Abstract
Aims/hypothesis
HLA-A*24 carriership hampers achievement of insulin independence in islet allograft recipients. However, less than half of those who fail to achieve insulin independence carry the allele. We investigated whether genetic polymorphism at the recipients’ zinc transporter 8-encoding SLC30A8 gene (rs13266634) could complement their HLA-A*24 status in predicting functional graft outcome.
Methods
We retrospectively analysed data of a hospital-based patient cohort followed for 18 months post transplantation. Forty C-peptide-negative type 1 diabetic individuals who received >2 million beta cells (>4000 islet equivalents) per kg body weight in one or two intraportal implantations under similar immunosuppression were genotyped for SLC30A8. Outcome measurements included achievement and maintenance of graft function. Metabolic benefit was defined as <25% CV of fasting glycaemia in the presence of >331 pmol/l C-peptide, in addition to achievement of insulin independence and maintenance of C-peptide positivity.
Results
In multivariate analysis, HLA-A*24 positivity, presence of SLC30A8 CT or TT genotypes and BMI more than or equal to the group median (23.9 kg/m2) were independently associated with failure to achieve insulin independence (p = 0.015–0.046). The risk increased with the number of factors present (p < 0.001). High BMI interacted with SLC30A8 T allele carriership to independently predict difficulty in achieving graft function with metabolic benefit (p = 0.015). Maintenance of C-peptide positivity was mainly associated with older age at the time of implantation. Only HLA-A*24 carriership independently predicted failure to maintain acceptable graft function once achieved (p = 0.012).
Conclusions/interpretation
HLA-A*24, the SLC30A8 T allele and high BMI are associated with poor graft outcome and should be considered in the interpretation of future transplantation trials.
Trial registration
ClinicalTrials.gov NCT00798785 and NCT00623610
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
In our clinical transplant protocol with cultured islet cell grafts (>2 million beta cells per kg body weight [BW] or >4000 islet equivalents [IEQ] per kg BW), HLA-A*24+ recipients less frequently achieved insulin independence within 6 months post implantation compared with HLA-A*24− individuals [1]. However, HLA-A*24 was only present in less than half of the recipients who failed to achieve insulin independence. We therefore searched for additional baseline characteristics of recipients that could complement their HLA-A*24 status in predicting graft function.
Since zinc transporter 8 (ZnT8) is a major antigenic target for autoreactive antibodies and CD8+ T lymphocytes in type 1 diabetes [2,3,4], we examined a correlation of graft outcome with genetic polymorphism at the SLC30A8 gene, which encodes for this transmembrane protein that facilitates Zn2+ efflux from cells and sequestration into intracellular compartments [5, 6]. This protein is abundantly expressed in secretory granules of pancreatic beta cells [2] but is also present in pancreatic alpha cells and adipose tissue [7, 8]. A non-synonymous SNP in SLC30A8 (rs13266634) encodes for either Arg (C allele) or Trp (T allele) at aa325 in the intracellular carboxy-terminal domain of ZnT8. This polymorphic region appears highly immunogenic, as the nature of aa325 determines the specificity of the autoimmune response in type 1 diabetes [2, 9]. We therefore hypothesised that ZnT8 polymorphism might influence functional graft outcome by modulating auto- and/or alloimmune responses. In addition, rs13266634 alleles and various SLC30A8 mutations have been associated with differences in ZnT8 activity, insulin secretion, insulin sensitivity and clearance, and risk of type 2 diabetes and post-transplantation diabetes mellitus in renal allograft recipients [10,11,12,13,14]. Moreover, interactions between environmental factors and SLC30A8 polymorphisms appear to modulate the risk of obesity in humans and in animal models [15, 16].
In the context of our previous short communication [1], we observed that in HLA-A*24− allograft recipients both failure to achieve insulin independence and development of an autoantibody surge post transplantation were associated with a higher BMI (p = 0.005 and p = 0.019, respectively) (unpublished observations from our previous analysis in reference [1]). Excess BMI has also been proposed as a risk factor for type 1 diabetes development in autoantibody-positive relatives, and as a driver of beta cell loss in individuals with recent-onset type 1 diabetes [17, 18].
Given the importance of ZnT8 as a diabetes autoantigen and the reported interactions of its variants with components of the metabolic syndrome [13,14,15,16], we investigated whether, in recipients of an islet allograft, rs13266634 polymorphism and BMI at baseline impacted graft function and could complement HLA-A*24 for prediction of functional outcome. To test this hypothesis, we determined rs13266634 polymorphism in recipients and donors included in a previous publication [1]. We therefore retrospectively analysed the impact of the two candidate genetic risk factors and BMI on graft function during an 18 month observation period post transplantation. In addition to achievement of insulin independence and maintenance of C-peptide positivity used in our previous report [1], we included achievement and maintenance of acceptable graft function (defined as basal C-peptide >331 pmol/l) associated with the metabolic benefit of a low variability in fasting glucose (defined as <25% CV of fasting glycaemia [CVfg]) as outcome criteria [19].
