Abstract
Purpose
Direct Discharge protocols (DD) can alleviate strain on healthcare systems by reducing routine outpatient follow-up. These protocols include low-complex musculoskeletal injuries, such as isolated greenstick fractures or torus fractures of the wrist in children. While there is consensus on the effectiveness of DD, there is a lack of injury-specific powered studies. This study compares treatment satisfaction between DD and traditional treatment in children with a greenstick fracture or torus fractures of the wrist.
Methods
Children with isolated torus or greenstick fractures of the distal radius or ulna were eligible for inclusion before (pre-DD cohort) and after (DD cohort) the implementation of DD in four hospitals. Traditionally, patients receive a (soft) cast and minimally one routine outpatient follow-up appointment. With DD, patients are discharged directly from the ED after receiving a brace and information, summarized in a smartphone app and a helpline for questions during recovery. The primary outcome was patient or proxy treatment satisfaction (0 to 10), and a power analysis was performed to assess non-inferiority. Secondary outcomes included complications, functional outcomes measured in Patient-Reported Outcomes Measurement Information System Upper Extremity (PROMIS UE), primary healthcare utilisation, and secondary healthcare utilisation (follow-up appointments and imaging).
Results
In total, 274 consecutive children were included to analyse the primary endpoint. Of these, 160 (58%) were male with a median age of 11 years (IQR 8 to 12). Pre-DD and DD treatment satisfaction did not vary statistically significantly for greenstick fractures (p = 0.09) and torus fractures (p = 0.93). No complications were observed. PROMIS UE showed no statistically significant differences before and after implementation of direct discharge protocol for torus (p = 0.99) or greenstick (p = 0.45) fractures. Secondary healthcare utilisation regarding follow-up was significantly lower in the DD-torus cohort compared to the pre-DD torus cohort, with a mean difference (MD) of − 1.00 follow-up appointments (95% Confidence Interval (CI) − 0.92 to − 1.13). Similar results were found in the pre DD-greenstick cohort compared to the pre-DD-greenstick cohort (MD): − 1.17 follow-up appointments, 95% CI − 1.09 to − 1.26).
Conclusion
Direct Discharge is non-inferior to traditional treatment in terms of treatment satisfaction for paediatric patients with greenstick or torus fractures of the wrist compared to children treated with rigid immobilisation and routine follow-up. Furthermore, the results demonstrate no complications, comparable functional outcomes, and a statistically significant reduction of secondary healthcare utilisation, making DD a good solution to cope with strained resources for children with an isolated greenstick fracture or torus fracture of the wrist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the wrist are among the most common injuries in paediatric patients, of which over 40% are low-complex, minor injuries [1]. Isolated torus and greenstick fractures without substantial displacement recover quickly and are most often treated with a cast [2, 3]. Low-complex paediatric wrist fractures, such as torus fractures or isolated greenstick fractures of the radius or ulna, have increasingly been managed through Direct Discharge protocols (DD) and Virtual Fracture Clinics (VFC) [4,5,6,7]. In its Dutch adaptation, DD involves discharging patients directly from the Emergency Department (ED) without routine follow-up, providing them with a removable orthosis or sling, and information through a mobile self-care application called the Virtual Fracture Care application (VFC app). Evidence supports DD’s overall safety and effectiveness as an alternative to traditional treatment protocols while reducing the need for secondary healthcare utilisation, resulting in comparable patient-reported outcomes (e.g. functional outcome and satisfaction scores) and little to no adverse outcomes (e.g. complications and persistent complaints) [7,8,9]. This method has gained popularity in the Netherlands, catalysed by the COVID-19 pandemic, and is currently standard care in over 30 of 80 Dutch hospitals. Although current evidence proves that the DD concept is satisfactory and safe, powered injury-specific results are lacking. Consequently, the optimal follow-up frequency for specific types of injuries remains unclear.
Therefore, the aim of this study was to determine whether treatment with a Direct Discharge protocol resulted in non-inferior child- and parental satisfaction in children with an isolated greenstick fracture or torus fracture of the wrist, compared to children treated with rigid immobilisation and routine follow-up.
