Abstract
Aim/hypothesis
Type 1 diabetes (T1D) is an autoimmune disease with multiple susceptibility genes. The aim of this study was to determine whether combining IDDM1/HLA and IDDM2/insulin (INS) 5′ variable number of tandem repeat locus (VNTR) genotypes improves T1D risk assessment.
Methods
Patients with T1D (n=488), control subjects (n=846), and offspring of parents with T1D (n=1122) were IDDM1 and IDDM2 genotyped. Offspring were followed for islet autoantibodies and T1D from birth until the age of 2 to 12 years.
Results
Compared to the I/I INS VNTR genotype, the I/III and III/III genotypes reduced T1D risk conferred by IDDM1/HLA in all HLA genotype categories of the case-control cohort by 1.6-fold to three-fold. The highest T1D risk was associated with INS VNTR class I/I plus HLA DR3/DR4-DQ8 (20.4% in patients, 0.6% in control subjects) or HLA DR4-DQ8/DR4-DQ8 (6.3% in patients, 0.2% in control subjects). In the offspring, HLA DR3/DR4-DQ8 and DR4-DQ8/DR4-DQ8 conferred increased risk for early development of islet autoantibodies (14.6% and 12.9% by age 2 years). Offspring with these high risk IDDM1 genotypes plus the INS VNTR class I/I genotype (n=71; 6.3%) had the highest risk of developing islet autoantibodies (21.8% by age 2 years vs 8.9% in offspring with high risk IDDM1 plus INS VNTR class I/III or III/III genotypes, p<0.05) and T1D (8.5% by age 6 years vs 4.3%). Offspring who developed autoantibodies to multiple antigens had increased frequencies of both high risk IDDM1 and IDDM2 genotypes (p<0.0001), whereas offspring who developed autoantibodies to GAD only had increased frequencies of high risk IDDM1 and protective IDDM2 genotypes, suggesting that IDDM2 influences the autoimmune target specificity.
Conclusion/Interpretation
Combining IDDM1 and IDDM2 genotyping identifies a minority of children with an increased T1D risk.
Similar content being viewed by others
Type 1 diabetes (T1D) is an autoimmune disease with multiple susceptibility genes [1, 2]. The major susceptibility genes are found within the HLA class II region of chromosome 6 (IDDM1). A second genetic susceptibility locus has been mapped by a variable number of tandem repeat (VNTR) in the insulin gene (INS) promoter region (IDDM2)[3, 4]. Identification of T1D-prone individuals through genotyping would facilitate prospective investigation of early environmental triggers and primary intervention trials. Such studies would become feasible if they could include only subjects with highest T1D risk and if early outcome markers were identified. Several prospective studies have shown that the islet autoimmunity that precedes T1D onset can be seen very early in life and can be used as an outcome marker to study triggers of autoimmunity [5, 6, 7]. We, and others, have shown that IDDM1 genotyping can identify newborns with an increased risk of developing T1D-associated autoimmunity [8, 9, 10]. Here we determine whether combining IDDM1 and IDDM2 genotyping improves risk assessment. We identify IDDM1 and IDDM2 T1D risk genotypes in a case-control cohort from Germany, and subsequently evaluate the predictive value of genetic pre-screening by follow-up for autoimmunity and T1D within the prospective BABYDIAB newborn offspring study. By combining IDDM1 and IDDM2 genotyping it was possible to identify a minority of newborns of parents with T1D who had a greater than 20% risk to develop persistent multiple islet autoantibodies by the age of 2 years and almost 10% risk to develop T1D by the age of 6 years. These findings allow primary intervention programs to delay T1D onset to be seriously considered and designed.