Methods
Participants
Forty C-peptide-negative type 1 diabetic individuals (median age 45 years) who were beginning to have chronic complications and/or hypoglycaemic unawareness, with no pre-existing HLA class I or II antibodies [20, 21], received 2.3–9.0 million beta cells (~4600–18,000 IEQ) per kg BW in one (n = 10) or two (n = 30) intraportal implantations, with ≤6 months between the first and second grafts (ClinicalTrials.gov NCT00798785 and NCT00623610), under anti-thymocyte globulin–mycophenolate mofetil–tacrolimus immunosuppression [19, 22]. Data and DNA samples collected during the above clinical transplantation trials were made available by the principal investigator (BK) for additional analysis in our previous report [1] (database and analysis of HLA class I alleles including HLA-A*24) and in the present study (database and analysis of SLC30A8 gene polymorphism). Compared with our previous study [1], one participant was excluded because immunosuppression had to be stopped due to the development of a melanoma 12 months post implantation. The study was approved by the Institutional Review Board of the University Hospital of the Vrije Universiteit Brussel; written informed consent was obtained from all participants [19, 22].
Assays and outcome measures
Plasma C-peptide and proinsulin (to correct for proinsulin interference in the C-peptide assay) were measured by time-resolved fluorescence immunoassay on AutoDELFIA (PerkinElmer, Turku, Finland) [23, 24]. HbA1c levels were determined by HPLC (Tosoh Bioscience, Tessenderlo, Belgium), and lymphocyte subclasses by an Epics XL flow cytometer (Beckman Coulter, Miami, FL, USA). C-peptide negativity [1] and acceptable graft function with a metabolic benefit [19] were defined as before. The time of achieving insulin independence was defined as the beginning of a period of at least 14 days without insulin injections. Autoantibodies against GAD, insulinoma-associated antigen-2 and ZnT8 were determined by liquid-phase radiobinding assays [25] at various time points within 6 months after the first islet implantation [1]. Significant autoantibody surges were defined as previously described [1, 26]. HLA-DQ2/DQ8 and HLA-A*24 were determined by allele-specific oligotyping [27], and ZnT8 genotypes by allelic discrimination (7900HT Fast Real-Time PCR System, TaqMan SNP Genotyping Assays, catalogue no. 4351379, and TaqMan Genotyping Master Mix, catalogue no. 4371355; Applied Biosystems, Foster City, CA, USA) [28]. The hyperglycaemic clamp procedure was performed as before [22]. C-peptide measurements at 120, 135 and 150 min of hyperglycaemia (10 mmol/l) were used to calculate C-peptide AUC [1]. Not all participants underwent the hyperglycaemic clamp test at 6, 12 and/or 18 months after the first implantation, because the procedure was implemented in the protocol when the follow-up of certain participants had already begun or was completed.
Statistical analysis
The data were analysed with the Mann–Whitney U test, χ2 test or Fisher’s exact test. Kaplan–Meier analysis with the logrank test was used to assess achievement of insulin independence, achievement and maintenance of acceptable graft function and maintenance of C-peptide positivity. The tested factors were compared with previously reported determinants for their capacity to act as independent predictors of insulin independence, achievement and maintenance of acceptable graft function and maintenance of C-peptide positivity, by means of time-dependent Cox regression analysis performed by a forward stepwise method. Only variables with p values <0.1 in the univariate analysis were entered into multivariate models with respect to the maximum number of variables allowed according to the Vittinghoff criterion [29]. All tests were performed two-sided using IBM SPSS for Windows, version 24.0 (IBM, Armonk, NY, USA). A p value <0.05 was considered significant.
Results
Occurrence of investigated risk factors among recipients
Subgroups were defined on the basis of the occurrence of three selected risk factors: HLA-A*24 status, SLC30A8 polymorphism and BMI. Twelve recipients carried HLA-A*24. The CC, CT and TT SLC30A8 genotypes at rs13266634 were present in 19, 17 and four participants, respectively. Since carriers of the CT and TT genotypes did not differ in frequency of developing insulin independence (electronic supplementary material [ESM] Fig. 1), we used a dominant model with respect to the T allele (CC vs CT+TT). To investigate the impact of BMI at baseline, the study population was stratified according to the median (P50; 23.9 kg/m2) of the whole group (BMI <P50 vs BMI ≥P50).