Methods
Design
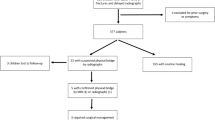
This multicentre, prospective observational cohort study took place in four Dutch level 2 trauma teaching hospitals from the 1st of December 2021 to the 31st of August 2022, alongside the implementation of DD. Eligible patients had isolated torus or greenstick fractures of the distal radius or ulna with acceptable angulation according to the Dutch guideline based on age-related residual growth (Fig. 1) [10]. Furthermore, eligible patients had isolated injuries, low-energy trauma, Glasgow Coma Scale over 14, and spoke Dutch or English fluently. The study comprised two cohorts, a pre-DD cohort and a DD cohort, divided by the hospital implementation date. No comorbidity or cognitive impairment restrictions were applied. However, patients were excluded if healthcare professionals deemed DD unsuitable (e.g., social care reasons or language barrier) or if they received initial treatment in another hospital or requested follow-up in a hospital close to home.
Pre-DD (traditional treatment)
Before DD, patients were treated according to local trauma protocols, which varied between hospitals but often involved (soft) cast immobilisation for two to four weeks and verbal injury-related information at the ED. At least one outpatient follow-up appointment was scheduled for review, detailed information, and definitive management within 2 weeks after the injury.
Direct discharge protocol
Derived from the British Virtual Fracture Clinic (VFC) model, DD included 12 treatment protocols for low-complex musculoskeletal injuries, including greenstick- and torus fractures of the distal radius or ulna [10]. With DD, patients were discharged directly from the ED without routine follow-up. They received a removable orthosis instead of a cast and verbal information at the ED, which is summarised in a mobile self-care application, the VFC app. During the review of all ED cases the next working day, eligibility for DD was verified by an orthopaedic or trauma surgeon and radiologist. DD varies from traditional treatment in (1) the mode of routine outpatient follow-up (changing from physical to none, (2) the immobilisation (changing from a (soft) cast to removable orthosis), and (3) the delivery of uniform information (changing from verbal to digital).
Outcomes
Satisfaction
The primary outcome of this study was satisfaction on a scale ranging from 0 to 100, 0 meaning very dissatisfied, to 100, meaning very satisfied, at three months after injury. Satisfaction was assessed in the three domains that change most with DD: overall treatment, immobilisation, and recovery information with patients or proxies (if patients were below the age of 12 years). All scores were rounded to numbers from one to ten to improve readability. The minimal clinically important difference (MCID) was set at 1.0 on a ten-point scale [6]. Treatment preferences were reported as face-to-face, neutral, or an application (such as the VFC app).
Immobilisation related outcomes
Immobilisation-related outcomes included ‘complications,’ ‘functional outcomes,’ and ‘analgesic use.’ Complications were evaluated by complication rate and type. Functional outcomes were measured with the Patient Reported Outcomes Measurement Information System for Upper Extremity (PROMIS UE) [7]. Currently, no musculoskeletal Patient Reported Outcome Measures are validated for children. To provide a holistic perspective of functional outcomes, relevant parameters of the CORE-kids outcomes have been used to provide additional data, including return to manual dexterity, return to sports, and return to activities of daily living (ADL) [11]. These were measured in four-point Likert scales ranging from 1, meaning complete return, to 4, no return at all. Additionally, analgesic use was measured in binary (yes/no), and by the type of analgesic used, including injury-site cooling, acetaminophen, and non-steroid anti-inflammatory drugs (NSAID). The timing of analgesic use was measured binary per week during the first four weeks (yes/no).
Healthcare utilisation
Healthcare utilisation was evaluated by ‘primary healthcare utilisation’ and ‘secondary healthcare utilisation’. Primary healthcare utilisation was evaluated by the number-, and frequency of injury-related follow-up appointments with a general practitioner or physiotherapist after the ED visit. Secondary healthcare utilisation was assessed based on the frequency of injury-related follow-up appointments and imaging procedures, including radiographs, computed tomography (CT), and magnetic resonance imaging (MRI).
VFC app use
VFC app use was evaluated by the frequency of use during the first 3 months of recovery as reported by patients or proxies.