Subjects and Methods
Subjects
DNA samples were obtained from a total of 538 Caucasian patients with T1D from Germany. These were parents of children who participated in the BABYDIAB study [5]. Their mean (SD) age of T1D onset was 17.5 (+8.5) years, 397 were female, 66 had a first degree relative (parent or sibling) with T1D, and 53% were living in the northern half of Germany (Zip code 01558–59889). The female bias in patients was due to a recruitment restriction in the first few years of the BABYDIAB study allowing only families in which mothers had T1D to participate. As control subjects, DNA was obtained from the non-diabetic parents of the BABYDIAB children (n=610) and from 307 unrelated non-diabetic volunteers without family history of T1D (45% were females and 55% were living in the northern half of Germany). DNA samples were also obtained from 1249 offspring of mothers (n=785), fathers (n=436), or both parents (n=28) with T1D. All offspring were participating in the German BABYDIAB study and were prospectively followed from birth in regular intervals up to the age of 12 years (median follow-up time 5.6 years; range 1.3–12.3 years) [5]. During follow-up T1D-associated islet autoantibodies [insulin autoantibodies (IAA), GAD autoantibodies, antibodies to the protein tyrosine phosphatase IA-2, and islet cell autoantibodies] were measured at 9 months, 2 years, 5 years, 8 years, and 11 years of age. Children with positive autoantibodies were followed with blood samples at 6 to 12 month intervals. Of the 1249 offspring, 63 have developed persistent (positive in at least two consecutive samples) islet autoantibodies, including 40 with autoantibodies to more than one antigen (multiple autoantibodies). Of these 63, 19 developed persistent islet autoantibodies by 9 months, an additional 25 by 2 years, an additional 15 by 5 years, and an additional 4 by 8 years. 18 offspring with persistent islet autoantibodies and none of the islet autoantibody negative offspring have developed T1D. IDDM1 HLA DR-DQ genotyping and IDDM2 INS VNTR genotyping was carried out on 488 T1D patients, 846 control subjects and 1122 offspring. The remaining 50 patients, 71 control subjects and 127 offspring were IDDM1 HLA DR-DQ genotyped only. Written informed consent was obtained from all subjects who participated in the study. The study was approved by the Bayerische Landesärztekammer ethical committee (Nr. 95357).
HLA typing
HLA-DRB1-DQA1 and -DQB1 alleles were typed using polymerase chain reaction (PCR)-amplified DNA and non-radioactive oligonucleotide probes (sequence-specific oligonucleotide typing SSO) in the laboratories of Ekkehard Albert (Ludwig-Maximilians-University, Munich). Genomic DNA was isolated from fresh peripheral blood cells (EDTA-blood) and diluted to 250 µg/ml in TE buffer and stored at −20°C until use. Genomic DNA (1 µg) was amplified by PCR using DRB1, DQB1 or DQA1 generic primers, spotted onto nylon membranes (Roche, Mannheim, Germany) and hybridized with 15 DRB1-, 17 DQA1- or 20 DQB1-allele-specific oligonucleotides, respectively. The hybridized oligonucleotides 3′end labelled with digoxigenin-11–2′,3′-dideoxyuridine-5′-triphosphate (Roche) were detected using anti-dioxigenin-AP Fab fragments (Roche) and visualized with the chemiluminescent substrate CSPD (Roche).
INS VNTR
Subjects were typed using HphI digestion of PCR amplification products of the region of interest as previously described [3]. PCR amplification was carried out in 96-well microtitre plates. Each 25 µl reaction tube contained 100 ng DNA, 2.5 µl 10 × reaction buffer (Eppendorf, Hamburg, Germany), 200 mmol/l desoxynucleotide triphosphate (dNTP)-Mix, 1.0 ng from each primer, 5.0 µl Taq-Enhancer (Eppendorf) and 0.5 U of Taq-Polymerase (Eppendorf). The PCR was carried out in 32 cycles (94°C 20 s, 57°C/15 s, 72°C/ 30 s). Primers for PCR were: 23 HphI 360F 5′-AGCAGGTCTGTTCCAAGG-3′ and 23 HphI 360R 5′-CTTGGGTGTGTAGAAGAAGC-3′. 25 µl of each PCR product was digested in 2 U of HphI at 37°C for 2 h, and each digested product was detected by ethidium bromide staining after electrophoresis in a 3% NuSieve gel (FMC BioProducts, Rockland, Me., USA).
Islet Autoantibody Testing
Autoantibodies to insulin (IAA), GAD, and IA-2 were measured in offspring samples by radiobinding assays [5, 7]. The upper limit of normal was defined by q-q plots [5]. Using these thresholds for positivity, the assays had sensitivities and specificities of 80% and 94% (GAD antibodies), 58% and 100% (IA-2 antibodies), and 30% and 98% (IAA) in the First DASP Proficiency [11].
