reoxygenation compared to hypoxic controls (open circles): filled circles 0.25 μg kg−1 min−1; filled triangles 0.50; filled squares 0.75 (n = 7 per group); # p < 0.05 individual group vs. normoxic baseline (0 min); ## p < 0.05 all groups vs. normoxic baseline; § p < 0.05 vs. pretreatment baseline (240 min); * p < 0.05 individual milrinone group vs. hypoxic controls; ** p < 0.05 all milrinone groups vs. hypoxic controls; ‡ p < 0.05 high-dose vs. low-dose milrinone group
Plasma milrinone levels
Dose-response on plasma milrinone levels after 2 h of treatment was observed (Fig. 5). Plasma milrinone levels were correlated with CO (r = 0.6, n = 28, p < 0.001; r = 0.9, n = 4 mean plasma levels and mean CO, p = 0.05). Modest correlations were found between milrinone levels and stroke volume, CAF, and carotid oxygen delivery (all r = 0.5, p < 0.05). Significant correlations were found between milrinone levels and VR (systemic, pulmonary, carotid: all r = −0.6, p < 0.05).
Boxplot showing the plasma milrinone concentrations in low-dose, medium-dose, and high-dose milrinone groups (0.25, 0.50, and 0.75 μg kg−1 min−1, respectively); Median, 25th and 75th percentiles, 95% confidence limits, and outliners are shown; * p < 0.05 vs. low-dose group; ‡ p < 0.05 vs. medium-dose group
Plasma troponin-I levels and cardiac tissue analysis
Significantly higher plasma troponin-I levels were found at 4 h of reoxygenation compared to normoxic baseline (0.71 ± 0.17 and 0.48 ± 0.18 ng/ml for hypoxic controls and high-dose milrinone-treated group vs. 0.09 ± 0.01 ng/ml at normoxic baseline, respectively). There were no significant differences in troponin-I levels between groups. There were no significant differences in cardiac left ventricle histopathology or tissue lactate levels between groups (data not shown). None of the myocardial tissue samples demonstrated prominent ischemic changes or overt necrosis.
Discussion
In this swine model of neonatal H-R we demonstrated the dose-related response of milrinone on systemic and carotid perfusion after hypoxia. All doses of milrinone did not cause significant hypotension or worsen PHT. Milrinone prevented the progressive increases in systemic and pulmonary VR found in hypoxic controls. In the absence of significant chronotropy it is plausible that milrinone improves aspects of systolic-diastolic cardiac function as well as left ventricular preload and afterload.
Systemic hemodynamic effects of milrinone
Neonatal asphyxia induces cardiovascular dysfunction with reduced myocardial contractility and passive dilation leading to cardiac stunning and systemic hypotension [1, 3]. This low CO state, similar to that in neonates after cardiac surgery, is evidenced by the continual decrease in cardiac function in the hypoxic control group. Doppler echocardiography in neonates has demonstrated that milrinone improved low CO with a direct myocardial effect [22]. We demonstrated the dose-response of milrinone on CO and further showed the significant correlation between cardiac variables and plasma milrinone levels, which is consistent with that in children after cardiac surgery [12, 23]. Interestingly, we found the cardiovascular effect with high-dose milrinone at plasma milrinone levels in H-R piglets (Fig. 5) that were substantially lower than the level of 180–300 ng/ml reported in studies in human subjects, although a hemodynamic effect at these levels is yet to be shown in preterm infants with low systemic blood flow [13]. Milrinone pharmacokinetics may be different in various pediatric populations and indications. Our lower levels may reflect subtle differences in the pathopharmacology of low CO syndrome between H-R and postcardiopulmonary bypass patients, different pharmacokinetics between piglets and human neonates, and the short administration to reach steady state.
