Abstract
Aims/hypothesis
The hormone glucagon-like peptide 1 (GLP-1) is released in response to a meal from the intestinal L-cells, where it is processed from proglucagon by the proconvertase (PC)1/3. In contrast, in the adult islets proglucagon is processed to glucagon by the PC2 enzyme. The aim of the study was to evaluate if, during the development of diabetes, alpha cells produce GLP-1 that, in turn, might trigger beta cell growth.
Methods
Beta cell mass, GLP-1 and insulin levels were measured in the gerbil Psammomys obesus (P. obesus), a rodent model of nutritionally induced diabetes. Furthermore, the presence of biologically active forms of GLP-1 and PC1/3 in alpha cells was demonstrated by immunofluorescence, and the release of GLP-1 from isolated P. obesus, mouse and human islets was investigated.
Results
During the development of diabetes in P. obesus, a significant increase in GLP-1 was detected in the portal vein (9.8 ± 1.5 vs 4.3 ± 0.7 pmol/l, p < 0.05), and in pancreas extracts (11.4 ± 2.2 vs 5.1 ± 1.3 pmol/g tissue, p < 0.05). Freshly isolated islets from hyperglycaemic animals released more GLP-1 following 24 h culture than islets from control animals (28.2 ± 4.4 pmol/l vs 5.8 ± 2.4, p < 0.01). GLP-1 release was increased from healthy P. obesus islets following culture in high glucose for 6 days (91 ± 9.1 pmol/l vs 28.8 ± 6.6, p < 0.01). High levels of GLP-1 were also found to be released from human islets. PC1/3 colocalised weakly with alpha cells.
Conclusions/interpretation
GLP-1 release from alpha cells is upregulated in P. obesus during the development of diabetes. A similar response is seen in islets exposed to high glucose, which supports the hypothesis that GLP-1 released from alpha cells promotes an increase in beta cell mass and function during metabolic challenge such as diabetes.
Similar content being viewed by others
Introduction
Conventional treatment of type 2 diabetes aims to control blood glucose levels through diet and exercise, drugs that target insulin secretion or resistance or by insulin injections. Despite intensive intervention therapies, the diabetic patient displays a continued decline in beta cell mass (BCM) and function [1]. The incretin hormone glucagon-like peptide (GLP)-1 is currently receiving considerable interest because of its ability not only to reduce blood glucose levels but also to potentially regenerate islet BCM [2]. Several in vitro [3, 4] and rodent in vivo studies [5–7] have demonstrated anti-apoptotic and proliferative effects of GLP-1 on pancreatic beta cells. Clearly, restoration of beta cell function will be of a great therapeutic value in the treatment of diabetes.
GLP-1 is a product of the pro-glucagon gene. The pro-glucagon precursor hormone is produced in intestinal L-cells, pancreatic alpha cells and a subset of neurons. The presence of different processing enzymes allows cell-specific products to be generated from the same precursor. In the L-cells, prohormone convertase (PC)1/3 is responsible for the generation of GLP-1 and GLP-2, whereas the alpha cells produce glucagon as a result of processing by PC 2, leaving the active form of the GLP-1 peptide trapped in a larger fragment, the major proglucagon fragment [8, 9]. After GLP-1 is released from the intestinal L-cells to the circulation, it is very rapidly degraded to an inactive metabolite (GLP-1 [9–37]) by the enzyme dipeptidyl peptidase 4 (DPP-IV) and only a small fraction reaches the pancreatic beta cells that express the GLP-1 receptor [10, 11]
The prevailing view is that in adults, all circulating GLP-1 is produced by the intestinal L-cells, with no contribution from the alpha cells as they are thought not to produce PC1/3, thus excluding GLP-1 production. However, several reports have demonstrated the production of a small amount of fully processed GLP-1 from alpha cells [12–15]. Furthermore, during specific stages of fetal development glucagon-positive cells in the pancreas co-produce PC1/3 and hence potentially also secrete GLP-1, which may be of importance during islet cell differentiation [16, 17]. These findings raise the possibility that GLP-1, produced within the islets under certain circumstances, acts as a paracrine factor facilitating beta cell protection and function as well as regeneration when needed. The alpha cells are in close proximity to the GLP-1 receptors on the beta cells, and alpha cells may, if GLP-1 production is switched on, provide a continuous beneficial supply of GLP-1 to the neighbouring beta cells. In support of this view it has recently been shown that rats with streptozotocin-induced beta cell loss display increased islet GLP-1 production [18, 19]. Recently it was elegantly shown by adenovirus introduction of PC1/3 in islet glucagon cells that GLP-1 can be released and act locally to improve islet function [15].
The gerbil Psammomys obesus is an animal model of nutritionally induced type 2 diabetes [20–22]. When these animals are transferred from their natural low-energy saltbush diet to more energy-dense rodent laboratory chow, the initial response is an increase in BCM to compensate for the increased insulin demand, followed by development of hyperglycaemia. This animal model is characterised by fast depletion of insulin stores as hyperglycaemia becomes manifest [23, 24]. Not all animals become hyperglycaemic as some are resistant to the high-energy diet and stay normoglycaemic (non-responders). In this paper, we used P. obesus to investigate the hypothesis that production of GLP-1 within the islets serves as a natural mechanism employed by the islets to promote beta cell function and increase BCM under situations of sustained metabolic pressure, such as hyperglycaemia. The findings are supported by in vitro studies using isolated P. obesus, human and mouse islets.