Recruitment and consent
After consent at the ED, eligible children or proxies were contacted by phone 3 months post-injury for a short survey, and an opt-out form was sent. Satisfaction scores, functional outcomes, and primary healthcare utilisation were collected, coded, and data were stored in an online database using RedCap [8]. The Electronic Patient Record was used to collect secondary healthcare utilisation and demographic data (age in years and sex) at least 3 months post-injury.
Statistical analysis
Statistical analysis was performed using SPSS version 26.0.0.2 (IBM Corporation, Armonk, NY, United States) [12]. Normal distribution of continuous data was assessed with visual analysis of histograms, Kolmogorov and Shapiro–Wilk tests. Discrete variables were reported as numbers (percentages of the total population). The Chi-square test was used to determine the statistical significance of categorical variables. The Mann–Whitney U test was used to determine the statistical significance of non-parametric independent data. All reported p-values were 2-sided and considered statistically significant if they were lower than 0.05.
Power analysis
The primary outcome was treatment satisfaction at 3 months post-injury. This study aimed to demonstrate non-inferiority in satisfaction with traditional treatment compared to DD. A calculation was made based on the average satisfaction of 7.95 (standard deviation (SD) 1.7) on a 10-point scale in the pilot study [9]. Assuming a Minimal Clinically Important Difference (MCID) of 1.0 points on a 10-point scale, 90% power, one-sided α = 0.025, and an SD of 1.7, 124 patients (62 per arm) were required to show non-inferiority [6]. Allowing for a 10% loss to follow-up during the inclusion period, the minimum sample size was set at 136 per injury. This resulted in a total of 68 patients per injury per treatment type.
Patient and public involvement
Patients were not involved in the design, intervention, research question, or outcome measures of this study.
Ethics
The study was conducted under the Declaration of Helsinki and was approved by the local medical ethical review board Utrecht (W21.261). The institutions of the authors affiliated with St. Antonius Hospital and OLVG Hospital have received funding for support of this work by an unrestricted grant from the Dutch Organization for healthcare sciences and healthcare innovation, ZonMw, The Hague, The Netherlands, grant number: 516012524. None of the authors have a conflict of interest to declare for the execution of this study. Studydata is accessible upon request.
Results
Demographics
Between the 1st of December 2021 and the 31st of August 2022, 457 patients were screened. Of those, 267 (58%) were male. A total of 221 patients were treated with traditional treatment, of which 130 sustained a torus fracture and 91 a greenstick fracture. Treatment with DD was given to 236 patients, of whom 138 sustained a torus fracture and 98 a greenstick fracture. Study follow-up was completed on the 30th of November 2022, with collected primary outcomes of at least 68 patients per treatment group and a total of 274 patients. Baseline demographics were similar in both treatment groups (Table 1). During the recruitment period, over 1.4 times as many children presented to the ED with a torus fracture compared to a greenstick fracture in both the pre-DD cohort (130/91) and the DD cohort (138/98).
Satisfaction
No statistically significant differences in treatment satisfaction were found between the pre-DD cohort (median 8.0, IQR 7.5 to 8.5) and the DD cohort for torus fractures (median 8.0, IQR 7.6 to 8.5) (p = 0.93). The same applied to pre-DD (median 8.0, IQR 8.0 to 8.5) and DD patients (median 8.0 IQR 7.9 to 8.0) (p = 0.09) with a greenstick fracture. Similar scores were observed for satisfaction with immobilisation for torus fractures pre-DD (median 8.0, IQR 8.0 to 8.5) and with DD (median 8.0, IQR 7.5 to 9.0) (p = 0.89), and greenstick fractures pre-DD (median 8.0, 8.0 to 8.8) and with DD (median 8.0 to 8.1) (p = 0.39), and satisfaction concerning information during recovery for torus fractures pre-DD (8.0, IQR 8.0 to 9.0) and with DD (8.0, IQR 8.0 to 9.0) (p = 0.79) and greenstick fractures pre-DD (median 8.0, IQR 8.0 to 9.0) and with DD (median 8.0, IQR 8.0 to 8.5) (p = 0.23) (Fig. 2). Among included patients and proxies in the pre-DD cohort, 89 (65%) preferred an application (such as the VFC app), 42 (31%) preferred face-to-face follow-up, and 5 (4%) had no preference.
