Abstract.
Background:
The initial delay to seek treatment accounts for a significant proportion of the unmet need for treatment of common psychiatric conditions. This study aimed to examine the barriers to initial help-seeking and factors that facilitate help-seeking for anxiety and depression.
Methods:
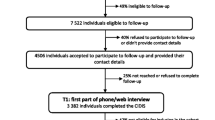
Help-seeking history was retrospectively self-reported by 233 patients at a specialist anxiety clinic, all of whom had delayed seeking professional treatment for at least one month. Data gathered included age at onset, age at help-seeking, primary reason for the delay, prompt to seek help and first professional contacted.
Results:
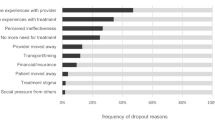
The most frequently endorsed reasons for the delay related to lack of knowledge about mental illness or available treatment. Increasing illness severity or disability was the primary prompt to seek help for the majority of respondents. Reason for the delay showed some relationship with length of the delay, but prompt to seek help did not. A general medical practitioner (GP) was the first professional contacted in 71% of cases.
Conclusions:
Lack of public ‘mental health literacy’ contributes to slow problem recognition. Increasing illness severity eventually facilitates problem recognition and prompts help-seeking. Structural barriers to initial help-seeking are relatively unimportant within the Australian health care system. General practitioners play an important role as gate-keepers to appropriate mental health care.
Similar content being viewed by others
References
Andersen R, Newman JF (1973) Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q 51:95–124
Andrews G,Henderson S (2000) (eds) Unmet need in psychiatry: Problems, resources, responses. Cambridge University Press, Cambridge
Andrews G, Sanderson K, Slade T, Issakidis C (2000) Why does the burden of disease persist? Relating the burden of anxiety and depression to effectiveness of treatment. Bull World Health Organ 78:446–454
Andrews G, Henderson S, Hall W (2001a) Prevalence, comorbidity, disability and service utilization: An overview of the Australian national mental health survey. Br J Psychiatry 178:145–153
Andrews G, Issakidis C, Carter G (2001b) Shortfall in mental health service utilisation. Br J Psychiatry 179:417–425
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders (4th ed). APA, Washington DC
Barkow K, Heun R, Üstün TB, Gänsicke M, Wittchen H-U, Maier W (2002) Test-retest reliability of self-reported age at onset of selected psychiatric diagnoses in general health care. Acta Psychiatr Scand 106:117–125
Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL, Olfson M, Kessler RC (2000) Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: An international survey of members of mental health patient advocate groups. Psych Med 30:693–703
Davenport TA, Hickie IB, Naismith SL, Hazdi-Pavlovic D, Scott EM (2001) Variability and predictors of mental disorder rates and medical practitioner responses across Australian general practices. Med J Aust 175 (suppl):S37–41
Goldberg D, Huxley P (1980) Mental illness in the community: The pathway to psychiatric care. Tavistock, London
Goldberg D, Huxley P (1992) Common mental disorders. Routledge, London
Hickie IB, Davenport TA, Scott EM, Hazdi-Pavlovic D, Naismith SL, Koschera A (2002) Unmet need for recognition of common mental disorders in Australian general practice (comment). Med J Aust 175 [suppl]:S18–24
Hunt C (2000) The unmet need for treatment in panic disorder and social phobia. In: Andrews G, Henderson S (eds) Unmet need in psychiatry: Problems, resources, responses. Cambridge University Press, New York
Huxley P (1996) Mental illness in the community: The Goldberg-Huxley model of the pathway to psychiatric care. Nord J Psychiatry 50 (suppl 37):47–53
Issakidis C, Andrews G (2002) Service utilization for anxiety in an Australian community sample. Soc Psychiatry Psychiatr Epidemiol 37:153–163
Jenkins R, Lewis G, Bebbington PE, Brugha T, Farrell M, Gill B, Meltzer H (1997) The National Psychiatric Morbidity Surveys of Great Britain—initial findings from the household survey. Psych Med 27:765–790
Jenkins R, Strathdee G (2000) The integration of mental health care with primary care. Int J Law Psychiatry 23:277–291
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P (1997) Mental health literacy: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust 166:182–186
Jorm AF, Medway J, Christensen H, Korten AE, Jacomb PA, Rodgers B (2000a) Attitudes towards people with depression: effects on the public’s help-seeking and outcome when experiencing common psychiatric symptoms. Aust N Z J Psychiatry 34:612–618
Jorm AF, Medway J, Christensen H, Korten AE, Jacomb PA, Rodgers B (2000b) Public beliefs about the helpfulness of interventions for depression: effects on actions taken when experiencing anxiety and depression symptoms. Aust N Z J Psychiatry 34:619–626
Kessler D, Lloyd K, Lewis G, Gray DP (1999) Cross sectional study of symptom attribution and recognition of depression and anxiety in primary care. Br Med J 318:136–140
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H, Kendler KS (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the US: Results from the National Comorbidity Survey. Arch Gen Psychiatry 51:8–19
Kessler RC, Olfson M, Berglund PA (1998) Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am J Psychiatry 155:62–69
Leaf PJ, Bruce ML, Tischler GL (1986) The differential effect of attitudes on the use of mental health services. Soc Psychiatry 21:187–192
Leaf PJ, Livingston MM, Tischler GL, Weissman MM, Holzer CE, Myers JK (1985) Contact with health professionals for the treatment of psychiatric and emotional problems. Med Care 23:1322–1337
Meadows G, Burgess P, Bobevski I, Fossey E, Harvey C, Liaw S-T (2002) Perceived need for mental health care: Influences of diagnosis, demography and disability. Psych Med 32:299–309
Mechanic D (1980) Mental health and social policy. Prentice Hall, Englewood Cliffs, New Jersey
Meltzer H, Bebbington P, Brugha T, Farrell M, Jenkins R, Lewis G (2000) The reluctance to seek treatment for neurotic disorders. J Ment Health 9:335–343
Mojtabai R, Olfson M, Mechanic D (2002) Perceived need and help-seeking in adults with mood, anxiety or substance use disorders. Arch Gen Psychiatry 59:77–84
Parslow RA, Jorm AF (2002) Improving Australians’ depression literacy. Med J Aust 177 (suppl.):S117–121
Roper Starch Worldwide Inc. (2001) America’s Mental Health Survey 2001 (Prepared for the National Mental Health Association, May 2001). www.nmha.org/pdfdocs/mental healthreport 2001.pdf (3 January, 2003)
Segee PF, Maquire L, Ross J, Malik ML, Colket J, Davidson JRT (1999) Demographics, treatment seeking, and diagnoses of anxiety support group participants. J Anxiety Disord 13:315–334
Sims A (1993) The scar that is more than skin deep: the stigma of depression. Br J Gen Pract 43:30–31
Thompson A, Issakidis C, Hunt C (submitted) Predictors of the delay to first seek treatment for anxiety and mood disorders in an Australian clinical sample
Wells JE, Robins LN, Bushnell JA, Jarosz D, Oakley-Browne MA (1994) Perceived barriers to care in St. Louis (USA) and Christchurch (NZ): Reasons for not seeking professional help for psychological distress. Soc Psychiatry Psychiatr Epidemiol 29:155–164
World Health Organisation (1990) Composite international diagnostic interview (CIDI), version 1.0. WHO, Geneva
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thompson, A., Hunt, C. & Issakidis, C. Why wait? Reasons for delay and prompts to seek help for mental health problems in an Australian clinical sample. Soc Psychiatry Psychiatr Epidemiol 39, 810–817 (2004). https://doi.org/10.1007/s00127-004-0816-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-004-0816-7