Statistical analysis
Allele, haplotype, and genotype frequencies were calculated for patients and the control group. Where both parents and offspring were typed, haplotypes were unambiguously defined by transmission. In families where unambiguous haplotype could not be defined, haplotypes were assigned by known HLA-DRB1-DQA1-DQB1 combinations. Odds Ratios and their p values were calculated by logistic regression, using Stata Statistical Software, Release 7.0 (Stata, College Station, Tex., USA). The Chi-square test for trend was used to compare genotype frequencies between age groups. Fisher's exact test was used to compare genotype frequencies between multiplex and single case families. Life table analysis was used to calculate the cumulative islet autoantibody frequency (positive predictive value) [8] using the Statistical Package for Social Science (SPSS, Chicago, Ill., USA). A p value of less than 0.05 was considered statistically significant.
Results
HLA-DRB1-DQA1-DQB1 genotypes in patients, controls and offspring cohorts
HLA-DRB1-DQA1-DQB1 genotypes conferring T1D susceptibility or protection in the case-control cohort are shown in Table 1. Patients who developed T1D before the age of 10 years (n=104) had a higher frequency of the very high risk DRB1*03-DQA1*0501-DQB1*0201/DRB1*04-DQA1*0301-DQB1*0302 (DR3/DR4-DQ8) genotype than patients who developed T1D after the age of 10 years (36.5% vs 24.1%, p <0.02, Table 2). Patients who had first degree relatives with T1D (n=66) had a higher frequency of the high risk DRB1*04-DQA1*0301-DQB1*0302/DRB1*04-DQA1*0301-DQB1*0302 (DR4-DQ8/DR4-DQ8) genotype than patients without a family history of T1D (18.1% vs 8.1%, p <0.05). No differences were observed in genotype frequencies between male and female patients (very high risk: 22.7% vs 28.0%; high risk: 9.2% vs 9.3%; moderate DR4-DQ8:15.6% vs 15.6%; Moderate DR3:13.5% vs 9.8%; neutral: 29.8% vs 30.7%; protective: 9.2 vs 6.5%) or between male and female control subjects. Within the case-control cohort, DQ8 conferred a lower susceptibility when together with DRB1*0402, DRB1*0403, or DRB1*0404 alleles than with DRB1*0401 (all p<0.02; data not shown).
The high-risk HLA DR3/DR4-DQ8 and DR4-DQ8/DR4-DQ8 genotypes were found in 155 (8% and 4.4%, respectively) of 1249 offspring from patients with T1D. A further 122 (9.8%) offspring had DR4-DQ8 genotypes conferring moderate T1D risk, and 61 (4.9%) offspring had DR3 genotypes conferring moderate risk (Table 1). DQ8 haplotypes with the less susceptible DRB1*04 alleles were found in 20 (*0402), 4 (*0403), and 41 (*0404) of the 1249 offspring (data not shown).
INS VNTR genotype frequency
The INS VNTR class I allele frequency in patients was 86.5% compared with 75% in control subjects (p <0.0001). The I/I, I/III, and III/III genotypes were found in 75%, 23.2%, and 1.8% of patients with T1D compared to 56%, 37.2%, and 6.8% of control subjects (p <0.0001; Table 2). This difference was similar in males (78.1%, 19.5%, 2.3% in patients vs 54.9%, 38.3%, 6.8% in control subjects, p <0.0001) and females (73.9%, 24.1%, 1.7% in patients vs 57.5%, 35.2%, 7.3% in control subjects, p <0.0001). T1D risk was reduced for both class I/III (OR 0.46) and III/III (OR 0.2) in comparison to class I/I genotypes suggesting that the class III allele confers semi-dominant protection. INS VNTR genotype frequencies in patients did not differ with respect to age of diabetes onset, or family history of T1D (data not shown).
The INS VNTR genotype modified T1D risk in all HLA DR-DQ genotype risk categories (Table 2). The INS VNTR class I/III and III/III genotypes were associated with a decreased T1D risk compared to INS VNTR I/I in the presence of HLA DR-DQ genotypes conferring very high and high T1D risk (OR 0.32; p <0.05 class I/III or III/III vs class I/I), moderate T1D risk (OR 0.43; p =0.01), neutral T1D risk (OR 0.39; p <0.0001), or protection (OR 0.61; p =0.21). Modification of T1D risk by INS VNTR in the different HLA DR-DQ risk categories was observed in both males (OR=0.24, 0.26, 0.41, and 0.61 for INS VNTR class I/I vs I/III or III/III in HLA high risk, moderate risk, neutral, or protective genotypes, respectively) and females (ORs of 0.56, 0.50, 0.32, and 0.62 for INS VNTR class I/I vs I/III or III/III in HLA high risk, moderate risk, neutral, or protective genotypes, respectively).