Methods
Animals
Male and female P. obesus, aged 7–9 weeks (Harlan, Jerusalem, Israel) were fed low-energy chow (LE 10 kJ/g) until the age of 14–15 weeks, when all animals except for an ‘LE’ group, were transferred to an ad libitum high-energy diet (HED 13 kJ/g). Body weight (BW), morning blood glucose (mBG) and HbA1c were measured once weekly. After 4–5 weeks, animals were killed and based on mBG the animals were categorised as responders (mBG ≥ 10 mmol/l) or non-responders (mBG < 10 mmol/l). This experimental protocol was repeated in order to obtain pancreases for characterisation of insulin content and BCM as described below. The study was approved by the Animal Experiments Inspectorate, Ministry of Justice, Denmark.
mBG
Blood samples were collected from the tail and mBG was measured as previously described by Vedtofte et al. [25].
Measurement of insulin and GLP-1 in P. obesus plasma
Blood was collected from the aorta and vena porta when the animals were killed and the plasma was stored at −80°C until analysis of insulin and GLP-1 was carried out.
Detection of insulin was by luminescence oxygen channelling immunoassay (LOCI) using two monoclonal antibodies (mAbs; mAb HUI-018 and mAb OXI005-03B) that recognise two different epitopes. The principle of the LOCI method is described in the electronic supplementary material (ESM).
Intact GLP-1 was detected with a method similar to that carried out for insulin determination by LOCI. However, two different mAbs were used: acceptor beads were conjugated with mAbF5 (which recognises amino acids 25–33 of GLP-1 [7–37]) and for biotinylation, mAb26.1 (which recognises amino acids 7–8 of GLP-1 [7–37]).
Measurements of GLP-1 and insulin in culture medium or KRB
GLP-1 from P. obesus islets in culture medium and GLP-1 from mouse and human islets in KRB were measured as described above, with the difference that the calibrators and controls were prepared in the corresponding matrix. Human insulin levels in KRB were measured by LOCI as described above with the following modifications: acceptor beads were conjugated with mAb RDI-TRK2IP10-D6C4, and mAb RDI-TRK2IP10-D3E7 was used for biotinylation. Calibrators and controls were prepared in the corresponding matrix.
Measurement of pancreatic GLP-1 and insulin content in P. obesus
Pancreases were removed from a subset of animals, weighed and immediately frozen in liquid nitrogen. For peptide extraction the tissue was dissolved in 1% (vol./vol.) trifluoroacetic acid and peptide material was isolated from using Sep-Pak C18 cartridges (Waters, Milford, MA, USA). Bound material was eluted with 70% (vol./vol.) ethanol and 0.1% (vol./vol.) trifluoroacetic acid, and lyophilised. Lyophilised material was dissolved phosphate buffered saline (+ albumin 0.1% [wt/vol.]) and the content of GLP-1 and insulin was measured by radioimmunoassay. Carboxy-terminal GLP-1 immunoreactivity was determined using antiserum 89390 [26], which has an absolute requirement for the intact amidated carboxy terminus of GLP-1 7–36 amide and has cross-reactivity of less than 0.01% with fragments truncated at the carboxy terminus and 89% with GLP-1 9–36 amide, the primary metabolite of DPP4-mediated degradation. Sensitivity was below 5 pmol/l, and the intra-assay coefficient of variation was below 10% [26]. Insulin was measured as previously described by Brand et al. [27].
cAMP measurements
Cells were harvested from a stable transfected baby hamster kidney (BHK) cell line producing the human GLP-1 receptor or the human glucagon receptor, and were stimulated with GLP-1, glucagon or islet culture medium. The response of GLP-1-, glucagon- or islet-medium-induced cAMP production was monitored using the FlashPlate Assay from PerkinElmer (Skovlunde, Denmark). The basic principle of the FlashPlate Assay is a competition between radioactive and non-radioactive cAMP for a fixed number of binding sites. Islet medium was incubated overnight at 4°C with or without a high-affinity glucagon mAb [27] or GLP-1 mAb (Mab26.1) prior to the cAMP assay.
Islet isolation
Islets were isolated from mice and P. obesus as described in the ESM. Human islets were obtained from Prodo Laboratories (Irvine, CA, USA). From one donor, a 43-year-old man, the islet purity was 75% and islet viability was 85%. From another donor, a 60-year-old man, the islet purity was 70% and islet viability was 95%. The study conformed to the ethical guidelines of Novo Nordisk for the use of human biological material. At arrival the islets were incubated free-floating in Petri dishes in RPMI 1640 medium (5.5 mmol/l glucose) supplemented with 5% (vol./vol.) human serum (Lonza, Basel, Switzerland) and 1% (vol./vol.) penicillin/streptomycin (P/S) and the perifusion experiment was performed the day after arrival.
