Abstract
Purpose
Vital signs are important for predicting clinical outcomes in patients with trauma. However, their accuracy can be affected in older adults because hemodynamic changes are less obvious. This study aimed to examine the usefulness of changes in vital signs during transportation in predicting the need for hemostatic treatments in older patients with trauma.
Methods
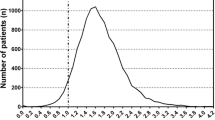
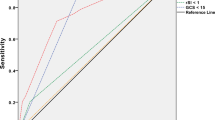
This retrospective cohort study was conducted using data from the Japan Trauma Data Bank (2004–2019). Patients aged ≥ 65 years who were hemodynamically stable at the scene were included in this study. The incidence of emergency surgery within 12 h after hospital arrival was compared between patients with delta Shock Index (dSI) > 0.1 and those with dSI ≤ 0.1. Predicting ability was examined after adjusting for patient demographics, comorbidities, vital signs at the scene and on hospital arrival, Injury Severity Score, and abbreviated injury scale in each region.
Results
Among the 139,242 patients eligible for the study, 3,701 underwent urgent hemostatic surgery within 12 h. Patients with dSI > 0.1 showed a significantly higher incidence of emergency surgery than those with dSI ≤ 0.1 (871/16,549 [5.3%] vs. 2,830/84,250 [3.4%]; odds ratio (OR), 1.60 [1.48–1.73]; adjusted OR, 1.22 [1.08–1.38]; p = 0.001). The relationship between high dSI and a higher incidence of intervention was observed in patients with hypertension and those with decreased consciousness on arrival.
Conclusion
High dSI > 0.1 was significantly associated with a higher incidence of urgent hemostatic surgery in older patients.

Similar content being viewed by others
Data availability
The data used in this study are available from the Japanese Association for Trauma Surgery and the Japanese Association for Acute Medicine, but restrictions apply to the availability of these data, which were used under license for the current study, so these data are not publicly available. The data are available from the authors upon reasonable request and with permission of the Japanese Association for Trauma Surgery and the Japanese Association for Acute Medicine.
References
Muramatsu N, Akiyama H. Japan: super-aging society preparing for the future. Gerontologist. 2011;51:425–32. https://doi.org/10.1093/geront/gnr067.
Tsuchiya Y, Shida N, Tsujiuchi T, Machida K. Healthy aging and concerns among elderly Japanese: a text analysis approach. Int Q Community Health Educ. 2015;35:215–26. https://doi.org/10.1177/0272684x15576515.
Martino C, Russo E, Santonastaso DP, Gamberini E, Bertoni S, Padovani E, et al. Long-term outcomes in major trauma patients and correlations with the acute phase. World J Emerg Surg. 2020;15:6. https://doi.org/10.1186/s13017-020-0289-3.
Jacoby SF, Ackerson TH, Richmond TS. Outcome from serious injury in older adults. J Nurs Scholarsh. 2006;38:133–40. https://doi.org/10.1111/j.1547-5069.2006.00090.x.
Boss GR, Seegmiller JE. Age-related physiological changes and their clinical significance. West J Med. 1981;135:434–40.
Baker SP, O’Neill B, Haddon W Jr., Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma score. J Trauma. 1989;29:623–9. https://doi.org/10.1097/00005373-198905000-00017.
Yousefzadeh CS, Ranjbar TF, Malekpouri R, Razzaghi A. Predicting mortality, hospital length of stay and need for surgery in pediatric trauma patients. Chin J Traumatol. 2017;20:339–42. https://doi.org/10.1016/j.cjtee.2017.04.011.
Koch E, Lovett S, Nghiem T, Riggs RA, Rech MA. Shock index in the emergency department: utility and limitations. Open Access Emerg Med. 2019;11:179–99. https://doi.org/10.2147/oaem.S178358.
Rau CS, Wu SC, Kuo SC, Pao-Jen K, Shiun-Yuan H, Chen YC, et al. Prediction of massive transfusion in trauma patients with shock index, modified shock index, and age shock index. Int J Environ Res Public Health. 2016;13. https://doi.org/10.3390/ijerph13070683.
Burstow M, Civil I, Hsee L. Trauma in the elderly: demographic trends (1995–2014) in a major New Zealand Trauma Centre. World J Surg. 2019;43:466–75. https://doi.org/10.1007/s00268-018-4794-4.
Mador B, Nascimento B, Hollands S, Rizoli S. Blood transfusion and coagulopathy in geriatric trauma patients. Scand J Trauma Resusc Emerg Med. 2017;25:33. https://doi.org/10.1186/s13049-017-0374-0.