Immobilisation related outcomes
Complications
Patients who sustained a torus fracture in the pre-DD and DD cohort reported no complications. In the pre-DD cohort of patients with a greenstick fracture, 2/68 (3%) reported persistent pain three months after injury. Both patients were scheduled for an outpatient follow-up. After reassurance and information, no interventions were required. One patient (1/70, 1%) with a greenstick in the DD cohort reported skin irritation due to the removable orthosis. This patient switched from a removable orthosis to a soft cast to support the fracture, after which follow-up was completed.
Functional outcomes
PROMIS UE scored at 3 months post-injury did not differ significantly between pre-DD and DD patients in the torus-cohort (p = 0.99), and the greenstick cohort (p = 0.65) with a median score of 8.0 (IQR 8.0 to 8.0) in all groups (Table 2). Almost all patients with a torus fracture in the pre-DD group had a full return to previous manual dexterity, sports, and ADL, except one (1/68, 1%) who was somewhat limited in all three. In the DD group, all patients with a torus fracture had a full return to previous manual dexterity, sports, and one (1/68, 1%) was somewhat limited in return to ADL. All patients with greenstick fractures in the pre-DD group had a full return to previous manual dexterity. In the DD group, all patients had a full return of function, except two (2/68, 3%) who were somewhat limited in return to sports and one (1/68, 1%) who was somewhat limited in return to ADL (Table 2).
Analgesic use
Analgesic use was high in the first week post-injury in all four groups and declined rapidly in the second week. Most pre-DD torus patients used analgesics (42/68, 62%), mostly acetaminophen (39/42, 93%), and some NSAIDs (2/42, 3%) or cooling (1/42, 1%). Most DD torus patients (52/68, 76%) used analgesics, all using acetaminophen. A similar number of pre-DD greenstick fracture patients (43/68, 63%) used analgesics, all using acetaminophen and one combining this with NSAIDs. Most DD greenstick patients 45/70 (64%) used analgesics, with 44/45 (98%) using acetaminophen and one using NSAIDs (Table 2).
Healthcare utilisation
Primary healthcare utilisation
In the pre-DD and DD cohort, four patients with a torus fracture utilised primary healthcare. Four patients with a greenstick fracture in the pre-DD cohort used primary healthcare during recovery, and six patients in the DD cohort, of which two patients visited both the physiotherapist and general practitioner (Table 3).
Secondary healthcare utilisation
The mean number of secondary healthcare appointments in the pre-DD cohort of torus fractures was 1.16 (SD 0.54) versus 0.16 (SD 0.47) in the DD cohort, resulting in a mean difference (MD) of 1.00 (95% CI 0.92 to 1.13). The mean number of secondary healthcare appointments in the pre-DD cohort of patients with a greenstick fracture was 1.34 (SD 0.64) versus 0.17 (0.39) in the DD cohort, with an MD of 1.17 (95% CI 1.09 to 1.26). Imaging was comparable and low in all four groups (Table 3).
VFC app use
The mean frequency of application use during recovery was 2.1 (SD 2.2) times during recovery in patients with a torus fracture and 1.5 (SD 2.3) times during recovery in patients with a greenstick fracture.
Discussion
Results of this prospective multicentre cohort study showed that DD is non-inferior in terms of satisfaction regarding overall treatment, immobilisation, and information during the recovery process compared to traditional treatment for patients with torus fracture or an isolated greenstick fracture of the distal forearm, compared to patients treated with rigid immobilisation and routine follow-up.
The satisfaction results of this study are in line with the current literature. In previous underpowered studies with cohorts comparable to the pre-DD and DD cohort, treatment and immobilisation satisfaction levels were similarly high [13,14,15]. Comparable to other studies, a removable orthosis with immediate discharge was preferred over a cast with routine follow-up [3, 14]. One study reported the preference for a cast on day one post-injury due to pain [3]. However, this preference was not observed in the study at 6 weeks or after, showing no differences in satisfaction scores or pain scores for both treatment methods. Furthermore, in this study, high levels of perceived safety and the preference for DD and a self-care application, such as the VFC app, over face-to-face follow-up for patients with torus- or greenstick fractures of the wrist were mentioned. These parameters have been reported in eHealth evaluation studies but are a novelty in DD and VFCs [16].
