Abstract
The timing of fracture fixation in polytrauma patients has been debated for a long time. The decision between DCO (damage control orthopaedics) and ETC (early total care) is a difficult dilemma. Overzealous ETC in haemodynamically compromised patients with significant chest and head injuries can be detrimental. It has been shown, however, that early fracture fixation has a trend towards better outcome in patients with less severe injuries. Delaying all orthopaedic surgery in critically injured patients can be a safe alternative, but has several disadvantages like longer ICU stay and septic complications. The literature shows equivocal evidence for both settings. This article will summarize the historical background and controversies regarding patient assessment and decision making during the treatment of polytrauma patients. It will also give guidance for choosing DCO versus ETC in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ultimate frontier for the trauma surgeon is a rapid and evidenced-based clinical decision-making during the management of the critically injured polytrauma patient. Specifically, the decision between early total care (ETC) surgery as opposed to damage control surgery (DCS) continues to cause significant debate.
The pathophysiological changes in polytrauma include the effects of haemorrhagic shock and tissue damage. These, in combination with patient factors and secondary hits from surgical interventions, provide a proinflammatory state. If the inflammatory response is exaggerated or dysfunctional, the patient may progress from a systemic inflammatory response syndrome (SIRS) into multiple organ failure (MOF), leading to significant intensive care resources utilisation, longer hospital stay, increased long-term morbidity and mortality [1, 2]. Proponents of DCS recommend only absolute life-saving surgical interventions, waiting for the proinflammatory phase to pass before undertaking definitive surgical fixation. Advocates of ETC surgery highlight that the benefits of early skeletal stabilisation (reduced pain, easier positioning of the patient in the intensive care unit (ICU) and decreased blood loss) potentially outweigh the risks of SIRS and MOF. It is important to find a balance between both pathways without compromising patients’ physiology and to be able to recognise which patient will do better with primary or with delayed surgery.
This article will highlight the historical perspectives, the physiological assessment and the decision-making regarding the management of the polytrauma patient. The main aim is to emphasise the role and timing for ETC versus DCS during primary procedures and when to perform secondary surgeries when DCS was chosen.
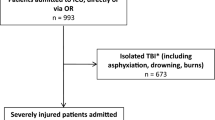
Population
There is currently no validated or consensus definition for the term “polytrauma” [3]. The term is mainly used to describe patients sustaining injuries to more than one body region, with altered physiology and a risk for secondary organ damage or a threat to life. The morbidity and mortality in these patients is higher than that expected from the summation of their anatomical injuries sustained. Polytrauma patients frequently have major skeletal injuries requiring specialist care and the careful timing of surgical management in the context of their torso and head injuries in combination with compromised physiology.
Historical perspective
The 20th century saw medical advances with profound effects on all facets of trauma care, resulting in patients surviving what were previously non-survivable injuries and allowed a new challenge to emerge––the surgical and critical care management of the polytrauma patient.
The timing of surgery in these patients is challenging. The concept of “too sick to operate” has been questioned from both sides of the Atlantic [4, 5] and Bone et al. [6] marked the beginning of ETC in a randomised trial.
The principles of surgical damage control by Rotondo et al. in 1993 marked a key change in the management of severe trauma [7]. Rotondo and Mattox both stressed that haemorrhage and contamination control are the top priority, and that hypothermia, acidosis and coagulopathy present the greatest threat to the patient. This is best treated with aggressive resuscitation and DCS, leaving definitive surgery until after resuscitation efforts have succeeded [8]. The understanding of the “two-hit” model of immune response resulted in the search for ways to minimise the second hit [9]. The recognition of harm associated with crystalloids [10, 11] has lead to a renewed focus on resuscitation strategies, with “haemostatic resuscitation” and “damage control resuscitation” being coined as terms [12].