In vitro islet studies
Freshly isolated P. obesus islets were handpicked and incubated in extracellular-matrix-coated 96 well plates (Biological Industries, Kibbutz Beit Haemek,Israel) with 10–15 islets/well in 150 μl RPMI 1640 (Invitrogen, Carlsbad, California) supplemented with 1% (vol/vol) penicillin/streptomycin, 10% (vol/vol) newborn calf serum and d-glucose at varying concentrations. The islets were incubated in a 5% CO2 humidified atmosphere at 37°C. After incubation the buffer was carefully removed from the islets and filtered through a 96 well filter plate (Multiscreen-DV from Millipore, Billerica, MA, USA) and stored at −20°C until analysis.
Mouse and human islets were placed in 96 well plates with 25 islets per well. The mouse islets were placed in the same medium as the P. obesus islets. Human islets were placed in RPMI 1640 (5.5 mmol/l glucose) supplemented with 5% (vol./vol.) human serum (Lonza) and 1% (vol./vol.) P/S. After 3 days, the islets were washed and incubated with 200 μl KRB (115 mmol/l NaCl, 4.7 mmol/l KCl, 2.6 mmol/l CaCl2, 1.2 mmol/l KH2PO4, 1.2 mmol/l MgSO4, 10 mmol/l HEPES, 0.2% (wt/vol.) BSA, 2 mmol/l glutamine, 5 mmol/l NaHCO3, 1% (vol./vol.) P/S, pH 7.4) for 1 h. After incubation the buffer was carefully removed from the islets and filtered through a 96-well filter plate and stored at −20°C until analysis.
Islet perifusion
Islets were washed in KRB and subsequently used in an islet perifusion experiment (Suprafusion 2500, Brandel, Lynge, Denmark). Four columns each with 40 islets were used. The islets were placed in Bio-gel P2 (BioRad, Copenhagen, Denmark) in the columns with a nylon mesh below and above the gel. The islets were initially perifused for 40 min with KRB containing 3 mmol/l glucose to obtain a stable baseline of insulin release. After 40 min the buffer was exchanged with 15 mmol/l glucose ± 0.5 μmol/l exendin (9–39) for 70 min (40–110 min). Finally, the buffer was exchanged to low glucose (3 mmol/l) for 30 min (110–140 min). The buffer was set to flow through the perifusion system at a rate of 0.3 ml/min. Samples were taken every 5 min from time 30 to 140 min. Samples were stored at −20°C and subsequently analysed for insulin.
Immunohistochemistry
Human pancreatic sections from weight- and age-matched healthy controls and from patients with type 2 diabetes (n = 7, respectively) were obtained from the National Disease Research Interchange. The method for staining the pancreas sections is described in the ESM.
Pancreas morphometry
The pancreases of a subset of the animals were examined histologically, as previously described by Raun et al. [28]. Briefly, pancreases were fixed in paraformaldehyde and sectioned according to a design-based stereological sampling scheme, the smooth fractionator method [29]. The sections were stained for insulin to visualise beta cells. BCM was evaluated stereologically in two to three sections with the origin of the sections blinded to the observer. The insulin staining intensity was graded semi-quantitatively on a scale of 0–5, with 0 being equal to islets characterised by absence of insulin staining and 5 equalling islets with insulin staining as seen in LE-fed P. obesus and in normal rat pancreas. The grading was carried out with the origin of the sections blinded to the observer.
Statistical methods
All data are expressed as mean ± SEM. Student’s t test was used for comparison of two groups. A value of p < 0.05 was considered statistically significant.
Results
Development of hyperglycaemia in HED-fed P. obesus
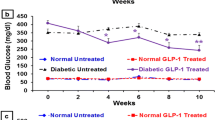
When transferred to the HED, about two-thirds of the animals (n = 26) became hyperglycaemic (mBG 15.5 ± 0.7 mmol/l) after 4 weeks. One-third of the animals (n = 15) were resistant to the HED and stayed normoglycaemic (mBG 5.7 ± 0.8 mmol/l; Fig. 1a).
Diabetes development in P. obesus. a Blood glucose in P. obesus on the HED. Responders (white circles; n = 26); non-responders (black circles; n = 15). b BCM in P. obesus after 4 weeks on the HED: non-responder, n = 19; hyperglycaemic, n = 26. Values for LE-fed controls (n = 10) are also shown. Non-resp, non-responder; hyperglyc, hyperglycaemic. **p < 0.01 compared with control. c Insulin score for the same animals as in b. ***p < 0.001 compared with control
BCM, insulin staining intensity, and insulin and GLP-1 content of P. obesus pancreases at death
After 4 weeks of HED, BCM was increased in responders (70 ± 9 mg/kg, n = 26, p < 0.05) and non-responders (87 ± 10 mg/kg, n = 19, p < 0.01), compared with animals on the LE diet (35 ± 7 mg/kg, n = 10; Fig. 1b). The intensity of the insulin staining decreased in the hyperglycaemic responders (1.1 ± 0.1, p < 0.001) and non-responders (2.6 ± 0.3, p < 0.001), as compared with LE-fed animals (5.0 ± 0.0; Fig. 1c). Pancreatic insulin content was higher in the non-responders compared with the hyperglycaemic animals (3.4 ± 0.5 nmol/g tissue [n = 9] vs 1.4 ± 0.3 nmol/g tissue [n = 16], p < 0.01) but was not significantly different from the LE group (2.1 ± 0.2 nmol/g tissue [n = 6]; Fig. 2a).