HLA-DRB1-DQA1-DQB1-INS VNTR genotypes and autoantibody/T1D risk in offspring
The cumulative frequency of islet autoantibodies and T1D in offspring according to HLA-DRB1-DQA1-DQB1 genotype is shown in Table 3 and Fig. 1. Autoantibody frequency was highest in offspring with the HLA DR3/DR4-DQ8 (21.1% by age 5 years) and DR4-DQ8/DR4-DQ8 (16.1% by age 5 years) genotypes (p<0.0001 vs 3.9% in offspring with other genotypes). Antibody frequency was also increased in offspring with the DR4-DQ8 containing moderate risk genotypes (9.3% by age 5 years; p<0.005 vs 3.1% in offspring with neutral and protective), but not in offspring with the moderate DR3 risk genotypes. Autoantibody frequency was highest in DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8 offspring who had the INS VNTR class I/I genotype (Table 4, Fig. 2). A total of 71 (6.3%) of 1122 offspring had these combined DRB1-DQA1-DQB1-INS VNTR genotypes. These 71 offspring had a 23.1% cumulative frequency of persistent autoantibodies already by the age of 2 years, a 21.1% frequency of persistent multiple antibodies by the age of 2 years, and an 8.5% cumulative frequency of T1D by the age of 6 years. Autoantibody frequency was higher in offspring with high risk DRB1-DQA1-DQB1-INS VNTR genotypes than those with only the high risk DRB1-DQA1-DQB1 genotypes (p<0.05). This difference was similar in children of mothers with T1D (21.1% cumulative frequency of autoantibodies by age 2 years in children with high risk DRB1-DQA1-DQB1-INS VNTR genotypes vs 8.4% in children with only the high risk DRB1-DQA1-DQB1 genotypes) and children of fathers with T1D (25.1% vs 8.5%; data not shown). INS-VNTR genotypes did not modify risk of developing islet autoantibodies in the offspring with moderate, neutral or protective IDDM1 HLA genotypes (2.6% by age 2 years in offspring with INS VNTR I/I vs 2.1% in offspring with I/III of III/III), but numbers of autoantibody positive cases in these offspring were low.
Life table analysis of developing at least one persistent islet autoantibody (A), at least two persistent islet autoantibodies (B), or Type 1 diabetes (C) in offspring of parents with Type 1 diabetes in the BABYDIAB study. Offspring are grouped by HLA-DR-DQ T1D risk category. The risk groups moderate DR3, neutral and protective are grouped together in C and shown by the dotted line. Offspring with very high, high, and moderate DR4 risk genotypes had increased risk for developing islet autoantibodies (p<0.0001, p<0.0001, p<0.005 vs remainder) and multiple islets autoantibodies (p<0.001, p<0.0001, p<0.01 vs remainder). T1D risk was increased in offspring with very high (p<0.0001) and high (p<0.001) risk genotypes
Life table analysis of developing at least one persistent islet autoantibody (A), at least two persistent islet autoantibodies (B), or Type 1 diabetes (C) in offspring of parents with Type 1 diabetes in the BABYDIAB study. Offspring are grouped by HLA-DR-DQ and INS VNTR genotype. Islet autoantibody frequencies are higher in offspring with high risk HLA DR-DQ and INS VNTR class I/I genotypes than offspring with high risk HLA DR-DQ and INS VNTR class I/III or III/III genotypes (p<0.05) or offspring with other genotypes (p<0.0001)
HLA-DRB1-DQA1-DQB1-INS VNTR genotypes and autoantibody target antigen
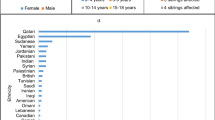
Persistent non-maternally acquired islet autoantibodies developed in 63 of the HLA typed offspring: 18 of these had the HLA DR3/DR4-DQ8, and eight the HLA DR4-DQ8/DR4-DQ8 genotypes, nine had protective and 16 neutral genotypes. Offspring who developed persistent autoantibodies to more than one antigen (n=40) had similar DRB1-DQA1-DQB1 genotypes to patients with T1D onset with an increase in DR3/DR4-DQ8 and DR4-DQ8/DR4-DQ8 genotypes (p<0.0001 vs antibody negative offspring; Fig. 3A). Children who developed GAD antibodies only (n=11) also had a higher prevalence of high risk HLA genotypes (p<0.02). In contrast, offspring who developed persistent IAA only (n=12) had remarkably similar HLA-DRB1-DQA1-DQB1 genotypes to offspring who remained autoantibody negative and control subjects. Most (7 of 9) islet autoantibody positive offspring with protective HLA-DRB1-DQA1-DQB1 genotypes had IAA only. IAA in these offspring were not maternally acquired (developed at or after age 2 years), were persistent, and were similar in titre to IAA in offspring with multiple islet autoantibodies (data not shown). INS VNTR genotypes also showed differences between antibody positive offspring (Fig. 3B). Notably, the protective INS VNTR class III/III genotype was found in 3 (27%) of 11 offspring with GAD antibodies only and in none of 51 offspring with IAA (p<0.02 GAD antibody only vs 0% in multiple or IAA only; p<0.01 vs 3.3% in autoantibody negative offspring).
