Abstract
Purpose
In light of the international evolutions to establish inclusive trauma systems and to concentrate the care for the most severely injured in major trauma centres, we evaluated the degree of dispersion of trauma care in Belgium.
Methods
We used descriptive statistics to illustrate the dispersion of major trauma care in Belgium based on two independent administrative databases: the registry of Mobile Intensive Care Units (2009–2015) and the Belgian Hospital Discharge Dataset (2009–2014).
Results
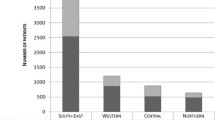
Patients with a severe trauma (n = 3856 in 2015) were transported towards 145 different hospital sites (on a total of 198 hospital sites) resulting in a median of 17 cases per hospital site (min = 1; P25 = 4; P75 = 30; max = 165). A minority of major trauma patients is after admission transferred to another hospital (8%) with a median of 10 days after admission to the hospital (IQR 3.5–24).
Conclusions
The dispersion of care for major trauma patients in Belgium is so high that a reorganisation of care for severe injured patients in major trauma centres concentrating professional expertise and specialised equipment is recommended to guarantee a high quality of care in a qualitative and sustainable way.

Source: Federal Public Service (FPS) Health, Food Chain Safety and Environment: Mobile Intensive Care Units (MICU) Data 2015
Similar content being viewed by others
References
WHO. Injuries and violence: the facts. 2010. http://www.who.int/violence_injury_prevention/key_facts/en/. Accessed 2 Oct 2015.
European Association for Injury Prevention and Safety Promotion (EuroSafe). Injuries in the European Union: summary of injury statistics for the years 2008–2010. Amsterdam; 2011.
European Association for Injury Prevention and Safety Promotion (EuroSafe). Injuries in the European Union: summary of injury statistics for the years 2010–2012. Amsterdam; 2013.
European Association for Injury Prevention and Safety Promotion (EuroSafe). Injuries in the European Union: summary of injury statistics for the years 2012–2014. Amsterdam; 2016.
Kim YJ. Relationship of trauma centre characteristics and patient outcomes: a systematic review. J Clin Nurs. 2014;23(3–4):301–14.
Caputo LM, Salottolo KM, Slone DS, Mains CW, Bar-Or D. The relationship between patient volume and mortality in American trauma centres: a systematic review of the evidence. Injury. 2014;45(3):478–86.
Minei JP, Fabian TC, Guffey DM, Newgard CD, Bulger EM, Brasel KJ, et al. Increased trauma center volume is associated with improved survival after severe injury: results of a Resuscitation Outcomes Consortium study. Ann Surg. 2014;260(3):456–64 (discussion 64).
Zacher MT, Kanz KG, Hanschen M, Haberle S, van Griensven M, Lefering R, et al. Association between volume of severely injured patients and mortality in German trauma hospitals. Br J Surg. 2015;102(10):1213–9.
Clement RC, Carr BG, Kallan MJ, Wolff C, Reilly PM, Malhotra NR. Volume–outcome relationship in neurotrauma care. J Neurosurg. 2013;118(3):687–93.
The Royal College of Surgeons of England. Provision of Trauma Care Policy Briefing. London: RCSE, September 2007. http://www.rcseng.ac.uk/rcseng/content/publications/docs/provision-of-trauma-care-1.
Nederlandse Vereniging voor Traumachirurgie. Levelcriteria NVT. 2013. http://www.trauma.nl/levelcriteria-nvt. Accessed 5 Jan 2018.
German Society for Trauma Surgery, Professional Association of Orthopaedic and Trauma Specialists. Whitebook medical care of the severely injured. Berlin: Deutsche Gesellschaft für Unfallchirurgie; 2012.
Landelijk Netwerk Acute Zorg. Landelijke Traumaregistratie 2010–2014. Rapportage Nederland; 2015.
Landelijk Netwerk Acute Zorg. Landelijke Traumaregistratie 2009–2013. Rapportage Nederland; 2014.
Lansink KW, Gunning AC, Spijkers AT, Leenen LP. Evaluation of trauma care in a mature level I trauma center in the Netherlands: outcomes in a Dutch mature level I trauma center. World J Surg. 2013;37(10):2353–9.
TraumaRegister DGU. 20 years of trauma documentation in Germany—actual trends and developments. Injury. 2014;45(Supplement 3):S14–9.