P. obesus plasma levels and pancreas content of insulin and active GLP-1 (a,c) Pancreas content of (a) insulin LE-fed control animals (n = 6), non-responders (n = 9) and hyperglycaemic (n = 16) animals and (c) GLP-1 amide of LE-fed control animals (n = 9), non-responders (n = 7) and hyperglycaemic (n = 9) animals.(b, d) Vena porta plasma levels of (b) insulin LE-fed control animals (n = 9), non-responders (n = 10) and hyperglycaemic (n = 19) animals and (d) intact GLP-1 from P. obesus after 4 weeks on the HED (non-responder, n = 20; hyperglycaemic, n = 30) or LE diet (control, n = 14). Non-resp, non-responder; hyperglyc, hyperglycaemic. *p < 0.05; ***p < 0.001 compared with control. †† p < 0.01 relative to hyperglycaemic animals
Portal vein levels of insulin were significantly higher in both the hyperglycaemic animals (5.5 ± 0.6 nmol/l [n = 19], p < 0.001) and in the non-responders (5.7 ± 0.9 nmol/l [n = 10], p < 0.001) compared with control LE animals (0.2 ± 0.05 nmol/l [n = 9]; Fig. 2b).
Analysis of the level of amidated GLP-1 in pancreatic extracts revealed a significant increase in the hyperglycaemic animals after 4 weeks on HED compared with LE-fed control animals (11.4 ± 2.2 pmol/g tissue [n = 9] vs 5.1 ± 1.3 pmol/g tissue [n = 9], p < 0.05; Fig. 2c). The pancreas content of intact GLP-1 in the non-responders was not significantly different from the LE controls (4.6 ± 1.1 pmol/g tissue [n = 7]). The increased GLP-1 level in the pancreases of hyperglycaemic animals was reflected in the portal vein plasma concentration, for which intact GLP-1 was also significantly higher in the hyperglycaemic group (9.8 ± 1.5 pmol/l, p < 0.05 [n = 30]) compared with the LE control group (4.3 ± 0.3 pmol/l [n = 14]), while GLP-1 levels in the non-responders (5.4 ± 0.8 pmol/l [n = 20]) were not different from LE controls (Fig. 2d). In contrast, for all animal groups plasma levels of intact GLP-1 in the aorta were below or only slightly above the quantification limit of the assay (0.7 pmol/l; data not shown).
GLP-1 release from P. obesus islets
To characterise the GLP-1 release further, accumulated GLP-1 release was analysed over 24 h in freshly isolated islets. Islets from hyperglycaemic animals released significantly more GLP-1 than islets from control animals (28.2 ± 4.4 pmol/l vs 5.8 ± 2.4, p < 0.01; Fig. 3a).
Release of intact GLP-1 from P. obesus islets in vitro. a Release of intact GLP-1 from freshly isolated P. obesus islets from control animals on the LE diet and from hyperglycaemic (hyperglyc) animals on HED over a 24 h incubation. Data represent islets isolated from four control animals and from six hyperglycaemic animals. b Glucose-induced release of GLP-1 from islets from P. obesus on the LE diet cultured for 24 h (black bars) or 6 days (white bars) at 3, 12 or 25 mmol/l glucose. Medium accumulated over 24 h; for the 6 day incubation the medium was changed between days 5 and 6. Data are mean ± SEM of three independent experiments. *p < 0.05; **p < 0.01 compared with control
Glucose-induced GLP-1 release from P. obesus islets
As diabetes is characterised by hyperglycaemia, we investigated if GLP-1 production by P. obesus islets could be increased by chronically elevated glucose levels in vitro. Incubation of control islets, isolated from P. obesus on the LE diet, for 24 h in 3, 12 or 25 mmol/l glucose did not lead to glucose-dependent changes in GLP-1 release (Fig. 3b). However, after 6 days of incubation a significant dose-dependent increase in GLP-1 release during the last 24 h of the 6 day culture period was observed (29 ± 7; 60 ± 6 [p < 0.05] and 91 ± 9 pmol/l [p < 0.01] for 3, 12 and 25 mmol/l glucose, respectively [n = 3]; Fig. 3b).
GLP-1 release from human and mouse islets
To establish if GLP-1 release could also be induced in human islets, isolated islets (pre-cultured in medium containing 5.5 mmol/l glucose for 3 days) were incubated for 1 h in KRB. A considerable amount of GLP-1 (72 ± 3 fmol islet−1/h−1 × 100 [n = 4]) was measured, whereas the release from mouse islets was very low (3.0 ± 2.5 fmol islet−1/h−1 × 100 [n = 3]; Fig. 4a). The functional significance of the GLP-1 released from human islets was assessed in an islet perifusion experiment. Addition of the GLP-1 receptor antagonist exendin (9–39) markedly (54%) reduced the glucose-stimulated insulin secretion (GSIS) in these islets (insulin AUC 30 ± 9 vs 65 ± 4 ng/100 islets, p < 0.05; Fig. 4b, c). Data are shown from one experiment out of two experiments from two donors yielding similar results (52% reduction for donor two). The results indicate that the GLP-1 receptor is active in these islets.