Frequency of IDDM1 HLA DR-DQ genotypes (A), and IDDM2 INS VNTR genotypes (B) and combined IDDM1 HLA DR-DQ and IDDM2 INS VNTR T1D risk genotypes (C) in offspring with multiple persistent islet antibodies, in offspring with persistent GADA only, in offspring with persistent IAA only, and in islet antibody negative offspring. Offspring with persistent multiple autoantibodies (p<0.0001 vs antibody negative) or GAD autoantibodies only (p<0.02) had increased prevalences of the DR3/DR4-DQ8 and DR4-DQ8/DR4-DQ8 genotypes (A). The INS VNTR class III/III was more prevalent in offspring with GAD antibodies only (p<0.02 vs IAA positive, p<0.01 vs antibody negative) (B). Multiple autoantibody positive offspring had an increased prevalence of DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8 plus INS VNTR I/I genotypes (p<0.0001 vs autoantibody negative offspring) (C); Offspring with GAD antibodies only had an increased prevalence of DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8 plus INS VNTR I/III or III/III genotypes (p<0.005 vs antibody negative offspring)(C)
The number and target specificity of autoantibodies was influenced by the combination of IDDM1 and IDDM2 genotypes (Fig. 3C). Multiple autoantibodies were associated with both IDDM1 and IDDM2 high risk genotypes: 16 of 39 offspring with multiple autoantibodies (all IAA and GAD antibody positive) had both IDDM1 (HLA DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8) and IDDM2 (INS VNTR class I/I) high-risk genotypes (p<0.0001 versus autoantibody negative offspring). Offspring who developed autoantibodies to GAD only had an increased prevalence of high-risk IDDM1 genotypes in the absence of high-risk IDDM2 genotypes (27% versus 2.7% in autoantibody negative offspring; p<0.005). IDDM1 and IDDM2 genotypes in offspring with persistent IAA only were similar to those in the autoantibody negative offspring and showed no enrichment of the high-risk genotypes. IA-2 antibodies were only found in offspring with multiple antibodies and were associated with both high risk IDDM1 and IDDM2 genotypes.
Discussion
This study classifies T1D risk on the basis of IDDM1 and IDDM2 genotyping. It identifies and stratifies individual HLA class II genotypes conferring different risks for T1D, confirms the separate contribution of the HLA-DRB1 locus to T1D risk, and demonstrates that the IDDM2 gene confers additional risk above that of IDDM1, regardless of IDDM1 genotype. Follow-up of over 1200 offspring of parents with T1D demonstrated that early T1D-associated autoimmunity and T1D was frequent only in children who had the high-risk IDDM1 genotypes and was most frequent in children who had combinations of both high risk IDDM1 and IDDM2 genotypes.
High risk IDDM1 genotypes in Germany were similar to those of other Caucasian populations [12, 13, 14, 15, 16]. Consistent with the high T1D risk conferred by the DR3/DR4-DQ8 and DR4-DQ8/DR4-DQ8 genotypes, a markedly increased risk of developing islet autoantibodies in the first years of life was observed for DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8 offspring of parents with T1D. The marked risk in the offspring with HLA-DR4-DQ8/DR4-DQ8 (similar to that of DR3/4) is consistent with the high prevalence of this genotype found in T1D patients who had a first degree relative with T1D. A novel finding was that offspring with other DR4 containing T1D risk genotypes, but not those with DR3 containing risk genotypes had an increased likelihood of developing islet autoantibodies.