Similar to the literature, a low amount of complications and good functional outcomes were detected in both cohorts for both injuries individually, indicating comparable results between traditional treatment and DD [3, 9]. Both PROMIS UE and the parameters of the CORE kids score, were comparably high, indicating good functional outcomes of these injuries at three months follow-up. Analgesic use was comparable to previous studies, showing high levels of analgesic use in the first week, followed by a rapid decline showing limited analgesic requirement throughout recovery, further strengthening the limited need for analgesics for these injuries and immobilisation types [3]. The treatment of torus fractures with less rigid immobilisation than a cast is supported by current literature, as these are widely regarded as stable, self-limiting fractures [3, 13, 14, 17]. This has been less evident for greenstick fractures, with study results reporting further displacement during the first 14 days after manually realigned greenstick fractures [17]. However, this secondary displacement never resulted in a change in fracture management, and this study excluded realigned fractures [17]. The lack of surgical intervention might be explained by the excellent remodelling capacities of distal epiphysis of the radius, which is the most active epiphysis in the growing child [18].
Based on the low complications, good functional outcome, and satisfactory results with immobilisation, we believe treatment with DD is safe. The statistically significant reductions in secondary healthcare utilisation were consistent with previous research and estimations [5, 19,20,21]. This shows that treatment of both fracture types can safely be reduced to one ED visit without negatively influencing satisfaction. The findings could make treatment strategies for greenstick fractures more uniform between hospitals regarding follow-up and immobilisation materials whilst reducing secondary healthcare utilisation.
This study has several strengths. First, the comprehensive outcomes provided a holistic perspective of patient satisfaction, functional outcome and treatment safety. Second, the study was adequately powered to detect an MCID in satisfaction with a representable study population. Third, the pragmatic pre-post multicentre design alongside the implementation of DD provided a cheap, effective, and quick alternative to often time-consuming and often expensive RCTs with an acceptable level of evidence. This study also has limitations. Only patients who responded to the phone call were included in the study, potentially leading to selection bias. Furthermore, the timing of functional outcome at 3 months follow-up might have been suboptimal to measure functional outcome, as almost all patients had fully recovered by then. Nevertheless, all scores were high with both protocols.
The outcomes of this study, along with previously published studies, can be used to support the implementation of DD as the new standard of care for specific injuries, which could support the reduction of secondary healthcare utilisation whilst maintaining non-inferior treatment satisfaction. Furthermore, DD reduces the heterogeneity in treatment of these low-complex injuries [22]. The study design used can be applied to rapidly and comprehensively assess differences between treatment options without hindering implementation in interested hospitals. A central registry with uniform parameters could be considered to improve DD further and potentially include new injuries in the protocol. Future studies should focus on the optimal timing to measure functional outcomes in paediatric patients and the validation of PROMs in children. Our future efforts will be focused on developing similar protocols for other and also more complex injuries to alleviate the burden on healthcare systems already under strain.
To conclude, the results of this multicentre cohort study on children with a greenstick fracture or torus fractures of the wrist. showed that Direct Discharge is non-inferior in terms of satisfaction with treatment, satisfaction with immobilisation, and satisfaction with information during the recovery process compared to traditional treatment. These results could help de-medicalise these injuries and prevent the overuse of healthcare resources for these common fractures.
Data availability
Studydata is accessible upon request.
References
Korup LR, et al. Children’s distal forearm fractures: a population-based epidemiology study of 4316 fractures. Bone Jt Open. 2022;3:448.
Handoll HHG, Elliott J, Iheozor-Ejiofor Z, Hunter J, Karantana A. Interventions for treating wrist fractures in children. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD012470.pub2.
Perry DC et al. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022;400(10345):39–47.
Fuschini C, et al. Validation of the primary care pathway model for management of orthopedic injuries: results of a prospective, Queensland study. J Prim Care Community Heal. 2020. https://doi.org/10.1177/2150132720967228.