We did not observe any significant effect on the heart rate and MAP during milrinone infusion. The chronotropic effect of milrinone may have been masked by the tachycardia during neonatal H-R [24] or ameliorated by the preceding fluid bolus. MAP during milrinone infusion has been found to be maintained [11, 25] or decreased [5, 11, 13]. Adequate volume status coupled with increased CO most likely helped to maintain MAP despite decreased systemic VR. The cardiac effect of milrinone was not associated with increased myocardial oxygen consumption [11, 12]. Although we did not measure coronary hemodynamics or perfusion, there was no significant increase in myocardial tissue lactate or any evidence of histological features of ischemic changes or H-R damage in the milrinone-treated groups compared to hypoxic controls in this short-term (2 h) infusion.
Pulmonary hemodynamics effects of milrinone
Neonatal hypoxia can lead to PHT, which has been previously demonstrated in this model of H-R [7, 26, 27]. Three case series recently reported milrinone use in neonates with unresponsive PHT and the drug's ability to increase ventricular output and decrease pulmonary VR [14–16]. The current study showed that milrinone might have a dose-related ability to prevent elevations in pulmonary VR, which is inversely correlated with the plasma milrinone level, with no significant change in PAP. In the current study left atrial pressure was not measured (due to increased mortality), and therefore pulmonary VR was an estimated parameter. Enhanced pulmonary arterial flow with milrinone infusion did not cause PHT exacerbation as seen in vasopressive doses of epinephrine or dopamine [28, 29].
Carotid hemodynamics and oxygen delivery
Cerebral blood flow is often impaired in hypoxic infants [30], even after resuscitation when blood pressure and oxygenation normalized [31, 32]. Milrinone at 250 μg/kg increased cerebral blood flow when given to hypoxic adult dogs [33]. We found that high-dose milrinone (0.75 μg kg−1 min−1) was more effective than lower doses at improving CAF, which has been shown to be correlated with cerebral blood flow (r = 0.84) in animal models of H-R [34]. Without significant effects found on the carotid VR peripheral VR but not MAP may be important for regional blood flow after hypoxia [35, 36].
Limitations
There are recognizable limitations in this study although piglets have similar pathophysiological responses to H-R as human neonates [37, 38]. To estimate CO we assumed negligible transatrial shunt during H-R with ductus arteriosus ligated. Unlike asphyxia, hypoxemia and acidemia was controlled in the presence of normocapnia. Our study model approximates the clinical scenario of neonatal hypoxia but is distinct from perinatal asphyxia [39]. Nonetheless, the piglets were hypotensive with cardiovascular dysfunction and decreased carotid flow after H-R. The piglet's pharmacodynamics of milrinone is unknown. Oxidative stress is related to the cardiovascular dysfunction after H-R; thus, measuring oxygen-derived free radicals production with milrinone would also be beneficial for future research. Given the short duration of the model, subsequent low plasma milrinone levels, and gross nature of the biochemical and histological examination, further long-term studies of milrinone infusions looking at beneficial and detrimental effects are needed.
In conclusion, in a swine model of neonatal H-R, milrinone improved CO and carotid flow without causing significant hypotension or aggravating PHT. Given these encouraging results, clinical investigation and further studies to compare milrinone with currently used inotropes in asphyxiated neonates are warranted.
