Abstract
Aims
The higher prevalence of chronic physical health conditions among people with psychotic disorders may result in a reduced life expectancy as compared to the general population. More research is needed on the risk of multiple co-occurring chronic health conditions, known as multimorbidity, for people with psychotic disorders.
Methods
We conducted a matched retrospective cohort study to quantify the prevalence of multimorbidity and associated factors among people with psychotic disorders over the 10-year period following first diagnosis, relative to those without psychosis. Data from an early psychosis intervention program in London, Canada were linked to population-based health administrative data to identify patients with first-episode psychosis (n = 439), and a comparison group from the general population (n = 1759) matched on age, sex, and postal code. We followed the cohort for 10 years to ascertain the prevalence of multimorbidity. We compared people with and without psychosis using modified Poisson regression models, and explored risk factors for multimorbidity among those with psychotic disorders.
Results
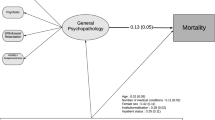
People with psychotic disorders may have a 26% higher prevalence of multimorbidity 10 years following first diagnosis, although our findings include the possibility of a null effect (PR = 1.26, 95% CI 0.96–1.66). People with psychosis living in areas with the highest levels of material deprivation had a threefold higher prevalence of multimorbidity as compared to those in the lowest areas of material deprivation (PR = 3.09, 95% CI 1.21–7.90).
Conclusion
Multimorbidity is prevalent among those with psychosis, and assessment for chronic health conditions should be integrated into clinical care for younger populations with psychotic illness.
Similar content being viewed by others
References
Foley DL (2018) Multiple indicators of ill health are evident in people with psychosis. Evid Based Ment Heal 21:e1 LP-e2. https://doi.org/10.1192/bjp.bp.112.123943
Lee EE, Liu J, Tu X et al (2018) A widening longevity gap between people with schizophrenia and general population: a literature review and call for action. Schizophr Res 196:9–13
De Hert M, Correll CU, Bobes J et al (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10:52–77
Meyer JM, Davis VG, Goff DC et al (2008) Change in metabolic syndrome parameters with antipsychotic treatment in the CATIE Schizophrenia Trial: prospective data from phase 1. Schizophr Res 101:273–286
Smith M, Hopkins D, Peveler RC et al (2008) First-v. second-generation antipsychotics and risk for diabetes in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 192:406–411
Kalman D, Morissette SB, George TP (2005) Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict 14:106–123
Stubbs B, Williams J, Gaughran F, Craig T (2016) How sedentary are people with psychosis? A systematic review and meta-analysis. Schizophr Res 171:103–109
Foley DL, Morley KI (2011) Systematic review of early cardiometabolic outcomes of the first treated episode of psychosis. Arch Gen Psychiatry 68:609–616
Mitchell AJ, Vancampfort D, De Herdt A et al (2013) Is the prevalence of metabolic syndrome and metabolic abnormalities increased in early schizophrenia? A comparative meta-analysis of first episode, untreated and treated patients. Schizophr Bull 39:295–305. https://doi.org/10.1093/schbul/sbs082
Filipcic IS, Ivezic E, Jaksic N et al (2019) Gender differences in early onset of chronic physical multimorbidities in schizophrenia spectrum disorder: Do women suffer more? Early Interv Psychiatry. https://doi.org/10.1111/eip.12867
Smith DJ, Langan J, McLean G et al (2013) Schizophrenia is associated with excess multiple physical-health comorbidities but low levels of recorded cardiovascular disease in primary care: cross-sectional study. BMJ Open 3:e002808
Salisbury C, Johnson L, Purdy S, Valderas JM (2011) Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract 61:e12–e21. https://doi.org/10.3399/bjgp11X548929