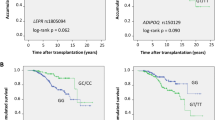
Association of selected risk factors with probability of achieving graft function
At post-transplantation month 2, HbA1c levels were <47 mmol/mol (6.5%) in all recipients. Eighteen achieved insulin independence which lasted for a median period (range) of 16.5 (3.5–44.2) months. Within 12 months after the first implantation, 34 participants achieved CVfg <25% in the presence of random C-peptide >331 pmol/l, and in 18 participants this was sustained for ≥18 months after achieving the functional endpoint. Low HbA1c levels (<47 mmol/mol [6.5%]) persisted less long, as all but four individuals presented with HbA1c values ≥47 mmol/mol (6.5%) 18 months after the first implantation (not shown). HLA-A*24− individuals (n = 28) displayed a higher rate of achieving insulin independence compared with HLA-A*24+ individuals (n = 12; p = 0.036) (Fig. 1a), but metabolic outcome in terms of reduction in CVfg (to <25%) and of random C-peptide >331 pmol/l was similar for both subgroups (Fig. 1b). Progression rate to insulin independence was also higher in carriers of the SLC30A8 CC genotype (n = 19) than in CT- or TT-positive recipients (n = 21) (p = 0.022) (Fig. 1c), while again no significant difference was observed in the rate of achieving the two additional endpoints (Fig. 1d). The higher rate of reaching insulin independence in the presence of CC than in the presence of CT or TT could not be explained by differences in the degree of mismatching with the donors’ SLC30A8 genotype; indeed, the frequency of mismatches was higher for CC-positive recipients (0–83%) than for CT-positive recipients (0%), but lower than for TT carriers (67–100%). However, CT and TT carriers had similar functional outcomes, which were worse for both groups than for CC carriers (ESM Fig. 1 and ESM Table 1). The rate of reaching insulin independence was higher in participants with BMI <P50 (n = 20) than in those with BMI ≥P50 (n = 20); this was also the case for reaching the additional functional endpoints (p = 0.044 and p = 0.016, respectively) (Fig. 1e, f).
Development of insulin independence (a,c,e) and achievement of CVfg <25% and C-peptide >331 pmol/l (b,d,f) in islet allograft recipients. (a, b) HLA-A*24− (solid line) vs HLA-A*24+ participants (dashed line) (number of events and total number of participants per group: a, 16/28 vs 2/12; b, 24/28 vs 10/12) (c, d) SCL30A8 CC (solid line) vs CT and TT (dashed line) (number of events and total number of participants per group: c, 12/19 vs 6/21; d, 18/19 vs 16/21). (e, f) BMI <P50 (solid line) vs BMI ≥P50 (dashed line) (number of events and total number of participants per group: e, 12/20 vs 6/20; f, 19/20 vs 15/20). None of the 18 participants who became insulin-independent returned to C-peptide negativity within 18 months after the first transplantation. CVfg remained <25% in 15 of those 18 participants during 18 months of follow-up (not shown). Compared with our previous study [1], one participant was excluded because immunosuppression had to be stopped owing to the development of a melanoma 12 months post implantation. *p < 0.05
Association of selected risk factors with probability of maintaining graft function
HLA-A*24− recipients tended to maintain C-peptide positivity longer during follow-up (p = 0.05) (Fig. 2a). Among recipients who achieved graft function with a metabolic benefit (CVfg <25% and random C-peptide >331 pmol/l), those who lacked HLA-A*24 tended to maintain this good functional outcome longer compared with carriers of this allele (p = 0.007) (Fig. 2b). Maintenance of C-peptide positivity or graft function was not affected by SLC30A8 genotype or BMI (Fig. 2c–f). Carriers of HLA-A*24 needed more insulin (p = 0.035–0.003 depending on the time point) (Table 1), and presented higher HbA1c values and glycaemic variability compared with HLA-A*24− recipients during follow-up (Table 1). Also, their hyperglycaemic clamp-derived C-peptide AUC tended to decline more rapidly during follow-up (Table 1). None of these metabolic variables were significantly affected by the recipients’ SLC30A8 genotype or BMI (data not shown).