GLP-1 release from mouse and human islets. a Intact GLP-1 released into KRB in a 1 h incubation (human data are mean ± SEM of four independent experiments representing four donors). Mouse islets, n = 3. b Total insulin secreted (insulin AUC) in perifusion experiment shown in c. c Islet perifusion experiment on human islets. Effect of GLP-1 receptor antagonist exendin (9–39) on GSIS. Black circles, glucose at: (1) 3 mmol/l; (2) 15 mmol/l; and (3) 3 mmol/l. White circles, glucose at: (1) 3 mmol/l; (2) 15 mmol/l + exendin (9–39); and (3) 3 mmol/l. Data in b and c are from an experiment using islets from one donor with each condition run in quadruplicate (represented by error bars). The experiment was repeated on islets from a second donor, yielding similar results
Bioactivity of GLP-1 released from P. obesus islets
Next we evaluated the bioactivity of the GLP-1 released from the P. obesus islets. Incubation of GLP-1 receptor-producing BHK cells with supernatant fraction from P. obesus islets cultured for 4 days in 25 mmol/l glucose-activated cAMP production to the same level as treatment of the cells with 100 pmol/l synthetic GLP-1 peptide (Fig. 5a). This receptor activation was, to a large extent, blocked by prior incubation of the islet medium with an antibody directed to the NH2-terminus of GLP-1 (mAb26.1; Fig. 5a). It is known that glucagon can activate the GLP-1 receptor with low potency (EC50 ≈ 1 nmol/l) [30]. Islet culture supernatant fractions contain glucagon released from alpha cells that could be responsible for activation of the GLP-1 receptor in this assay. In order to demonstrate that active GLP-1 and not glucagon was responsible for the production of cAMP, the GLP-1 receptor activation experiment was also performed in the presence of a high-affinity glucagon mAb [27]. The high-affinity glucagon mAb had no effect on the GLP-1 receptor activation by the islet medium (Fig. 5a). It did, however, completely inhibit the glucagon receptor activation (Fig. 5b). Addition of islet supernatant fraction to non-transfected BHK cells resulted in no induction of cAMP production (Fig. 5c). This confirmed that GLP-1 released from the islets is an active form of the peptide.
Bioactivity of GLP-1 released by islets into medium. a cAMP production by activation of the GLP-1 receptor expressed in BHK cells by islet medium with and without pre-incubation with glucagon antibody or GLP-1 antibody; 100 pmol/l GLP-1 serves as positive control b cAMP production by activation of the glucagon receptor produced in BHK cells by islet medium with and without pre-incubation with glucagon antibody; 100 pmol/l glucagon serves as positive control. c cAMP production by non-transfected BHK cells stimulated with islet medium. The data shown are mean ± SEM from a single representative experiment performed in duplicate. Glu Ab, high-affinity glucagon antibody
Expression of GLP-1 in the pancreas
Using antisera specific to the N-terminus of the active form of GLP-1 as well as antisera specific for the 7–36 amide form of the GLP-1 peptide, we performed immunocytochemistry to examine the localisation of GLP-1 in the islets. In most glucagon immunoreactive cells, both the C-terminal (amidated) and the N-terminal immunoreactivity of GLP-1 were detectable in control and hyperglycaemic P. obesus (Fig. 6a, b) and the merge is shown by a pinkish colour. There was no colocalisation of GLP-1 amide and insulin. Also in human pancreas, there was a strong colocalisation of GLP-1 amide, N-terminally derived biologically active GLP-1 and glucagon in sections from both controls and patients with type 2 diabetes and no colocalisation with insulin (Fig. 6c, d).
Pattern of glucagon, insulin and PC1/3- and biologically active forms of GLP-1 in pancreas. a–d Colocalisation of glucagon with GLP-1 amide (a, c) and N-terminal GLP-1 (b, d) in normal and hyperglycaemic P. obesus and human pancreas. Nearly all glucagon cells are co-immunoreactive as denoted by a pink-purple colour. e–h Colocalisation of PC1/3 in insulin and some glucagon immunoreactive cells in normal and diabetic P. obesus and human pancreas. The white arrow marks glucagon-positive cells producing PC1/3. Scale bars 20 μm. N-Term, N-terminal
PC2 and PC1/3 are produced in alpha cells of hyperglycaemic P. obesus and of patients with type 2 diabetes
To further explore the production of GLP-1 in the islets and to establish whether changes in the processing enzymes responsible for processing proglucagon to glucagon (PC2) or GLP-1 (PC1/3) were changed in hyperglycaemic vs control islets from P. obesus as well as in islets from humans, histochemical analyses were performed. Pancreas sections from P. obesus and humans were stained for insulin, glucagon and PC1/3. The beta cells stained strongly for PC1/3 while the majority of alpha cells were weakly positive for PC1/3, and the surrounding exocrine pancreas showed no immunoreactivity (Fig. 6e-h). As seen in Fig. 6f, h the diabetic state results in a very different staining pattern. In hyperglycaemic P. obesus, nearly all the alpha cells now stained more intensely for PC1/3 (Fig. 6f) and some beta cells lost immunoreactivity. In sections from humans with type 2 diabetes, either a low level was observed, but not in every glucagon immunoreactive cell, or the staining was not much different from the non-diabetic state (Fig. 6g, h).