Agborsangaya CB, Lau D, Lahtinen M et al (2012) Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health 12:201
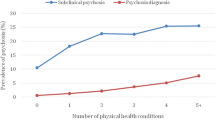
Moreno C, Nuevo R, Chatterji S et al (2013) Psychotic symptoms are associated with physical health problems independently of a mental disorder diagnosis: results from the WHO World Health Survey. World Psychiatry 12:251–257. https://doi.org/10.1002/wps.20070
Strassnig M, Harvey P, Holden J, et al (2019) O6.6. Real world sedentary behavior and activity levels in schizophrenia patients and healthy controls derived from ecological momentary assessment. In: Schizophrenia Bulletin, 2019/04/09. Oxford University Press, pp S178–S178
Owen N, Sparling PB, Healy GN et al (2010) Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc 85:1138–1141. https://doi.org/10.4065/mcp.2010.0444
Multimorbidity Technical Working Group (2012) Summary Report: Technical Meeting: Measurement of Multimorbidity for Chronic Disease Surveillance in Canada
Lehnert T, Heider D, Leicht H et al (2011) Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387–420
Sinnott C, Mc Hugh S, Browne J, Bradley C (2013) GPs’ perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open 3:e003610
Makovski TT, Schmitz S, Zeegers MP et al (2019) Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. https://doi.org/10.1016/j.arr.2019.04.005
Rodrigues M, Wiener JC, Stranges S, et al (2020) The risk of physical multimorbidity in people with psychotic disorders: A systematic review and meta-analysis. J Psychosom Res 110315
Fortin M, Almirall J, Nicholson K (2017) Development of a research tool to document self-reported chronic conditions in primary care. JOC. https://doi.org/10.15256/joc.2017.7.122.285
Ryan BL, Jenkyn KB, Shariff SZ et al (2018) Beyond the grey tsunami: a cross-sectional population-based study of multimorbidity in Ontario. Can J Public Heal 109:845–854
Benchimol EI, Smeeth L, Guttmann A et al (2015) The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 12:e1001885. https://doi.org/10.1371/journal.pmed.1001885
ICES (2020) About ICES. https://www.ices.on.ca/About-ICES. Accessed 14 Apr 2020
Norman RMG, Manchanda R (2016) Prevention and early intervention program for psychoses (PEPP). Heal Q 18:37–41
ElTayebani M, ElGamal M, Roshdy R, Al-Khadary S (2014) Gender difference in affective and nonaffective psychosis. Egypt J Psychiatry 35:45
Chen Y, Farooq S, Edwards J et al (2019) Patterns of symptoms before a diagnosis of first episode psychosis: a latent class analysis of UK primary care electronic health records. BMC Med 17:227. https://doi.org/10.1186/s12916-019-1462-y
George M, Maheshwari S, Chandran S et al (2017) Understanding the schizophrenia prodrome. Indian J Psychiatry 59:505–509. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_464_17
Feely A, Lix LM, Reimer K (2017) Estimating multimorbidity prevalence with the Canadian chronic disease surveillance system. Heal Promot Chronic Dis Prev Canada Res policy Pract 37:215
Roberts KC, Rao DP, Bennett TL et al (2015) Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Heal Promot Chronic Dis Prev Canada Res policy Pract 35:87–94
Matheson FI, van Ingen T (2018) 2016 Ontario marginalization index: user guide. St. Michael’s Hospital. Joint publication with Public Health Ontario, Toronto
Moin JS, Moineddin R, Upshur REG (2018) Measuring the association between marginalization and multimorbidity in Ontario, Canada: A cross-sectional study. J Comorbidity 8:2235042X18814939. https://doi.org/10.1177/2235042X18814939
Köhler O, Horsdal HT, Baandrup L et al (2016) Association between Global Assessment of Functioning scores and indicators of functioning, severity, and prognosis in first-time schizophrenia. Clin Epidemiol 8:323–332. https://doi.org/10.2147/CLEP.S109036
Ministry of Community and Social Services (2016) Monthly reports: OW and ODSP
Rosenheck RA, Estroff SE, Sint K et al (2017) Incomes and outcomes: social security disability benefits in first-episode psychosis. Am J Psychiatry 174:886–894. https://doi.org/10.1176/appi.ajp.2017.16111273