IDDM2 genotyping was done in order to determine whether its addition to IDDM1 genotyping might improve prediction of offspring who will develop T1D. The contribution of IDDM2 to T1D risk has been consistently demonstrated by others [3, 17, 18, 19]. However, it remains unclear whether risk is modified equally in subjects with different IDDM1 genotypes. Data from the Belgium diabetes registry showed that IDDM2 conferred increased risk only in subjects with moderate risk HLA DR-DQ genotypes suggesting that there was interaction between these genes and that INS VNTR typing in subjects with high-risk IDDM1 genotypes would be of limited value [20]. Our data on a larger patient and control cohort found modification of risk in subjects with the high risk and neutral HLA-DR-DQ genotypes. Risk modification was similar in all HLA DR-DQ genotypes, but numbers of patients with protective HLA genotypes and of controls with the high risk genotypes were too small to allow meaningful comparisons. We therefore cannot exclude that IDDM2 modifies risk less in subjects with very high risk IDDM1 genotypes than in subjects with moderate risk genotypes, as suggested by the Belgian data. Within subjects with the high risk IDDM1 HLA DR3/DR4-DQ8 genotype, the INS VNTR class I/III or III/III genotypes was associated with more than two-fold lower T1D risk than the class I/I genotype. Moreover, risk for T1D-associated autoantibody development in offspring was more than two-fold lower in DR3/DR4-DQ8 or DR4-DQ8/DR4-DQ8 offspring who also carried the INS VNTR class I/III or III/III genotypes compared to those who had the class I/I genotypes. Autoantibody risk in the offspring without high risk HLA genotypes was not modified by the INS VNTR genotypes. However, numbers of autoantibody offspring with non-high risk HLA risk genotypes was low and it remains to be determined whether INS VNTR can stratify risk in these offspring.
The class III allele of IDDM2 has been suggested to lower T1D risk by increasing immune tolerance to insulin and its precursors via increasing expression of the autoantigen in the thymus [21, 22]. The suggested model implies that insulin autoimmunity and therefore IAA would develop more frequently in individuals with the INS VNTR class I/I genotype than in individuals with the class I/III or III/III genotypes. Evidence in support of this was recently provided by the finding that the number of INS VNTR class I alleles was directly proportional to the prevalence of IAA at T1D onset [23]. The BABYDIAB offspring cohort provided a unique opportunity to test the hypothesis since autoantibodies were measured prospectively throughout the pre-diabetic period. This allowed assessment of genetic associations with the development of IAA per se and not just in those who subsequently develop T1D. IAA are the earliest autoantibodies that are detected in this cohort of children [5]. These are not maternally acquired antibodies and are persistent in the majority of cases [7]. Most children who develop IAA often also develop antibodies to GAD and/or IA-2 (multiple islet antibodies), and these children have the highest T1D risk. A minority of children develop GAD antibodies without ever becoming IAA positive. We therefore compared IDDM1 and IDDM2 genotypes in children with multiple islet autoantibodies (IAA and GAD antibody positive) to those with single antibodies and to islet autoantibody negative children. Children with both IAA and GAD antibodies had similar HLA and INS VNTR genotypes to patients with T1D. Multiple islet antibodies developed most frequently when offspring had both high risk IDDM1 and INS VNTR class I/I genotypes. Children with GAD antibodies but no IAA also had an increase in high risk IDDM1 genotype frequency, but in contrast to IAA positive children, had an excess of the protective INS VNTR class III/III genotype. This genotype was in 27% (3/11) of children with GAD antibodies only, but was not found in any of the 51 IAA positive children. Although the number of subjects developing GAD antibodies only was small, these data suggest that the development of IAA is prevented in the absence of INS VNTR class I alleles and are consistent with the hypothesis proposed by the other studies. The new finding that one copy of the class III INS VNTR reduces risk of disease and autoantibody development, with two copies of this allele providing a further risk reduction is also consistent with a peptide-HLA class II-T cell receptor affinity mechanism underlying the association of IDDM1/HLA with T1D and its relationship with IDDM2/INS VNTR [14, 21, 22]. Previously, it was concluded that IDDM2 was a recessive susceptibility locus or a dominant protective locus [3], but this is clearly not the case, as shown in a large family study (I.A. Eaves, B.J. Barratt, J.A. Todd, in preparation). An additional surprising finding was that the development of IAA without spreading to GAD or IA-2 antibodies was not associated with T1D risk IDDM1 genotypes. This implies that persistent IAA in isolation are unlikely to be associated with high T1D risk.