PC2 staining (co-staining with glucagon and insulin) of human and P. obesus normal and diabetic pancreas tissue is shown in ESM Fig. 1. In LE-fed P. obesus pancreas, PC2 was colocalised with both insulin and glucagon, while in the hyperglycaemic state, PC2 was only found in the alpha cells. This contrasts with the human pancreas, where PC2 was found in both insulin and glucagon cells in pancreases from control and type 2 diabetes patients.
Discussion
We have provided evidence that pancreatic islets from P. obesus produce fully processed GLP-1 during the development of hyperglycaemia and that this production can also be induced in vitro following culture of P. obesus islets in high glucose. Pancreatic alpha cells from patients with type 2 diabetes and P. obesus stained positive for GLP-1, and human islets released GLP-1 in vitro. Based on our observations we hypothesise that this paracrine GLP-1 system may play a role in adult islets in regulating BCM and function when metabolic stress is imposed on the beta cells e.g. during the development of diabetes.
The pancreatic beta cells are located quite distantly from the GLP-1 producing L-cells in the intestine. It is well established that only a fraction of the intestinal GLP-1 reaches the beta cell via the circulation because GLP-1 is exposed to inactivation by DPP-IV immediately after its release [10, 11]. Bearing in mind this rapid decline in the peripheral GLP-1 signal arising from the L-cells, it is tempting to hypothesise the existence of a local GLP-1 signalling system in the islets close to the beta cell GLP-1 receptors. Indeed, proglucagon and PC1/3 colocalise in the pancreas at certain fetal stages, suggesting an important and transient role of GLP-1 during pancreas development [16, 18]. In the present study, we have shown also that the adult islet harbours a local GLP-1 signalling system, as has also been suggested by other studies [13]. Interestingly, a paracrine system involving GLP-1 was recently reported where GLP-1 produced locally by taste cells and acting via GLP-1 receptors produced on nearby afferent nerve fibres, serves to modulate taste sensitivity [31]. To what extent GLP-1 produced by the alpha cells will reach the beta cells is controversial, based on the proposed circulation from beta to alpha cells [32]. Nevertheless, it has recently been shown that islets in which PC1/3 production is enhanced by gene transfer display improved GSIS and are less sensitive to cytokine treatment. When transplanted to a mouse model of type 1 diabetes the GLP-1-producing islets perform better than normal islets [15]. Also, cell therapy with PC1/3-producing alpha cells improves glucose handling in db/db mice [33].
The mechanism leading to upregulation of GLP-1 from alpha cells needs to be determined. One possibility is increased production or activity of PC1/3. Indeed it has been shown that PC1/3 is upregulated by high glucose in alpha cells [34] and in hyperglycaemic db/db mice [17]. Therefore, it is possible that this is also the mechanism in our studies. Our data did show heterogeneity of PC1/3 production with mainly low but detectable levels in glucagon immunoreactive cells. Using two different antisera, we were able to demonstrate N-terminally biologically active GLP-1 as well as amidated GLP-1, both of which result from PC1/3 cleavage of proglucagon, providing further evidence of PC1/3 activity in alpha cells. Interestingly, fully processed GLP-1 can be detected in the plasma of humans with PC1/3 deficiency [35] and this finding emphasises that there are some aspects of proglucagon processing that are yet to be understood. As an alternative possibility there could be an inherent presence of PC1/3 in alpha cells which, during upregulation of transcription and translation of proglucagon, would lead to increased levels of GLP-1 accompanied by increased levels of circulating glucagon. In the present study, however, we did not see an increase in circulating glucagon (data not shown) accompanying the increase in GLP-1 in P. obesus.
When P. obesus were fed a HED the BCM increased but the insulin content of the pancreases of non-responders was significantly higher than in hyperglycaemic P. obesus, and so was the intensity of insulin staining, although there was no difference in BCM. The reason for this could be that BCM is a measure of the volume of the area of the endocrine pancreas that has any positive staining for insulin, and is not related to the quantity of insulin in the cells. If there is an expansion of the islet area with peripheral weak insulin staining, this will be reflected in an increased BCM but not indicative of the level of functionality. Insulin content of the pancreas and intensity of insulin immunoreactivity could be a better estimate for a functional BCM. We also saw the same level of increase of insulin in vena porta vessels from non-responders and hyperglycaemic animals compared with the LE controls, despite profound differences in mBG levels. This suggests that the responders are not able to compensate for elevated mBG by increasing insulin secretion, probably because of an inadequate functional BCM [25].