Throughout the 1990s, concerns about the burden of ETC orthopaedics were well published, in particular in patients with associated head and chest injuries. No consensus was reached with multiple studies either refuting [13, 14] or confirming [15, 16] the safety of ETC in severe trauma. Reports of pulmonary complications and MOF in patients treated with primary internal fixation, as well as improving the understanding of the immunological component of severe trauma lead, to some resistance to ETC. The use of temporary external fixation was a safe alternative and, thus, damage control orthopaedics (DCO) was born [17, 18].
After an initial surge in popularity, it has been recognised that DCO has a significant implication for the patient and the health care system in regards to longer hospital stay and increased health care costs [19]. The rates of complication differ significantly across systems, regardless of the rates of DCS or ETC, suggesting that there are more factors at play [20].
Initial physiological assessment
The initial assessment of the polytrauma patient is crucial in order to determine the strategy for further management. The factors influencing the initial decision-making during limited time include physiological, injury pattern and patient factors, especially in the young patient that is able to initially compensate for haemorrhagic shock and in the elderly patient who is influenced by medication and comorbidities.
Physiological parameters
Classification (stable, borderline, unstable and in extremis)
Comprehensive physiological assessment is a fundamental component for optimising the modifiable factors during the initial management. In general, the biological and physiological condition is being assessed while the resuscitation is conducted. Historically, 2 L of crystalloid has been used as an initial fluid resuscitation [21], although the recent advancement of early massive transfusion with higher ratios of fresh frozen plasma/red blood cells and decreased amounts of crystalloid administration is dramatically changing this [22–25].
After the initial resuscitation, patients can be classified into four groups: stable, borderline, unstable and in extremis (based on Pape’s classification) [26].
Vital signs (BP/HR, lactate and BD)
The physiology of trauma patients is initially assessed using vital signs, heart rate (HR), blood pressure (BP), respiratory rate (RR), peripheral oxygen saturation (POS) and Glasgow Coma Scale (GCS) score. These parameters have been investigated over the decades. However, these values fail to prove to be sensitive enough by themselves in the initial assessment of patients or the prediction of poor outcome. In the early 1990s, several studies started to focus on blood gas analysis and demonstrated that the initial base excess and lactate are better predictors of outcome amongst multiply injured patients [27–29]. Point-of-care blood gas analysis has been shown to be as repeatable and accurate as laboratory-based testing, making critical information available far sooner [30, 31]. Blood gas analysis is an essential tool for the initial assessment of global perfusion in patients with haemorrhagic shock and assists in the initiation of massive transfusion. Sequential blood gas analysis can also provide guidance for identifying the endpoint of resuscitation [32]. A threshold base deficit (BD) of ≥6 mmol/L is universally used as an indicator of haemorrhagic shock, since a pre-resuscitation BD <5 mmol/L can uniformly predict survival [33, 34]. Lactic acidosis reflects the presence of anaerobic metabolism that, in trauma, is most likely the result of hypoperfusion. BD also appears to be reliable for assessing the normalisation of metabolic acidosis after haemorrhagic shock [35]. Similarly, the resolution of lactate acidosis correlates with survival in a time-dependent fashion [27].
Temperature
Hypothermia is a sign of shock, demonstrating a patient’s inability to control their core temperature. It is part of the bloody vicious cycle of coagulopathy and acidosis. Many enzymes of the clotting cascade are temperature-dependant and cannot work once the body temperature decreases to under a certain level [36]. The patient’s blood loses the ability to clot and the patient continues to bleed due to the combination of reduced enzyme activity and impaired platelet aggregation. Turning this patient around is a major challenge, as increasing the body temperature is a slow process, while the continuing resuscitation has the potential to cool the patient further. Trauma patients who develop this lethal cascade are likely to develop MOF [37]. Historically, the association between hypothermia and mortality has been reported [38–40].