C-peptide-positive survival in all allograft recipients (a,c,e) and maintenance of CVfg <25% and C-peptide >331 pmol/l in recipients who achieved acceptable graft function (b,d,f). (a, b) HLA-A*24− (solid line) vs HLA-A*24+ participants (dashed line) (number of events and total number of participants per group: a, 24/28 vs 7/12; b, 16/24 vs 2/10). (c, d) SCL30A8 CC (solid line) vs CT + TT (dashed line) (number of events and total number of participants per group: c, 16/19 vs 15/21; d, 10/18 vs 8/16). (e, f) BMI <P50 (solid line) vs BMI ≥P50 (dashed line) (number of events and total number of participants per group: e, 16/20 vs 15/20; f, 12/19 vs 6/15). None of the 18 participants who became insulin-independent, returned to C-peptide negativity within 18 months after the first transplantation. CVfg remained <25% in 15 of those 18 participants during 18 months after reaching a clinically satisfactory graft function (not shown). Compared with our previous study [1], one participant was excluded because immunosuppression had to be stopped owing to the development of a melanoma 12 months post implantation. **p < 0.01
Complementary contribution of selected risk factors to failure of islet cell implants
In the joint absence of the three risk factors (HLA-A*24, SLC30A8 T allele and BMI ≥P50), six out of seven recipients achieved insulin independence; all seven recipients achieved the set criteria for metabolic graft function and six out of seven maintained it (Table 2). Interestingly, none exhibited a rise in autoantibodies following implantation, whereas such a rise occurred in ten out of 33 recipients when one of these risk factors was present (Table 2).
Interference with favourable outcome by one of the three examined risk factors was higher when at least one additional factor was present (Table 2). The complementarity of the selected risk factors in hampering the achievement or maintenance of the selected outcome measures was also evident when Kaplan–Meier analysis was performed according to the number of factors present (ESM Fig. 2 and ESM Fig. 3, respectively). In particular, we noticed that high BMI and presence of the SLC30A8 T allele interacted to increase the risk of failure to achieve insulin independence (p = 0.005) and satisfactory graft function (p = 0.022) in Kaplan–Meier analysis (ESM Fig. 4). Post-transplantation autoantibody surges tended to occur predominantly in recipients presenting with two or more risk factors (7/19 vs 3/21 in all other recipients; p = 0.100) (not shown).
Assessment of predictive power of tested risk factors vs that of previously reported determinants
All graft and recipient characteristics listed in ESM Tables 2–5 were first tested in univariate Cox regression analysis (data not shown). Only the variables that were significant in univariate analysis and a selection of previously reported potentially confounding risk factors at baseline are shown in Tables 3 and 4. BMI ≥P50, HLA-A*24 positivity and presence of SLC30A8 CT or TT genotypes were all independently associated with failure to achieve insulin independence (Table 3). In multivariate analysis, the risk increased with the number of risk factors (HR 0.31 [95% CI 0.16, 0.74] for zero to three risk factors; p < 0.001) (Table 3). Higher BMI was the only independent predictor of difficulty in achieving acceptable graft function (HR 0.46 [95% CI 0.23, 0.93]; p = 0.029) (Table 3); in multivariate analysis it was outperformed by the joint presence of higher BMI and SLC30A8 T allele (HR 0.32 [95% CI 0.13, 0.80]; p = 0.015) (not shown). In the univariate analysis, maintenance of C-peptide positivity was mainly associated with older age at the time of implantation, in line with the 9th Annual Collaborative Islet Transplant Registry report [30]; multivariate analysis was not performed for this endpoint due to the low number of events (n = 9) (not shown). HLA-A*24 carriership was the only independent predictor of failure to maintain satisfactory graft function (HR 0.28 [95% CI 0.10, 0.75]; p = 0.012) (Table 4). Graft and recipient characteristics listed in Tables 3 and 4 did not differ according to the presence or absence of HLA-A*24 (ESM Table 2), SLC30A8 T allele (ESM Table 3), BMI ≥P50 (ESM Table 4) or at least one risk factor (ESM Table 5).
Discussion
We previously reported that the presence of HLA-A*24 was associated with a higher risk of failure to achieve insulin independence after implantation of a beta cell graft. In the present study, we identified two additional risk factors, i.e. presence of the T allele at rs13266634 of the SLC30A8 gene and high BMI. The three baseline characteristics carry an independent risk which is increased with the number of factors present. All participants lacking the three complementary risk factors achieved and maintained graft function with a metabolic benefit and none experienced a significant post-implantation surge in autoantibody levels, which is considered an indicator of poor functional outcome [1, 31, 32].
A higher BMI—mostly in combination with positivity for the rs13266634 T allele—conferred a lower probability of achieving acceptable graft function (defined as <25% CVfg and >331 pmol/l C-peptide) within the first months post transplantation. By contrast, failure to maintain this level of function was only significantly associated with HLA-A*24 positivity of the recipient, in parallel with a more rapid decline of hyperglycaemic clamp-derived C-peptide release and metabolic control in this group.