The modification of T1D risk conferred by IDDM2 to IDDM1 for developing T1D-associated autoimmunity to multiple autoantigens should improve our ability to identify at risk subjects from an early age. Several studies are under way to intensively follow, or to undertake primary prevention trials in, children at high risk for T1D [5, 6, 9, 10, 24]. Selection of children to be included into these studies is likely to be benefited by increased specificity since both intensive follow-up and primary intervention can be a burden to the family. The risk of T1D even for DR3/DR4-DQ8-positive children can be substantially reduced by possession of one or two INS VNTR class III alleles, and it is anticipated that protective alleles at other disease loci will soon be identified, such as CTLA4 (J.A. Todd, unpublished). It is, therefore, conceivable that a combination of protective alleles of non-MHC loci in certain individuals could reduce the T1D risk of the HLA-DR3/DR4-DQ8 genotype to 1, thereby providing a case for their exclusion from a clinical trial. By combining family history of T1D, IDDM1 and IDDM2 genotyping we were able to identify a cohort of children who had an 8.7% likelihood of developing T1D already by the age of 6 years and 21% risk for developing persistent islet autoimmunity to multiple T1D autoantigens already by the age of 2 years. This represents a high risk group that might be targeted in primary intervention trials when suitable candidate intervention therapies become available.
Abbreviations
- Abs:
-
antibodies
- dNTP:
-
desoxynucleotide triphosphate
- IAA:
-
insulin autoantibodies
- INS :
-
insulin gene
- OR:
-
odds ratio
- T1D:
-
Type 1 diabetes
- VNTR :
-
variable number of tandem repeat
References
Cox NJ, Wapelhorst B, Morrison VA et al. (2001) Seven regions of the genome show evidence of linkage to Type 1 diabetes in a consensus analysis of 767 multiplex families. Am J Hum Genet69:820–830
Redondo MJ, Eisenbarth GS (2002) Genetic control of autoimmunity in Type I diabetes and associated disorders. Diabetologia 45:605–622
Bennett ST, Lucassen AM, Gough SC et al. (1995) Susceptibility to human type 1 diabetes atIDDM2 is determined by tandem repeat variation at the insulin gene minisatellite locus. Nat Genet 9:284–292
Cordell HJ, Todd JA, Bennett ST, Kawaguchi Y, Farrall M (1995) Two-locus maximum lod score analysis of a multifactorial trait: joint consideration ofIDDM2 and IDDM4 with IDDM1 in type 1 diabetes. Am J Hum Genet 57:920–934
Ziegler AG, Hummel M, Schenker M, Bonifacio E (1999) Autoantibody appearance and risk for development of childhood diabetes in offspring of parents with type 1 diabetes: the 2-year analysis of the German BABYDIAB Study. Diabetes 48:460–468
Yu L, Robles DT, Abiru N et al. (2000) Early expression of antiinsulin autoantibodies of humans and the NOD mouse: evidence for early determination of subsequent diabetes. Proc Natl Acad Sci USA 97:1701–1706
Naserke HE, Bonifacio E, Ziegler AG (2001) Prevalence, characteristics and diabetes risk associated with transient maternally acquired islet antibodies and persistent islet antibodies in offspring of parents with type 1 diabetes. J Clin Endocrinol Metab86:4826–4833
Schenker M, Hummel M, Ferber K et al. (1999) Early expression and high prevalence of islet autoantibodies for DR3/4 heterozygous and DR4/4 homozygous offspring of parents with Type I diabetes: The German BABYDIAB study. Diabetologia 42:671–677
Yu J, Yu L, Bugawan TL et al. (2000) Transient antiislet autoantibodies: infrequent occurence and lack of association with "genetic" risk factors. J Clin Endocrinol Metab 85:2421–2428
Kupila A, Keskinen P, Simell T et al. (2002) Genetic risk determines the emergence of diabetes-associated autoantibodies in young children. Diabetes 51:646–651