Nevertheless, Gentilello et al. [41] demonstrated in their prospective cohort study that the early correction of hypothermia did not improve the survival rate. Also, a recent multi-centre, prospective observational study demonstrated that hypothermia itself does not predict mortality and concluded that hypothermia is a secondary phenomenon in nature and is reflective of insufficient circulation [37]. Although studies are inconsistent, hypothermia might be just an indicator of metabolic exhaustion and the failure of re-warming in these patients can lead to death. At this stage, we recommended to continuously monitor the temperature during the initial resuscitation and avoid unnecessary cooling due to environmental exposure in the emergency department and operating theatre. The usage of pre-warmed fluid and blood transfusions is standard care in most centres.
Coagulation
Recent studies have demonstrated that almost 25% of trauma patients are already coagulopathic on arrival to hospital, regardless of fluid resuscitation [42]. There are multiple definitions for coagulopathy, such as prolonged prothrombin time (PT), prolonged activated partial thromboplastin time (aPTT) or increased PT/aPTT ratio [32, 42–44]. These assays of blood coagulation in polytrauma are imperfect, since these are static measurements, performed at 37°C with a normal pH and only represent a snapshot of the past.
Platelet count is frequently used to assess coagulation and is one of the triggers for massive transfusion in some trauma centres [32]. It is one of the fastest blood tests available during the initial resuscitation and a value below 90,000 indicates impending traumatic intravascular coagulopathy [26].
Recent studies suggested that decreased fibrinogen is associated with coagulopathy and an increase in mortality [25, 45]. Fries et al. showed, in their in vitro study, that fibrinogen can reverse coagulopathy after haemodilution with crystalloid and colloids, but further animal and clinical studies are needed to confirm this [46]. Thus far, only one retrospective review of 252 patients at a US Army combat support hospital has shown improved survival with a high fibrinogen to red cell ratio in trauma patients [47]. However, these results were limited by the fact that fibrinogen was given as cryoprecipitate, plasma, platelets and whole blood, with each product containing other coagulation factors in varying amounts. Whether the survival benefit is a result of fibrinogen alone or in combination with other factors is currently still unknown. Fibrinogen supplementation could be beneficial in the coagulopathic trauma patient [45].
Point-of-care tests for lactate and the international normalized ratio (INR) have become an important tool to assess shock and coagulation and help in the decision-making of the polytrauma patient in the emergency department. Increased blood lactate reflects inadequate tissue perfusion and, if prolonged and above 4 mmol/L, is associated with haemorrhagic shock, the development of MOF and increased mortality [27, 33, 48]. An INR >1.5 is consistently recognised as a marker of coagulopathy [42, 49] and is closely correlated with an increase in mortality [50]. Both tests are quick and readily available.
Thromboelastography, a dynamic test characterising clot formation and breakdown, can help in the real-time assessment of coagulation [51]. Contrary to other tests, it analyses whole blood, in particular, the speed of thrombus formation and breakdown. The traces are easy to read and the test can be performed at the patient’s actual body temperature, meaning that it does not mask the effects of hypothermia [52]. There are limitations to thromboelastography, as it cannot provide a diagnosis of specific factor deficiencies and does not reflect endothelial-related coagulation.
Assessment in regards to secondary surgeries
The management plan implies major secondary procedures for definitive fixation. The monitoring of parameters implies the same as that for the initial period after trauma.
Coagulation and cardiac sequelae are the most pertinent physiological concerns in haemorrhagic models of hypothermic shock, despite adequate volume replacement [52].
Hypothermia and coagulopathy often mandate a simplified approach to complex surgical problems. Few controlled investigations exist; however, clinical opinion strongly supports the active prevention of hypothermia in the acutely traumatised patient. Both passive and active re-warming techniques, including the use of warming blankets and other conductive heat devices, preclinical use of fluid warmers and extracorporeal devices in severe cases, have been successfully utilised. The ideal method of re-warming is unclear, but it must be individualised to the patient and varies among institutions. Conversely, hypothermia has selected clinical benefits when appropriately used in cases of trauma under clinical conditions. When sustained hypothermia was used, surprising survival rates were described in the course of accidental circulatory arrest.