The use of glycaemic variability—a surrogate marker for risk of severe hypoglycaemia and a close and inverse correlate of restored functional beta cell mass [19]—as a functional outcome measure is a strength of the study, as is the homogeneity of the patient cohort. All initially C-peptide-negative participants received a sufficient amount of beta cells to generate plasma C-peptide levels at post-transplantation month 2 under similar immunosuppression [1, 21]. The relatively small cohort size constitutes a weakness of our study which may have caused some variables to remain non-significant in Cox regression analysis (Tables 3 and 4). Our observations could also have benefited from a larger number of participants in the subgroups, in particular carriers of the SLC30A8 TT genotype. Our retrospective analysis did not allow us to evaluate insulin sensitivity by euglycaemic–hyperinsulinaemic clamp, nor by surrogate markers such as waist circumference.
Our observations that HLA-A*24 carriership, presence of the SLC30A8 T allele and high BMI of the recipients impact transplant outcome, alone or in combination, do not deny the importance of other well-established graft and recipient characteristics, related, but not limited, to islet isolation procedure, islet cell quality and numbers, pre-existing auto- and alloimmunity, and instant blood-mediated inflammatory reaction post transplantation [22, 31, 33,34,35,36,37,38,39]. However, we have several reasons to believe that our findings are largely independent of these factors. First, when stratified according to the presence or absence of (a combination of) the three investigated risk factors, participants did not differ according to a large number of graft and recipient characteristics (ESM Tables 2–5). Second, none of the participants had pre-existing HLA class I and II antibodies, and their transplant outcome was already previously shown to be unaffected by pre-existing islet autoantibody status [1, 31, 36, 37]. Third, all participants received at least 2 million beta cells (4000 IEQ) per kg BW, an amount previously shown to consistently induce graft function with a metabolic benefit [22]. Finally, excessive beta cell loss in the first hour post implantation could not have biased our results, because only two participants showed a disproportionate rise in plasma GAD65 1 h after implantation of their first islet cell graft [38].
Our results confirm and extend our previous observations on the accelerated loss of implanted beta cells in HLA-A*24+ recipients, regardless of the number of mismatches for this allele with donor HLA [1], and are consistent with reports of an association of the allele with a more rapid progression to clinical onset in autoantibody-positive individuals at risk of type 1 diabetes, and accelerated decline of residual beta cell mass in those with recent-onset type 1 diabetes [27, 40]. Currently, transplantation centres do not preselect recipients on the basis of HLA composition, which limits the value of this observation. Nevertheless, our results re-emphasise that, in order to compare the efficacy of islet allotransplantation protocols or the prognostic value of novel biomarkers, results should be adjusted for the recipients’ HLA-A*24 status. They also raise the question as to whether the immunosuppressive regimen should be adapted for recipients carrying the allele. Although the exact mechanism by which HLA-A*24 affects transplant outcome remains unknown, one might envisage testing a therapy that better targets autoimmune aggression than anti-thymocyte globulin, for example a T cell-directed immunodepletion strategy using an anti-CD3 monoclonal antibody (e.g. otelixizumab) with or without an anti-B cell therapy (e.g. rituximab) [39, 41].
To the best of our knowledge, our finding that the presence of the SLC30A8 T allele combines with BMI ≥P50 (in our cohort, 23.9 kg/m2) to increase insulin needs in allograft recipients and to hamper the achievement of acceptable graft function is novel. The effect of the recipient’s T allele could not be explained by the degree of mismatching with the donor’s SLC30A8 alleles. Indeed, while CT carriers had a lower frequency of mismatches and TT carriers had a higher frequency of mismatches compared with CC-positive recipients, both CT- and TT-positive individuals had overall a worse functional outcome compared with CC-positive participants. Hence, our findings provide no support for the possibility that ZnT8 polymorphism might have impacted allo- or autoimmune responses, as might have been hypothesised from the immunogenicity of the ZnT8 epitope co-determined by rs13266634 [9]. Rather, they may suggest a role for the recipients’ ZnT8 activity in modulating insulin sensitivity, and imply that cell types other than beta cells are likely to be involved in the process. Expression of ZnT8 has indeed been reported in pancreatic alpha cells and in adipose tissue [7, 8], and altered levels of transporter activity have been linked with functional or metabolic changes in animal models [7, 16]. It is, however, unknown through which mechanisms altered non-beta cell ZnT8 activity may impact insulin sensitivity and interact with the effect of raised BMI in humans.