Ruchholtz S, Mand C, Lewan U, Debus F, Dankowski C, Kühne C, et al. Regionalisation of trauma care in Germany: the “TraumaNetwork DGU®-Project”. Eur J Trauma Emerg Surg. 2011;38(1):11–7.
NHS England. NHS standard contract for Major Trauma Services (all ages). London: NHS England; 2013.
Alfred Health Caring for the severely injured in Australia. Inaugural report of the Australian Trauma Registry. Melbourne: Alfred Health; 2014.
Trauma Association of Canada, Association Canadienne de Traumatologie. Trauma system. Accreditation guidelines. 2011.
Committee on trauma American College of Surgeons. Resources for optimal care of the injured patient. American college of Surgeons: Chicago; 2014
Innledning: nasjonal traumeplan—Traumesystem i Norge 2015 [Introduction: national trauma plan—Trauma System in Norway 2015].
Dehli T, Gaarder T, Christensen BJ, Vinjevoll OP, Wisborg T. Implementation of a trauma system in Norway: a national survey. Acta Anaesthesiol Scand. 2015;59(3):384–91.
Kristiansen T, Ringdal KG, Skotheimsvik T, Salthammer HK, Gaarder C, Naess PA, et al. Implementation of recommended trauma system criteria in south-eastern Norway: a cross-sectional hospital survey. Scand J Trauma Resusc Emerg Med. 2012;20:5.
Kristiansen T, Soreide K, Ringdal KG, Rehn M, Kruger AJ, Reite A, et al. Trauma systems and early management of severe injuries in Scandinavia: review of the current state. Injury. 2010;41(5):444–52.
NHS Clinical Advisory Groups Report. Regional networks for major trauma. London: NHS England; 2010.
Australasian Trauma Verification Program Officer. The Australasian trauma verification program manual. Royal Australasian College of Surgeons: Melbourne; 2009.
Ashley DW, Pracht EE, Medeiros RS, Atkins EV, NeSmith EG, Johns TJ, et al. An analysis of the effectiveness of a state trauma system: treatment at designated trauma centers is associated with an increased probability of survival. J Trauma Acute Care Surg. 2015;78(4):706–12 (discussion 12).
Di Bartolomeo S, Marino M, Ventura C, De Palma R. Evaluation of the survival benefit of trauma-centre care in the Italian setting. Injury. 2014;45(1):299–303.
Glance LG, Osler TM, Mukamel DB, Dick AW. Impact of trauma center designation on outcomes: is there a difference between level I and level II trauma centers? J Am Coll Surg. 2012;215(3):372–8.
Kuimi BL, Moore L, Cisse B, Gagne M, Lavoie A, Bourgeois G, et al. Influence of access to an integrated trauma system on in-hospital mortality and length of stay. Injury. 2015;46(7):1257–61.
Matsushima K, Schaefer EW, Won EJ, Armen SB. The outcome of trauma patients with do-not-resuscitate orders. J Surg Res. 2016;200(2):631–6.
Vickers BP, Shi J, Lu B, Wheeler KK, Peng J, Groner JI, et al. Comparative study of ED mortality risk of US trauma patients treated at level I and level II vs nontrauma centers. Am J Emerg Med. 2015;33(9):1158–65.
Dinh MM, Bein KJ, Gabbe BJ, Byrne CM, Petchell J, Lo S, et al. A trauma quality improvement programme associated with improved patient outcomes: 21 years of experience at an Australian Major Trauma Centre. Injury. 2014;45(5):830–4.
Dinh MM, Curtis K, Mitchell RJ, Bein KJ, Balogh ZJ, Seppelt I, et al. Major trauma mortality in rural and metropolitan NSW, 2009–2014: a retrospective analysis of trauma registry data. Med J Aust. 2016;205(9):403–7.
Moore L, Hanley JA, Turgeon AF, Lavoie A. Evaluation of the long-term trend in mortality from injury in a mature inclusive trauma system. World J Surg. 2010;34(9):2069–75.
Moore L, Turgeon AF, Lauzier F, Emond M, Berthelot S, Clement J, et al. Evolution of patient outcomes over 14 years in a mature, inclusive Canadian trauma system. World J Surg. 2015;39(6):1397–405.