Usually, re-warming has been achieved by the morning after admission. However, coagulopathy may still be ongoing in the aftermath of severe bleeding. If this issue continues for further days, an extended operation should be postponed. Other signs of ongoing problems are continuing pulmonary dysfunction and excessive interstitial fluid overload. The clinical parameters to monitor these functions have been described in numerous publications. In the clinical course, the lung is the first organ to fail and also represents the most frequent organ system developing dysfunction. Among the reasons for lung failure during the course of multiple organ dysfunction syndrome (MODS), the theory of the “first filter” also has to be taken into consideration. Activated blood cells, cytokines, toxins and cell debris, often deriving from the areas of injury, are directly transported into the lung via the bloodstream.
Historically, three phases of pulmonary dysfunction have been differentiated, the third leading to a state of scarring of pulmonary tissue and often irreversible loss of organ function. Within days after the injury, changes of the vascular permeability with albumin extravasation into the interstitial space have been shown. Consequently, an increase in extravascular lung water (EVLW) has been observed, which may result in the decompensation of lymph drainage and pulmonary interstitial oedema. These mechanisms are maintained by inflammatory reactions, such as the activation of monocytes and polymorphonuclear leukocytes, thus, inducing a release of proteases and cytokines. All of these mechanisms may also contribute to the vicious cycle leading to organ failure during the late course after injury (Table 1).
The practice of delaying complex definitive surgery implies that the biological burden of surgical trauma on the traumatised patient can be assessed. This was confirmed in a prospective study measuring proinflammatory cytokines. Clinically stable patients with an Injury Severity Score (ISS) >16 and a femoral shaft fracture were randomised to primary intramedullary nailing of the femur within 24 h versus initial temporarily stabilisation of the femur with external fixateur and subsequent intramedullary nailing. A sustained inflammatory response (higher levels of IL-6) was measured after primary (<24 h) intramedullary femoral instrumentation, but not after initial external fixation or after secondary conversion to an intramedullary implant. The authors concluded that DCO surgery appears to minimise the additional surgical impact induced by the acute stabilisation of the femur [52].
Other issues that have been discussed with regard to the DCO concept include the ideal timing to perform the secondary definitive surgery and whether it is safe to convert an external fixateur to an intramedullary nail or whether this is associated with an unacceptably high infection rate.
It was clearly shown that the post-trauma days 2–4 do not offer optimal conditions for definitive surgery. In general, during this period, marked immune reactions are ongoing and enhanced generalised oedema is observed [52].
Nevertheless, these patients represent a highly diverse group and individual clinical judgement is more reliable, especially when combined with information from the newer laboratory tests. In a retrospective analysis, it was found that a secondary procedure lasting for more than 3 h was associated with the development of MODS. Also, the patients who developed complications had their surgery performed between days 2 and 4, whereas patients who did not go on to develop MODS were operated between days 6 and 8 (p < 0.001) [52].
The measurement of inflammatory mediators has been shown to be sensitive in gauging the ongoing response in recovering patients. A prospective study has recently shown that polytraumatised patients submitted to secondary definitive surgery at days 2–4 developed a significantly increased inflammatory response, compared to those operated at days 6–8. It was concluded that, in different post-traumatic periods, a variable inflammatory response to comparable stimuli is observed.
Strategy in specific injury patterns
There are various competing priorities among injuries in the multiply injured patient. Severe abdominal and/or thoracic injuries have a high mortality due to haemorrhagic shock. In patients with concomitant severe head injury, the dilemma between hypotensive resuscitation and adequate perfusion pressure to prevent secondary brain damage needs to be balanced out.
Severe head injury and skeletal injuries
There are concerns regarding the timing of definitive long-bone fracture fixation in patients with closed head injury. The main problem is secondary brain injury as a consequence of hypoxia or hypotension during the procedure. This can be exacerbated with increased fluid resuscitation, which can increase cerebral oedema and can make intracranial pressure control difficult. However, the literature is inconclusive. In some studies, patients with early fixation had an increase in mortality, especially when reamed intramedullary devices were used [14], whilst Poole et al. [53] examined patients with traumatic brain injury (TBI) and found that patient outcome was dictated by the severity of brain injury and not the timing of fracture fixation.