The marked inhibition by exendin (9–39) on GSIS in the isolated human islets demonstrates that the GLP-1 receptors in these islets are already active. This could be explained by constitutively active receptors [36] or by an adequate amount of GLP-1 present locally to activate the receptor. The level of active GLP-1 measured in the islet medium of 1 h incubations as well as the blunting of the GSIS by the GLP-1R antagonist exendin (9–39) favours the latter possibility. In addition, in similar experimental setups we failed to see the expected increment in insulin release by addition of exogenous GLP-1 (data not shown). So why is alpha cell GLP-1 production switched on in healthy human islets? There could be several reasons for this. For example, they may have experienced metabolic stress, such as hypoxia before or during the isolation procedure, shipment or subsequent culture before the experiments were undertaken. Further studies are needed to explore whether GLP-1 secretion from alpha cells in humans is a real phenomenon under normal or diabetic conditions and to what extent failure in this process could be involved in the pathogenesis of diabetes.
Abbreviations
- BCM:
-
Beta cell mass
- BHK:
-
Baby hamster kidney
- DPP-IV:
-
Dipeptidyl peptidase 4
- GLP-1:
-
Glucagon-like peptide-1
- GSIS:
-
Glucose-stimulated insulin secretion
- HED:
-
High-energy diet
- LE:
-
Low-energy chow
- LOCI:
-
Luminescence oxygen channelling immunoassay
- mAb:
-
Monoclonal antibody
- mBG:
-
Morning blood glucose
- PC:
-
Prohormone convertase
- P/S:
-
Penicillin/streptomycin
References
Anonymous (1995) UK prospective diabetes study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes 44:1249–1258
Drucker DJ (2006) The biology of incretin hormones. Cell Metab 3:153–165
Farilla L, Bulotta A, Hirshberg B et al (2003) Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology 144:5149–5158
Bregenbolt S, Moldrup A, Blume N et al (2005) The long-acting glucagon-like peptide-1 analogue, liraglutide, inhibits beta-cell apoptosis in vitro. Biochem Biophys Res Commun 330:577–584
Farilla L, Hui H, Bertolotto C et al (2002) Glucagon-like peptide-1 promotes islet cell growth and inhibits apoptosis in Zucker diabetic rats. Endocrinology 143:4397–4408
Wang Q, Brubaker PL (2002) Glucagon-like peptide-1 treatment delays the onset of diabetes in 8 week-old db/db mice. Diabetologia 45:1263–1273
Perfetti R, Zhou J, Doyle ME, Egan JM (2000) Glucagon-like peptide-1 induces cell proliferation and pancreatic-duodenum homeobox-1 expression and increases endocrine cell mass in the pancreas of old, glucose-intolerant rats. Endocrinology 141:4600–4605
Rouillé Y, Martin S, Steiner DF (1995) Differential processing of proglucagon by the subtilisin-like prohormone convertases PC2 and PC3 to generate either glucagon or glucagon-like peptide. J Biol Chem 270:26488–26496
Rouillé Y, Kantengwa S, Irminger JC, Halban PA (1997) Role of the prohormone convertase PC3 in the processing of proglucagon to glucagon-like peptide 1. J Biol Chem 272:32810–32816
Vilsboll T, Agerso H, Krarup T, Holst JJ (2003) Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J Clin Endocrinol Metab 88:220–224
Deacon CF, Johnsen AH, Holst JJ (1995) Degradation of glucagon-like peptide-1 by human plasma in vitro yields an N-terminally truncated peptide that is a major endogenous metabolite in vivo. J Clin Endocrinol Metab 80:952–957
Heller RS, Aponte GW (1995) Intra-islet regulation of hormone secretion by glucagon-like peptide-1-(7–36) amide. Am J Physiol Gastrointest Liver Physiol 269:G852–G860
Masur K, Tibaduiza EC, Chen C, Ligon B, Beinborn M (2005) Basal receptor activation by locally produced glucagon-like peptide-1 contributes to maintaining beta cell function. Mol Endocrinol 19:1373–1382
Mojsov S, Kopczynski MG, Habener JF (1990) Both amidated and nonamidated forms of glucagon-like peptide I are synthesized in the rat intestine and the pancreas. J Biol Chem 265:8001–8008
Wideman RD, Yu ILY, Webber TD et al (2006) Improving function and survival of pancreatic islets by endogenous production of glucagon-like peptide 1 (GLP-1). Proc Natl Acad Sci USA 103:13468–13473
Wilson ME, Kalamaras JA, German MS (2002) Expression pattern of IAPP and prohormone convertase 1/3 reveals a distinctive set of endocrine cells in the embryonic pancreas. Mech Dev 115:171–176
Kilimnik G, Kim A, Steiner DF, Hara M (2010) Intraislet production of GLP-1 by activation of prohormone convertase 1/3 in pancreatic alpha-cells in mouse models of beta-cell regeneration. Islets 2:149–155
Thyssen S, Arany E, Hill DJ (2006) Ontogeny of regeneration of beta-cells in the neonatal rat after treatment with streptozotocin. Endocrinology 147:2346–2356