Bingley PJ, Bonifacio E, Mueller P and participating laboratories (2001) Diabetes antibody standardisation programme: first assay proficiency evaluation Diabetologia 44 [Suppl. 1]:A 74 (Abstract)
Zavattari P, Lampis R, Motzo C et al. (2001) Conditional linkage disequilibrium analysis of a complex disease superlocus,IDDM1 in the HLA region, reveals the presence of independent modifying gene effects influencing the type 1 diabetes risk encoded by the major HLA-DQB1, -DRB1 disease loci. Hum Mol Genet10:881–889
Buyse I, Sandkuyl LA, Zamani Ghabanbasani M et al. (1994) Association of particular HLA class II alleles, haplotypes and genotypes with susceptibility to IDDMin the Belgian population. Diabetologia 37:808–817
Baisch JM, Weeks T, Giles R, Hoover M, Stastny P, Capra JD (1990) Analysis of HLA-DQ genotypes and susceptibility in insulin-dependent diabetes mellitus. The N Engl J Med 322:1836–1841
Caillat-Zucman S, Djilali-Saiah I, Timsit J et al. (1997) Insulin dependent diabetes mellitus (IDDM): 12th International Histocompatibility Workshop study. In: Charron D (ed.) HLA. Proceedings of the Twelfth Histocompatibility Workshop and Conference, vol 2. EDK, Paris, pp 389 –398
Cucca F, Congia M, Angius E et al. (2001) A correlation between the relative predisposition of MHC class II alleles to type 1 diabetes and the structure of their proteins. Hum Mol Genet 10:2025–2037
Bell GI, Horita S, Karam JH (1984) A polymorphic locus near the human insulin gene is associated with insulin-dependent diabetes mellitus. Diabetes33:176–183
Chowdhury TA, Mijovic CH, Barnett AH (1999) The aetiology of Type I diabetes. Best Pract Res Clin Endocrinol Metab 13:181–195
Awata T, Kurihara S, Kikuchi C et al. (1997) Evidence for association between the class I subset of theinsulin gene minisatellite (IDDM2 locus) and IDDMin the Japanese population. Diabetes 46:1637–1642
Auwera B van der, Schuit F, Lyaruu I et al. (1995) Genetic susceptibility for insulin-dependent diabetes mellitus in Caucasians revisited: the importance of diabetes registries in disclosing interactions between HLA-DQ- andinsulin gene-linked risk. Belgian Diabetes Registry. J Clin Endocrinol Metab 80:2564–2565
Pugliese A, Zeller M, Fernandez A Jr et al. (1997) The insulin gene is transcribed in the human thymus and transcription levels correlated with allelic variation at theINS VNTR-IDDM2 susceptibility locus for type 1 diabetes. Nat Genet 15:293–297
Vafiadis P, Bennett ST, Todd JA et al. (1997) Insulin expression in human thymus is modulated byINS VNTR alleles at the IDDM2 locus. Nat Genet 15:289–292
Graham J, Hagopian WA, Kockum I et al. (2002) Genetic effects on age-dependent onset and islet cell autoantibody markers in Type 1 diabetes. Diabetes 51:1346–1355
Colman P, Steele C, Couper JJ et al. (2000) Islet autoimmunity in infants with a Type I diabetic relative is common but is frequently restricted to one autoantibody. Diabetologia43:203–209
Acknowledgements
This study was supported by grants from the Juvenile Diabetes Research Foundation (JDRF #1-2000-619, 061858), the Wellcome Trust (061858), the Stiftung 'Das Zuckerkranke Kind', and the Deutsche Diabetesgesellschaft (Dr. Buding-Stiftung). We thank A. Knopff, J. Vordemann, I. Zöbisch and E. Kleinschmidt for data collection and expert technical assistance, and H. Cordell for advice in statistical analyses. We also thank the pediatricians and family doctors in Germany for participation in the BABYDIAB study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, M., Albert, E., Conrad, M. et al. IDDM2/insulin VNTR modifies risk conferred by IDDM1/HLA for development of Type 1 diabetes and associated autoimmunity. Diabetologia 46, 712–720 (2003). https://doi.org/10.1007/s00125-003-1082-z
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-003-1082-z