Our observation of a worse functional outcome in allograft recipients carrying the SLC30A8 T allele is consistent with reports of a less preserved beta cell function, higher insulin needs and lower insulin sensitivity in children and adolescents with type 1 diabetes carrying the TT genotype or the T allele, compared with individuals with the CC genotype [42, 43]. Our results are in apparent contradiction to the reported association of the C allele with increased risk of type 2 diabetes and post-transplantation diabetes in kidney allograft recipients [11, 12]. Based on the available knowledge, it is difficult to find a unifying explanation for the seemingly conflicting available data on the relationship between SLC30A8 variants, ZnT8 activity and risk of diabetes (progression). Indeed, while the type 2 diabetes risk allele (C) was associated with lowered ZnT8 activity and beta cell function [10, 12, 44], rare loss-of-function mutations in SLC30A8 were found to confer protection against type 2 diabetes [13]. It has been suggested that the risk of diabetes varies according to the balance between pancreatic hormone secretion and clearance, as influenced by the complex interplay between changes in ZnT8 activity and circulating Zn2+ concentrations [10, 14].
Although a BMI >28 or >26 kg/m2 (depending on the studies) [33,34,35] is being used as an exclusion criterion in islet allotransplantation, overweight (BMI >25 kg/m2) at baseline failed to predict graft function when considered in isolation, but did so when combined with a family history of type 2 diabetes [45]. Our study shows that even a BMI in the upper-normal range might reduce the probability of achieving insulin independence and an acceptable graft function. As BMI is a continuous variable, further studies on larger cohorts should determine from which threshold onwards the risk starts to increase. In our cohort, the effect of BMI became apparent from 23 kg/m2 onwards (not shown). Consistent with those of Leitão et al [45], our results in addition indicate that the effect of BMI is amplified by the presence of other risk factors. In particular, failure to achieve insulin independence and acceptable graft function with a metabolic benefit was most manifest in the combined presence of high BMI and the SLC30A8 T allele (ESM Fig. 4). When participants were stratified according to the presence or absence of high BMI and T allele we observed no difference in baseline insulin needs. Therefore, the latter could not explain the interaction between both risk factors. This is not to deny that the effect of high BMI (greater than or equal to the median of the whole group) on transplant outcome tended to be more pronounced in those with higher insulin needs at baseline (greater than or equal to the median of the whole group) (not shown), in line with previous observations [35, 46]. Our results suggest that candidate recipients of an islet allograft who have a BMI in the upper-normal range or who are slightly overweight should be asked to lose weight before being put on a waiting list.
In conclusion, we identified three recipient characteristics—HLA-A*24, the SLC30A8 T allele and high BMI—that act as independent risk factors for failing to achieve insulin independence following islet allotransplantation and contribute in various ways to hampering the achievement or maintenance of a graft function with metabolic benefit. These results should be confirmed in independent cohorts, as they may have practical implications for the selection, preparation and treatment of participants in future transplantation trials, the design of study protocols and the interpretation of their results.
Data availability
The datasets generated and/or analysed during the current study are available from the principal investigator of the transplantation trial (BK) upon reasonable request.
Abbreviations
- BW:
-
Body weight
- CVfg:
-
CV of fasting glycaemia
- IEQ:
-
Islet equivalents
- ZnT8:
-
Zinc transporter 8
References
Demeester S, Balke EM, Van der Auwera BJ et al (2016) HLA-A*24 carrier status and autoantibody surges posttransplantation associate with poor functional outcome in recipients of an islet allograft. Diabetes Care 39:1060–1064
Wenzlau JM, Juhl K, Yu L et al (2007) The cation efflux transporter ZnT8 (SLC30A8) is a major autoantigen in human type 1 diabetes. Proc Natl Acad Sci U S A 104:17040–17045
Dang M, Rockell J, Wagner R et al (2011) Human type 1 diabetes is associated with T cell autoimmunity to zinc transporter 8. J Immunol 186:6056–6063