Nie Y, Nakashima M, Brubaker PL et al (2000) Regulation of pancreatic PC1 and PC2 associated with increased glucagon-like peptide 1 in diabetic rats. J Clin Invest 105:955–965
Kalderon B, Gutman A, Levy E (1986) Characterization of stages in development of obesity-diabetes syndrome in sand rat (Psammomys obesus). Diabetes 35:717–724
Shafrir E, Ziv E (1998) Cellular mechanism of nutritionally induced insulin resistance: The desert rodent Psammomys obesus and other animals in which insulin resistance leads to detrimental outcome. J Basic Clin Physiol Pharmacol 9:347–385
Kaiser N, Yuli M, Ueckaya G et al (2005) Dynamic changes in beta-cell mass and pancreatic insulin during the evolution of nutrition-dependent diabetes in Psammomys obesus−impact of glycemic control. Diabetes 54:138–145
Donath MY, Gross DJ, Cerasi E, Kaiser N (1999) Hyperglycemia-induced beta-cell apoptosis in pancreatic islets of Psammomys obesus during development of diabetes. Diabetes 48:738–744
Kaiser N, Nesher R, Donath MY et al (2005) Psammomys obesus, a model for environment-gene interactions in type 2 diabetes. Diabetes 54:S137–S144
Vedtofte L, Bödarsdottir TB, Gotfredsen CF, Karlsen AE, Knudsen LB, Heller RS (2010) Liraglutide, but not vildagliptin, restores normoglycaemia and insulin content in the animal model of type 2 diabetes, Psammomys obesus. Regul Pept 160:106–114
Orskov C, Rabenhoj L, Wettergren A, Kofod H, Holst JJ (1994) Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes 43:535–539
Brand CL, Rolin B, Jorgensen PN, Svendsen I, Kristensen JS, Holst JJ (1994) Immunoneutralization of endogenous glucagon with monoclonal glucagon antibody normalizes hyperglycaemia in moderately streptozotocin-diabetic rats. Diabetologia 37:985–993
Raun K, von Voss P, Gotfredsen CF, Golozoubova V, Rolin B, Knudsen LB (2007) Liraglutide, a long-acting glucagon-like peptide-1 analog, reduces body weight and food intake in obese candy-fed rats, whereas a dipeptidyl peptidase-iv inhibitor, vildagliptin, does not. Diabetes 56:8–15
Gundersen HJG (2002) The smooth fractionator. J Microsc 207:191–210
Runge S, Wulff BS, Madsen K, Brauner-Osborne H, Knudsen LB (2003) Different domains of the glucagon and glucagon-like peptide-1 receptors provide the critical determinants of ligand selectivity. Br J Pharmacol 138:787–794
Martin B, Dotson CD, Shin YK et al (2009) Modulation of taste sensitivity by GLP-1 signaling in taste buds. Ann NY Acad Sci 1170:98–101
Bosco D, Armanet M, Morel P et al (2010) Unique arrangement of alpha and beta cells in human islets of Langerhans. Diabetes 59(1):202–1210
Wideman RD, Gray SL, Covey SD, Webb GC, Kieffer TJ (2008) Transplantation of PC1/3-expressing α cells improves glucose handling and cold tolerance in leptin-resistant mice. Mol Ther 17:191–198
McGirr R, Ejbick CE, Carter DE et al (2005) Glucose dependence of the regulated secretory pathway in alpha TC1-6 cells. Endocrinology 146:4514–4523
Jackson RS, Creemers JWM, Farooqi IS et al (2003) Small-intestinal dysfunction accompanies the complex endocrinopathy of human proprotein convertase 1 deficiency. J Clin Invest 112:1550–1560
Serre V, Dolci W, Schaerer E et al (1998) Exendin-(9–39) is an inverse agonist of the murine glucagon-like peptide-1 receptor: implications for basal intracellular cyclic adenosine 3′, 5′-monophosphate levels and β cell glucose competence. Endocrinology 139:4448–4454
Acknowledgements
We would like to thank L. Eriksen, H. Jensen-Holm, T. Rørmose Hansen, T. Merethe Olsen and S. Primdahl for technical assistance, and the National Disease Research Interchange (NDRI) for providing human pancreatic sections. We thank D. F. Steiner for providing the PC2 antibody. K. Maedler is supported by the German Research Foundation (DFG, Emmy Noether Programme MA4172/1-1).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. M. K. Hansen and T. B. Bödvarsdottir are joint first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 57.9 kb)
ESM Table 1
Antibodies (PDF 8.62 kb)
ESM Fig. 1
Pattern of insulin, glucagon and PC2 in pancreas. a–d PC2 is colocalised with insulin and glucagon cells in the both control P. obesus and human pancreas, but lower levels are observed in the glucagon cells pancreas from type 2 diabetic patients, while it is produced in abundance in the insulin cells. In hyperglycaemic P. obesus, PC2 is completely lost in the insulin cells and maintained in most of the glucagon immunoreactive cells. Size bar 20 μm (PDF 518 kb) (PDF 518 kb)
Rights and permissions
About this article
Cite this article
Hansen, A.M.K., Bödvarsdottir, T.B., Nordestgaard, D.N.E. et al. Upregulation of alpha cell glucagon-like peptide 1 (GLP-1) in Psammomys obesus—an adaptive response to hyperglycaemia?. Diabetologia 54, 1379–1387 (2011). https://doi.org/10.1007/s00125-011-2080-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-011-2080-1