References
van Bel F, Walther FJ (1990) Myocardial dysfunction and cerebral blood flow velocity following birth asphyxia. Acta Paediatr Scand 79:756–762
Osborn D, Evans N, Kluckow M (2004) Diagnosis and treatment of low systemic blood flow in preterm infants. Neoreviews 5:e109–e121
Leuthner SR, Das UG (2004) Low Apgar scores and the definition of birth asphyxia. Pediatr Clin North Am 51:737–745
Evans N, Kluckow M, Currie A (1998) Range of echocardiographic findings in term neonates with high oxygen requirements. Arch Dis Child Fetal Neonatal Ed 78:F105–F111
Chatterjee K, De Marco T (2003) Role of nonglycoside inotropic agents: indications, ethics and limitations. Med Clin North Am 87:391–418
Penny DJ, Sano T, Smolich JJ (2001) Increased systemic oxygen consumption offsets improved oxygen delivery during dobutamine infusion in newborn lambs. Intensive Care Med 27:1518–1525
Al-Salam Z, Johnson ST, Abozaid S, Bigam D, Cheung PY (2007) The hemodynamic effects of dobutamine during reoxygenation after hypoxia: a dose response study in newborn pigs. Shock 28:317–325
Wessel DL (2001) Managing low cardiac output syndrome after congenital heart surgery. Crit Care Med 29:S220–S230
Monrad ES, McKay RG, Baim DS, Colucci WS, Fifer MA, Heller GV, Royal HD, Grossman W (1984) Improvement in index of diastolic performance in patients with congestive heart failure treated with milrinone. Circulation 70:1030–1037
Coe JY, Olley PM, Vella G, Coceani F (1987) Bipyridine derivatives lower arteriolar resistance and improve left ventricular function in newborn lambs. Pediatr Res 22:422–428
Chang AC, Atz AM, Wernovsky G, Burke RP, Wessel DL (1995) Milrinone: systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med 23:1907–1904
Monrad ES, Baim DS, Smith HS, Lanoue A, Brauwald E, Grossman W (1985) Effects of milrinone on coronary hemodynamics and myocardial energetics in patients with congestive heart failure. Circulation 71:972–979
Paradisis M, Evans N, Kluckow M, Osborn D, McLachlan AJ (2006) Pilot study of milrinone for low systemic blood flow in very preterm infants. J Pediatr 148:306–313
Bassler D, Choong K, McNamara P, Kirpalani H (2006) Neonatal persistent pulmonary hypertension treated with milrinone: four case reports. Biol Neonate 89:1–5
Danhaive O, Margossian R, Geva T, Kourembanas S (2005) Pulmonary hypertension and right ventricular dysfunction in growth restricted, extremely low birth weight neonates. J Perinatol 25:495–499
McNamara PJ, Laique F, Muang-In S, Whyte HE (2006) Milrinone improves oxygenation in neonates with severe persistent pulmonary hypertension of the newborn. J Crit Care 21:217–222
Parr GV, Blackstone EH, Kirklin JW (1975) Cardiac performance and mortality early after intracardiac surgery in infants and young children. Circulation 51:867–874
Haase E, Bigam DL, Nakonechny QB, Jewell LD, Korbutt G, Cheung PY (2004) Resuscitation with 100% oxygen causes intestinal glutathione oxidation and reoxygenation injury in asphyxiated newborn piglets. Ann Surg 240:364–373
Passonneau JV, Lowry OH (1993) Enzymatic analysis: a practical guide. Humana, Press Totowa
Brocks DR, Spencer TJ, Shayeganpour A (2005) A sensitive and specific high performance liquid chromatographic assay for milrinone in rat and human plasma using a commercially available internal standard and low sample volume. J Pharm Sci 8:124–131
Rose AG, Opie LH, Bricknell OL (1976) Early experimental myocardial infarction: evaluation of histologic criteria and comparison with biochemical and electrocardiographic measurements. Arch Pathol Lab Med 100:574–580
Duggal B, Pratap U, Slavik Z, Kaplanova J, Macrae D (2005) Milrinone and low cardiac output following cardiac surgery in infants: is there a direct myocardial effect. Pediatr Cardiol 26:642–645
Hoffman TM, Wernovsky G, Atz AM, Bailey JM, Akbary A, Kocsis JF, Nelson DP, Chang AC, Kulik TJ, Spray TL, Wessel DL (2002) Prophylactic intravenous use of milrinone after cardiac operation in pediatrics (PRIMACORP) study. Am Heart J 143:15–21