Énée É, Kratzer R, Arnoux JB et al (2012) ZnT8 is a major CD8+ T cell-recognized autoantigen in pediatric type 1 diabetes. Diabetes 61:1779–1784
Chimienti F, Devergnas S, Favier A, Seve M (2004) Identification and cloning of a beta-cell-specific zinc transporter, ZnT-8, localized into insulin secretory granules. Diabetes 53:2330–2337
Palmiter RD, Huang L (2004) Efflux and compartmentalization of zinc by members of the SLC30 family of solute carriers. Pflugers Arch 447:744–751
Solomou A, Meur G, Bellomo E et al (2015) The zinc transporter SLC30A8/ZnT8 is required in a subpopulation of pancreatic alpha-cells for hypoglycemia-induced glucagon secretion. J Biol Chem 290:21432–21442
Smidt K, Pedersen SB, Brock B et al (2007) Zinc-transporter genes in human visceral and subcutaneous adipocytes: lean versus obese. Mol Cell Endocrinol 264:68–73
Wenzlau JM, Liu Y, Yu L et al (2008) A common nonsynonymous single nucleotide polymorphism in the SLC30A8 gene determines ZnT8 autoantibody specificity in type 1 diabetes. Diabetes 57:2693–2697
Rutter GA, Chimienti F (2015) SLC30A8 mutations in type 2 diabetes. Diabetologia 58:31–36
Kang ES, Kim MS, Kim YS et al (2008) A polymorphism in the zinc transporter gene SLC30A8 confers resistance against posttransplantation diabetes mellitus in renal allograft recipients. Diabetes 57:1043–2047
Sladek R, Rocheleau G, Rung J et al (2007) A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445:881–885
Flannick J, Thorleifsson G, Beer NL et al (2014) Loss-of-function mutations in SLC30A8 protect against type 2 diabetes. Nat Genet 46:357–363
Pearson E (2014) Zinc transport and diabetes risk. Nat Genet 46:323–324
Hosseini-Esfahani F, Mirmiran P, Koochakpoor G et al (2017) Some dietary factors can modulate the effect of the zinc transporters 8 polymorphism on the risk of metabolic syndrome. Sci Rep 7:1649
Hardy AB, Wijesekara N, Genkin I et al (2012) Effects of high-fat diet feeding on Znt8-null mice: differences between beta cell and global knockout of Znt8. Am J Physiol Endocrinol Metab 302:E1084–E1096
Ferrara CT, Geyer SM, Liu YF et al (2017) Excess BMI in childhood: a modifiable risk factor for type 1 diabetes development? Diabetes Care 40:698–701
Lauria A, Barker A, Schloot N et al (2015) BMI is an important driver of beta cell loss in type 1 diabetes upon diagnosis in 10- to 18-year-old children. Eur J Endocrinol 172:107–113
Gillard P, Hilbrands R, Van de Velde U et al (2013) Minimal functional beta-cell mass in intraportal implants that reduces glycemic variability in type 1 diabetic recipients. Diabetes Care 36:3483–3488
Campbell PM, Salam A, Ryan EA et al (2007) Pretransplant HLA antibodies are associated with reduced graft survival after clinical islet transplantation. Am J Transplant 7:1242–1248
Brooks AM, Carter V, Liew A et al (2015) De novo donor specific HLA antibodies are associated with rapid loss of graft function following islet transplantation in type 1 diabetes. Am J Transplant 15:3239–3246
Keymeulen B, Gillard P, Mathieu C et al (2006) Correlation between beta cell mass and glycemic control in type 1 diabetic recipients of islet cell graft. Proc Natl Acad Sci U S A 103:17444–17449
De Pauw PE, Vermeulen I, Ubani OC et al (2008) Simultaneous measurement of plasma concentrations of proinsulin and C-peptide and their ratio with a trefoil-type time-resolved fluorescence immunoassay. Clin Chem 54:1990–1998
Van Dalem A, Demeester S, Balti EV et al (2016) Prediction of impending diabetes through automated dual-label measurement of proinsulin:C-peptide ratio. PLoS One 11:E0166702
Demeester S, Keymeulen B, Kaufman L et al (2015) Preexisting insulin autoantibodies predict efficacy of otelixizumab in preserving residual beta cell function in recent-onset type 1 diabetes. Diabetes Care 38:644–651
Decochez K, Tits J, Coolens JL et al (2000) High frequency of persisting or increasing islet-specific autoantibody levels after diagnosis of type 1 diabetes presenting before 40 years of age. The Belgian Diabetes Registry. Diabetes Care 23:838–844
Mbunwe E, Van der Auwera BJ, Vermeulen I et al (2013) HLA-A*24 is an independent predictor of 5-year progression to diabetes in autoantibody-positive first-degree relatives of type 1 diabetic patients. Diabetes 62:1345–1350
Schleinitz D, Distefano JK, Kovacs P (2011) Targeted SNP genotyping using the TaqMan® assay. Methods Mol Biol 700:77–87