Moore L, Stelfox HT, Evans D, Hameed SM, Yanchar NL, Simons R, et al. Trends in injury outcomes across Canadian trauma systems. JAMA Surg. 2016;152(2):168–74.
Dutton RP, Stansbury LG, Leone S, Kramer E, Hess JR, Scalea TM. Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns, 1997–2008. J Trauma. 2010;69(3):620–6.
Sarkar B, Brunsvold ME, Cherry-Bukoweic JR, Hemmila MR, Park PK, Raghavendran K, et al. American College of Surgeons’ Committee on Trauma Performance Improvement and Patient Safety program: maximal impact in a mature trauma center. J Trauma. 2011;71(5):1447–53 (discussion 53–4).
Moore L, Champion H, Tardif PA, Kuimi BL, O’Reilly G, Leppaniemi A, et al. Impact of trauma system structure on injury outcomes: a systematic review and meta-analysis. World J Surg. 2017.
Jansen JO, Lendrum RA, Morrison JJ. Trauma care in Scotland: the role of major trauma centres, trauma units, and local emergency hospitals. Surg J R Coll Surg Edinb Irel. 2016;14(5).
Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Hutchison JD, et al. Access to specialist care: optimizing the geographic configuration of trauma systems. J Trauma Acute Care Surg. 2015;79(5):756–65.
Deasy C, Cronin M, Cahill F, Geary U, Houlihan P, Woodford M, et al. Implementing major trauma audit in Ireland. Injury. 2016;47(1):166–72.
Décision concernant la planification de la médecine hautement spécialisée (MHS) dans le domaine de la prise en charge des blessés graves; 2015.
Van den Heede K, Dubois C, Devriese S, Baier N, Camaly O, Depuijdt E, et al. Organisation and payment of emergency care services in Belgium: current situation and options for reform. Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE); 2016.
Koninklijk besluit van 27 april 1998 houdende vaststelling van de normen waaraan een functie “gespecialiseerde spoedgevallenzorg” moet voldoen om erkend te worden. B.S. 19 juni 1998.
Van de Voorde C, Van den Heede K, Obyn C, Quentin W, Geissler A, Wittenbecher F, Busse R, Magnussen J, Camaly O, Devriese S, Gerkens S, Misplon S, Neyt M, Mertens R. Conceptual framework for the reform of the Belgian hospital payment system. Health Services Research (HSR) Brussels: Belgian Health Care Knowledge Centre (KCE). 2014. KCE Reports 229. D/2014/10.273/68.
Matsushima K, Schaefer EW, Won EJ, Armen SB, Indeck MC, Soybel DI. Positive and negative volume-outcome relationships in the geriatric trauma population. JAMA Surg. 2014;149(4):319–26.
Ambulancezorg Nederland, Nederlands Vereniging van Medisch Managers Ambulancezorg,V&NV Ambulancezorg. Landelijk Protocol Ambulancezorg; 2014.
German Trauma Society, German Society of General and Visceral Surgery, German Society of Anesthesiology and Intensive Care Medicine, German Society of Endovascular and Vascular Surgery, German Society of Hand Surgery, German Society of Oto-Rhino-Laryngology HaNS, et al. S3—guideline on treatrment of patients with severe and multiple injuries. English Version of the German Guideline S3—Leitlinie Polytrauma/Schwerverletzten-Behandlung. Berlin: German Trauma Society (DGU); 2012.
Christiaens W, Van de Walle E, Devresse S, Van Halewyck D, Benahmed N, Paulus D, et al. The view of severely burned patients and healthcare professionals on the blind spots in the aftercare process: a qualitative study. BMC Health Serv Res. 2015;15:302.
Acknowledgements
This study was funded by the Belgian Health Care Knowledge Centre (KCE). The KCE is a federal institution which is financed by the National Institute for Health and Disability Insurance (NIHDI, RIZIV—INAMI), the Federal Public Service of health, food chain safety and environment, and the Federal Public Service of social security. The development of health services research studies is part of the legal mission of the KCE. Although the development of the studies is paid by the KCE budget, the sole mission of the KCE is providing scientifically valid information.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors state that they have no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Van den Heede, K., Dubois, C., Mistiaen, P. et al. Evaluating the need to reform the organisation of care for major trauma patients in Belgium: an analysis of administrative databases. Eur J Trauma Emerg Surg 45, 885–892 (2019). https://doi.org/10.1007/s00068-018-0932-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0932-9