Stata (2021) Stata version 17.0 [computer program]. Coll. Station. Tex Stata Corp
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706. https://doi.org/10.1093/aje/kwh090
Hardt J, Herke M, Leonhart R (2012) Auxiliary variables in multiple imputation in regression with missing X: a warning against including too many in small sample research. BMC Med Res Methodol 12:184. https://doi.org/10.1186/1471-2288-12-184
Fortin M, Bravo G, Hudon C et al (2005) Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med 3:223–228. https://doi.org/10.1370/afm.272
Stubbs B, De Hert M, Sepehry AA et al (2014) A meta-analysis of prevalence estimates and moderators of low bone mass in people with schizophrenia. Acta Psychiatr Scand 130:470–486. https://doi.org/10.1111/acps.12313
Carney CP, Jones L, Woolson RF (2006) Medical comorbidity in women and men with schizophrenia. J Gen Intern Med 21:1133–1137
Varghese D, Scott J, Welham J et al (2011) Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr Bull 37:389–393. https://doi.org/10.1093/schbul/sbp083
Gontijo Guerra S, Berbiche D, Vasiliadis H-M (2019) Measuring multimorbidity in older adults: comparing different data sources. BMC Geriatr 19:166. https://doi.org/10.1186/s12877-019-1173-4
Viron MJ, Stern TA (2010) The impact of serious mental illness on health and healthcare. Psychosomatics 51:458–465. https://doi.org/10.1016/S0033-3182(10)70737-4
Stubbs B, Ku P-W, Chung M-S, Chen L-J (2017) Relationship between objectively measured sedentary behavior and cognitive performance in patients with schizophrenia vs controls. Schizophr Bull 43:566–574. https://doi.org/10.1093/schbul/sbw126
Fortin M, Stewart M, Poitras M-E et al (2012) A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 10:142–151
Quiñones AR, Botoseneanu A, Markwardt S et al (2019) Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS ONE 14:e0218462
Penttilä M, Jääskeläinen E, Hirvonen N et al (2014) Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 205:88–94. https://doi.org/10.1192/bjp.bp.113.127753
Tonelli M, Wiebe N, Fortin M et al (2015) Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 15:31. https://doi.org/10.1186/s12911-015-0155-5
Huntley AL, Johnson R, Purdy S et al (2012) Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med 10:134–141. https://doi.org/10.1370/afm.1363
Lambert L, Blais C, Hamel D et al (2012) Evaluation of care and surveillance of cardiovascular disease: can we trust medico-administrative hospital data? Can J Cardiol 28:162–168. https://doi.org/10.1016/j.cjca.2011.10.005
Perry MJ (1996) The relationship between social class and mental disorder. J Prim Prev 17:17–30
Anderson KK, Norman R, MacDougall AG et al (2018) Disparities in access to early psychosis intervention services: comparison of service users and nonusers in health administrative data. Can J Psychiatry 63:395–403
Langan J, Mercer SW, Smith DJ (2013) Multimorbidity and mental health: can psychiatry rise to the challenge? Br J Psychiatry 202:391–393. https://doi.org/10.1192/bjp.bp.112.123943
Knaak S, Mantler E, Szeto A (2017) Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthcare management forum. SAGE Publications Sage CA, Los Angeles, pp 111–116
Acknowledgements
This work was supported by a grant from the Canadian Institutes for Health Research (#153022), an Early Researcher Award from the Ontario Ministry of Research, Innovation, and Science (KKA), and the Dr. Carol Buck Graduate Scholarship in Epidemiology from the Department of Epidemiology and Biostatistics at Western University (MR).
Funding
Role of the funding source: none.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Declaration of interest: none.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodrigues, M., Stranges, S., Ryan, B.L. et al. The prevalence of physical multimorbidity among people with non-affective psychotic disorders 10 years after first diagnosis: a matched retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol 57, 495–503 (2022). https://doi.org/10.1007/s00127-021-02157-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02157-y