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and cox regression. Am J Epidemiol 165:710–718
Collaborative Islet Transplant Registry (2016) 9th Annual Collaborative Islet Transplant Registry report. Available from www.citregistry.org/content/citr-9th-annual-report. Accessed 13 Sept 2017
Piemonti L, Everly MJ, Maffi P et al (2013) Alloantibody and autoantibody monitoring predicts islet transplantation outcome in human type 1 diabetes. Diabetes 62:1656–1664
Braghi S, Bonifacio E, Secchi A et al (2000) Modulation of humoral islet autoimmunity by pancreas allotransplantation influences allograft outcome in patients with type 1 diabetes. Diabetes 49:218–224
Vantyghem MC, Defrance F, Quintin D et al (2014) Treating diabetes with islet transplantation: lessons from the past decade in Lille. Diabetes Metab 40:108–119
Shapiro AM, Ricordi C, Hering BJ et al (2006) International trial of the Edmonton protocol for islet transplantation. N Engl J Med 355:1318–1330
Othonos N, Choudhary P (2017) Who should be considered for islet transplantation alone? Curr Diab Rep 17:23
Huurman V, Hilbrands R, Pinkse C et al (2008) Cellular islet autoimmunity associates with clinical outcome of islet cell transplantation. PLoS One 3:e2435
Hilbrands R, Huurman VA, Gillard P et al (2009) Differences in baseline lymphocyte counts and autoreactivity are associated with differences in outcome of islet cell transplantation in type 1 diabetic patients. Diabetes 58:2267–2276
Ling Z, De Pauw P, Jacobs-Tulleneers D et al (2015) Plasma GAD65, a marker for early β-cell loss after intraportal islet cell transplantation in diabetic patients. J Clin Endocrinol Metab 100:2314–2321
Shapiro AMJ (2011) State of the art of clinical islet transplantation and novel protocols of immunosuppression. Curr Diab Rep 11:345–354
Nakanishi K, Inoko H (2006) Combination of HLA-A*24, -DQA1*03, and -DR9 contributes to acute-onset and early complete beta-cell destruction in type 1 diabetes: longitudinal study of residual beta-cell function. Diabetes 55:1862–1868
Chatenoud L (2008) Chemical immunosuppression in islet transplantation—friend or foe? N Engl J Med 358:1192–1193
Nielsen LB, Vaziri-Sani F, Pörksen S et al (2011) Relationship between ZnT8, the SLC30A8 gene and disease progression in children with newly diagnosed type 1 diabetes. Autoimmunity 44:616–623
Moosavi M, Séguin J, Li Q, Polychronakos C (2012) The effect of type 2 diabetes risk loci on insulin requirements in type 1 diabetes. Horm Res Paediatr 77:305–308
Nicolson TJ, Bellomo EA, Wijesekara N et al (2009) Insulin storage and glucose homeostasis in mice null for the granule zinc transporter ZnT8 and studies of the type 2 diabetes-associated variants. Diabetes 58:2070–2083
Leitão CB, Bernetti K, Tharavanij T et al (2009) Type 2 diabetes mellitus phenotype and graft survival after islet transplantation. Transplantation 88:57–61
Al-Adra DP, Gill RS, Imes S et al (2014) Single-donor transplantation and long-term insulin-independence in select patients with type 1 diabetes mellitus. Transplantation 98:1007–1012
Acknowledgements
The authors thank M. Robyn, B. Swennen, K. Rouffe and N. Pardon (Leuven University Hospitals, Leuven, Belgium); S. Vandenhoeck, S. Thomas and V. Van Damme (Brussels University Hospitals, Brussels, Belgium); and R. Braspenning (Antwerp University Hospital, Antwerp, Belgium) for completing all clamp tests.
Contribution statement
EMB, SD, BK and FKG designed the study and acquired, researched and interpreted the data. EMB and SD performed the statistical analyses. DL, PG, RH, UVdV, BJVdA, ZL, BOR and DGP contributed to the data acquisition, analysis and interpretation. EMB and FKG drafted the manuscript and SD, DL, PG, RH, UVdV, BJVdA, ZL, BOR, DGP and BK revised it critically. All authors approved the final version of the manuscript. FKG and BK are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This study was supported by the JDRF (grant 4/2005/1327) and the Willy Gepts Fund of Brussels University Hospitals. PG is funded by the Clinical Research Foundation of Leuven University Hospitals, Catholic University of Leuven.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 858 kb)
Rights and permissions
About this article
Cite this article
Balke, E.M., Demeester, S., Lee, D. et al. SLC30A8 polymorphism and BMI complement HLA-A*24 as risk factors for poor graft function in islet allograft recipients. Diabetologia 61, 1623–1632 (2018). https://doi.org/10.1007/s00125-018-4609-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4609-z