Heffernan DS, Thakkar RK, Monaghan SF, Ravindran R, Adams CA Jr., Kozloff MS, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69:813–20. https://doi.org/10.1097/TA.0b013e3181f41af8.
Joseph B, Haider A, Ibraheem K, Kulvatunyou N, Tang A, Azim A, et al. Revitalizing vital signs: the role of delta shock index. Shock. 2016;46:50–4. https://doi.org/10.1097/shk.0000000000000618.
Kim DK, Jeong J, Shin SD, Song KJ, Hong KJ, Ro YS, et al. Association between prehospital field to emergency department delta shock index and in-hospital mortality in patients with torso and extremity trauma: a multinational, observational study. PLoS ONE. 2021;16:e0258811. https://doi.org/10.1371/journal.pone.0258811.
Yamamoto R, Suzuki M, Yoshizawa J, Nishida Y, Junichi S. Physician-staffed ambulance and increased in-hospital mortality of hypotensive trauma patients following prolonged prehospital stay: a nationwide study. J Trauma Acute Care Surg. 2021;91:336–43. https://doi.org/10.1097/ta.0000000000003239.
Grant SW, Hickey GL, Head SJ. Statistical primer: multivariable regression considerations and pitfalls. Eur J Cardiothorac Surg. 2019;55:179–85. https://doi.org/10.1093/ejcts/ezy403.
Ostir GV, Uchida T. Logistic regression: a nontechnical review. Am J Phys Med Rehabil. 2000;79:565–72. https://doi.org/10.1097/00002060-200011000-00017.
Wu SC, Rau CS, Kuo SCH, Hsu SY, Hsieh HY, Hsieh CH. Shock index increase from the field to the emergency room is associated with higher odds of massive transfusion in trauma patients with stable blood pressure: a cross-sectional analysis. PLoS ONE. 2019;14:e0216153. https://doi.org/10.1371/journal.pone.0216153.
Yamamoto R, Fujishima S, Sasaki J. Nasal intubation for trauma patients and increased in-hospital mortality. Eur J Trauma Emerg Surg. 2022;48:2795–802. https://doi.org/10.1007/s00068-022-01880-8.
Paneni F, Diaz CC, Libby P, Lüscher TF, Camici GG. The aging cardiovascular system: understanding it at the cellular and clinical levels. J Am Coll Cardiol. 2017;69:1952–67. https://doi.org/10.1016/j.jacc.2017.01.064.
Pandit V, Rhee P, Hashmi A, Kulvatunyou N, Tang A, Khalil M, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:1111–5. https://doi.org/10.1097/ta.0000000000000160.
Martin JT, Alkhoury F, O’Connor JA, Kyriakides TC, Bonadies JA. Normal’ vital signs belie occult hypoperfusion in geriatric trauma patients. Am Surg. 2010;76:65–9.
Jacobs DG, Plaisier BR, Barie PS, Hammond JS, Holevar MR, Sinclair KE, et al. Practice management guidelines for geriatric trauma: the EAST Practice Management guidelines Work Group. J Trauma. 2003;54:391–416. https://doi.org/10.1097/01.Ta.0000042015.54022.Be.
Viazzi F, Russo E, Mirijello A, Fioretto P, Giorda C, Ceriello A, et al. Long-term blood pressure variability, incidence of hypertension and changes in renal function in type 2 diabetes. J Hypertens. 2020;38:2279–86. https://doi.org/10.1097/hjh.0000000000002543.
Li CL, Liu R, Wang JR, Yang J. Relationship between blood pressure variability and target organ damage in elderly patients. Eur Rev Med Pharmacol Sci. 2017;21:5451–5. https://doi.org/10.26355/eurrev_201712_13934.
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
SF and RY designed the study. SF, JS, YT, and RK performed data collection. JS contributed to quality control. SF, RY, KH, and JY performed data analysis, data interpretation, writing, and critical revision. All authors critically revised the manuscript and approved the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the IRB of Keio University School of Medicine. All the procedures were conducted in accordance with the tenets of the Declaration of Helsinki. The requirement for informed consent was waived due to the retrospective nature of the study.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Funabiki, S., Yamamoto, R., Homma, K. et al. Delta Shock Index and higher incidence of emergency surgery in older adults with blunt trauma. Eur J Trauma Emerg Surg 50, 561–566 (2024). https://doi.org/10.1007/s00068-023-02438-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02438-y