Geerdink TH, et al. Healthcare utilization and satisfaction with treatment before and after direct discharge from the Emergency Department of simple stable musculoskeletal injuries in the Netherlands. Eur J Trauma Emerg Surg. 2022;48:2135–44.
Logishetty K. Adopting and sustaining a virtual fracture clinic model in the district hospital setting – a quality improvement approach. BMJ Qual Improv Reports. 2017. https://doi.org/10.1136/bmjquality.u220211.w7861.
Vardy J, et al. Effect of a redesigned fracture management pathway and ‘virtual’ fracture clinic on ED performance. BMJ Open. 2014. https://doi.org/10.1136/bmjopen-2014-005282.
Geerdink TH, Haverlag R, van Veen RN, Bouwmeester OVA, Goslings JC. Direct discharge from the ED for patients with simple stable injuries: a Dutch pilot study. Ned Tijdschr Geneeskd. 2020;164:D4604.
Geerdink TH, et al. Direct discharge of patients with simple stable musculoskeletal injuries as an alternative to routine follow-up: a systematic review of the current literature. Eur J Trauma Emerg Surg. 2022;48:2589–605.
Federation of Medical Specialist, Dutch Guideline of Pediatric Fractures. (2019). Available at: https://richtlijnendatabase.nl/richtlijn/fracturen_bij_kinderen/polsfracturen/behandeling_polsfracturen.html.Accessed 26 May 2023.
Marson BA, et al. Development of the CORE-Kids core set of outcome domains for studies of childhood limb fractures. Bone Jt J. 2021;103:1821–30.
IBM. IBM Corp. Released 2020. IBM SPSS statistics for windows, Version 27.0. (2020)
Solan MC, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury. 2002;33:503–5.
Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ. 2010;182:1507–12.
Boutis K, et al. A randomized, controlled trial of a removable brace versus casting in children with low-risk ankle fractures. Pediatrics. 2007;119:e1256.
Enam A, Torres-Bonilla J, Eriksson H. Evidence-based evaluation of ehealth interventions: systematic literature review. J Med Internet Res. 2018;20:e10971.
Randsborg PH, Sivertsen EA. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthop. 2009;80:585–9.
Pritchett JW. Growth plate activity in the upper extremity. Clin Orthop Relat Res. 1991;1:235.
Ting BL, Kalish LA, Waters PM, Bae DS. Reducing cost and radiation exposure during the treatment of pediatric greenstick fractures of the forearm. J Pediatr Orthop. 2016;36:816–20.
Hamilton TW, et al. The treatment of stable paediatric forearm fractures using a cast that may be removed at home: comparison with traditional management in a randomised controlled trial. Bone Jt J. 2013;95B:1714.
Khan SA, Asokan A, Handford C, Logan P, Moores T. How useful are virtual fracture clinics? Bone Jt Open. 2020. https://doi.org/10.1302/2633-1462.111.bjo-2020-0107.r1.
Geerdink TH, et al. Adoption of direct discharge of simple stable injuries amongst (orthopaedic) trauma surgeons. Injury. 2021;52:774–9.
Acknowledgements
We would like to thank Dr. Ben Arthur Marson, Clinical Research Fellow at department of Orthopaedics and Trauma at the University of Nottingham for his knowledge and assistance regarding functional outcomes and Patient Reported Outcome Measures in paediatric patients with musculoskeletal injuries.
Gelre Ziekenhuis: J. Ten Brinke, Alrijne Ziekenhuis: M. Leijnen, Gelderse Vallei: T. Nosewicz, Slingeland Ziekenhuis: D.L. Tiel Groenestege, OLVG: R. N. van Veen.
Funding
The institutions of the authors affiliated with St. Antonius Hospital and OLVG Hospital have received funding to support this work by an unrestricted grant from the Dutch organization for healthcare sciences and healthcare innovation, ZonMw, the Hague the Netherlands, grant number: 516012524.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest to declare for the execution of this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spierings, J.F., Willinge, G.J.A., Schuijt, H.J. et al. Direct discharge for children with a greenstick or torus fracture of the wrist is a non-inferior satisfactory solution to traditional treatment. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-023-02391-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-023-02391-w