Haase E, Bigam DL, Nakonechny QB, Rayner D, Korbutt G, Cheung PY (2005) Cardiac function, myocardial glutathione, and matrix metalloproteinase-2 levels in hypoxic newborn pigs reoxygenated by 21%, 50%, or 100% oxygen. Shock 23:383–389
Hoffman TM, Wernovsky G, Atz AM, Kulik TJ, Nelson DP, Chang AC, Bailey JM, Akbary A, Kocsis JF, Kaczmarek R, Spray TL, Wessel DL (2003) Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation 107:996–1002
Dakshinamurti S (2005) Pathophysiologic mechanisms of persistent pulmonary hypertension of the newborn. Pediatr Pulmonol 39:492–503
Cheung PY, Barrington KJ, Bigam DL (1998) Temporal effects of prolonged hypoxemia and reoxygenation on systemic, pulmonary and mesenteric perfusions in newborn piglets. Cardiovasc Res 39:451–458
Phillipos EZ, Robertson MA (1995) A randomized double blinded controlled trial of dopamine versus epinephrine on pulmonary arterial pressure in premature infants < 1750 grams. Pediatr Res 47:425 (Abstract)
Cheung PY. Barrington KJ (2001) The effects of dopamine and epinephrine on hemodynamics and oxygen metabolism in hypoxic anesthetized piglets. Crit Care 5:158–168
Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, Volpe JJ (2000) Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106:625–632
Pourcyrous M, Parfenova H, Bada HS, Korones SB, Leffler CW (1997) Changes in cerebral cyclic nucleotides and cerebral blood flow during prolonged asphyxia and recovery in newborn pigs. Pediatr Res 41:617–623
Pryds O, Greisen G, Lou H, Friis-Hansen B (1990) Vasoparalysis is associated with brain damage in asphyxiated term infants. J Pediatr 117:119–125
Setoyama K, Ota H, Miura N, Fujiki M, Misumi K, Sakamoto H (2002) Effects of milrinone on hemodynamics and regional blood flow in the hypoxic dog. J Vet Med Sci 64:499–503
Gratton R, Carmichael L, Homan J, Richardson B (1996) Carotid arterial blood flow in the ovine fetus as a continuous measure of cerebral blood flow. J Soc Gynecol Invest 3:60–65
Bennet L, Booth L, Malpas SC, Quaedackers JS, Jensen E, Dean J, Gunn AJ (2006) Acute systemic complications in the preterm fetus after asphyxia: role of cardiovascular and blood flow responses. Clin Exp Pharmacol Physiol 33:291–299
Weindling AM, Kissack CM (2001) Blood pressure and tissue oxygenation in the newborn baby at risk of brain damage. Biol Neonate 79:241–245
Swindle M (1985) Porcine models in surgical research: an overview. In: Tumbleson M (ed) Swine in biomedical research, vol 1. Plenum, New York, pp 235–242
Gootman PM (1985) Cardiovascular regulation in developing swine. In: Tumbleson M (ed) Swine in biomedical research, vol 2. Plenum, New York, pp 1161–1175
Markus T, Hansson S, Am-Wåhlin I, Hellström-Westas L, Saugstad OD, Ley D (2007) Cerebral inflammatory response after fetal asphyxia and hyperoxic resuscitation in newborn sheep. Pediatr Res 62:71–77
Acknowledgements
We sincerely thank the excellent technical assistance of Corinne Tymafichuk and Judy Li of the Neonatal Sciences Laboratory, and Lynette Elder of Dr. Korbutt's Laboratory in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The project was funded by operating grants from the Canadian Institutes of Health Research and Stollery Children's Hospital Foundation. C.J. received support from the Clinician Investigator Program of the Royal College of Physicians and Surgeons of Canada and Clinical Fellowship Program of the Alberta Heritage Foundation for Medical Research; P.Y.C. is an investigator of the Canadian Institutes of Health Research and the Alberta Heritage Foundation for Medical Research.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Joynt, C., Bigam, D.L., Charrois, G. et al. Dose-response effects of milrinone on hemodynamics of newborn pigs with hypoxia-reoxygenation. Intensive Care Med 34, 1321–1329 (2008). https://doi.org/10.1007/s00134-008-1060-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1060-5