Abstract
Objective
To assess the relationship between the base deficit value in the immediate postoperative period of coronary surgery for cardiopulmonary bypass and the length of stay in the ICU.
Design and setting
Prospective descriptive study in the department of anesthesia and cardiovascular surgery of a university hospital.
Patients
185 consecutive patients.
Interventions
Coronary artery bypass graft with cardiopulmonary by pass.
Measurements and results
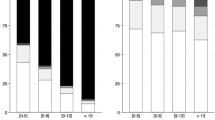
Thirty variables were determined during the pre-, intra-, and postoperative periods; a statistical univariate analysis was performed differentiating patients whose length of stay in the ICU was 2 days or less and those whose stay was more than 2 days. Secondly, a logistic regression model was performed on the variables shown to have a statistically significant difference in univariate analysis, with determination of the odd ratio. Fourteen variables had a statistically significant difference in univariate analysis and three of them highlighted by the logistic regression model: administration of catecholamines, base deficit value in the 1st h postoperatively, and age with odd ratios, respectively, of 3.15, 1.51, and 1.07).
Conclusions
The value of base deficit measured during the 1st h after coronary surgery for cardiopulmonary bypass is correlated with the length of stay in ICU.
Similar content being viewed by others
References
Tu JV, Mazer CD, Levinton C, Armstrong PW, Naylor CD (1994) A predictive index for length of stay in the intensive care unit following cardiac surgery. Can Med Assoc J 151:117–185
Tu JV, Jaglal SB, Naylor CD (1995) Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Circulation 91:677–684
Tuman K, McCarthy R, March R, Najafi H, Ivankovich A (1992) Morbidity and duration of ICU stay after cardiac surgery. A model for preoperative risk assessment. Chest 102:36–44
Davis JW, Shackford SR, Mackersie RC, Hoyt DB (1988) Base deficit as a guide to volume resuscitation. J Trauma 28:1464
Siegel JH, Rivkind AI, Dala S, Goodarzi S (1990) Early physiologic predictors of injury severity and death in blunt multiple trauma. Arch Surg 125:498
Davis JW, Parks SN, Kaups KL, Gladen HE, O'Donnell-Nicol S (1996) Admission base deficit predicts transfusion requirements and risk of complication. J Trauma 41:769
Davis JW, Shackford SR, Holbrook TL (1991) Base deficit as a sensitive indicator of compensated shock and tissue oxygen utilization. Surg Gynecol Obst 173:473
Davis JW (1994) The relationship of base deficit to lactate in porcine hemorrhagic shock and resuscitation. J Trauma 36:168
Dunham CM, Siegel JH, Weireter L (1991) Oxygen debt and metabolic acidemia as quantitative predictors of mortality and the severity of the ischemic insult in hemorrhagic shock. Crit Care Med 19:231–243
Rutherford EJ, Morris JA Jr, Reed GW, Hall K (1992) Base deficit stratifies mortality and determines therapy. J Trauma 33:417
Sauai A, Moore FA, Moore EE, Haenel JB, Read RA, Lezotte DC (1994) Early predictors of post-injury multiple organ failure. Arch Surg 129:39
Boyd O, Mackay CJ, Lamb G, Bland JM, Grounds RM, Bennett ED (1993) Comparison of clinical information gained from routine blood gas analysis and from gastric tonometry for intramural pH. Lancet 341:142
Botha AJ, Moore FA, Moore EE, Peterson VM, Goode AW (1997) Base deficit after major trauma directly relates to neutrophil CD11b expression: a proposed mechanism of shock-induced organ injury. Intensive Care Med 23:504
Jonathan H. Waters, Lawrence R. Miller, Sara Clack, Joyce V Kim (1999) Cause of metabolic acidosis in prolonged surgery. Crit Care Med 27:2142–2146
Jonathan H. Waters, Clifford A. Bernstein (2000) Dilutional acidosis following hetastarch or albumin in healthy volunteers. Anesthesiology 93:1184–1187
Rehm M, Orth V, Scheingraber S, Kreimeier U, Brechtelsbauer H, Finsterer U (2000) Acid-base changes caused by 5% albumin versus 6% hydroxyethyl starch solution in patients undergoing acute normovolemic hemodilution. Anesthesiology 93:1174–1183
Liskaser FJ, Bellomo R, Hayhoe M, Story D, Poustie S, Smith B, Letis A, Bennett M (2000) Role of pump prime in the etiology and pathogenesis of cardiopulmonary bypass-associated acidosis. Anesthesiology 93:1170–1173
Michalopoulos A, Tzelepis G, Pavlides G (1996) Determinants of duration of ICU stay after coronary artery bypass graft surgery. Br J Anaesth 77:208–212
Poeze M, Graham R, Greve JWM, Singer M (1999) Prediction of postoperative cardiac surgical morbidity and organ failure within 4 hours of intensive care unit admission using esophageal Doppler ultrasonography. Crit Care Med 27:1288–1294
Rady MY, Ryan T (1999) Perioperative predictors of extubation failure and the effect on clinical outcome after cardiac surgery. Crit Care Med 27:340–347
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hugot, P., Sicsic, JC., Schaffuser, A. et al. Base deficit in immediate postoperative period of coronary surgery with cardiopulmonary bypass and length of stay in intensive care unit. Intensive Care Med 29, 257–261 (2003). https://doi.org/10.1007/s00134-002-1587-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-002-1587-9