In the ideal setting, an intracranial pressure (ICP) monitor is inserted and ongoing haemostatic resuscitation is continued before any skeletal stabilisation. The patient can be continuously monitored, and if cranial pressures are increasing, the surgeon can switch to damage control mode at any time.
Severe chest injury and skeletal injuries
Thoracic injury is one of the major factors influencing the management of polytrauma. Initial respiratory and/or cardiovascular stabilisation with surgical haemostasis should be achieved and prioritised. The preventative strategy for acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), and subsequent MOF need to be considered, as the definitive surgical fixation of long-bone fractures often cause secondary damage to lung tissue, especially in patients with pulmonary contusions [13]. The clinical relevance of this varies from patient to patient.
However, it is important to recognise the severity of pulmonary damage. Pulmonary contusion, which may be initially subtle, can easily develop ARDS, as described in both clinical and animal studies [54, 55]. Reported mortality in polytrauma patients with pulmonary contusion has been more than 20%, which substantially increases with additional injuries [56, 57].
Clinical decision of the applicability of ETC should be based on clinical parameters (not the ISS), such as the PaO2/FiO2 ratio or the existence of pulmonary contusion [58]. In patients with concomitant pleural injuries, such as haemothorax or pneumothorax, an expeditious intercostal catheter (ICC) needs to be inserted. Patients that respond well to ICC insertion, with confirmed expanded lungs and good drainage, might still be candidates for ETC once their physiology is stabilised. In patients with pulmonary contusions and unfavourable parameters or with a chest injury that requires surgical operation, DCO should be initiated.
The big advantage in choosing ETC in suitable patients is the early positioning in the ICU with shorter ventilator time, shorter ICU length of stay and decreased complications such as ventilation-related pneumonia and sepsis [59].
Major abdominal injuries and skeletal injuries
Haemorrhagic shock due to abdominal injury is the main priority before any surgical skeletal stabilisation. However, the management for concomitant retroperitoneal bleeding due to an unstable pelvic fracture remains controversial due to two competing priorities and variations in the infrastructure of trauma centres. In the “unstable” patient with major abdominal/vascular injury, surgical haemostasis is the main priority for the initial surgery and DCS/DCO are probably indicated [59].
There is no consensus in regards to the “borderline” patient as to which approach should be used. Nevertheless, some studies demonstrated that, if the physiology is restored with early aggressive resuscitation, then ETC is still feasible [60–62]. Haemorrhage control in the abdomen or pelvis is the main priority. In patients with good response to resuscitation/surgery, definitive fixation can be done and is superior to DCO. A shorter mechanical ventilation time, ICU stay and total hospital stay can be achieved [60]. Monitoring the response to initial resuscitation and surgery in order to guide the mode of treatment is highly warranted.
Multiple skeletal injuries
The gold standard for multiple long-bone fractures is stabilisation in the first 24 h [6, 26, 63]. The debate regarding DCO versus ETC is currently ongoing, especially in patients with head and chest injuries, where ETC is thought to be potentially harmful [13, 14, 64]. It has been shown that patients with longer surgery time do have a higher incidence of ARDS and MOF [26]. Indicators for increased risk for developing organ dysfunction (platelet count, urine output, lactate, base deficit, temperature, transfusions and PaO2/FiO2 ratio) can help to assess the patient intraoperatively and, if necessary, change the management from ETC to DCO or vice versa.
Conclusions
The polytrauma patient needs a timely multidisciplinary team approach. The patient is kept warm in the resuscitation bay and all fluids are pre-warmed, as well as the operating theatre is heated up. Good communication between the anaesthetist and the surgeon is crucial. The overall decision-making from early total care (ETC) surgery to damage control orthopaedics (DCO) or vice versa is a dynamic process that can change at any stage during the resuscitation or initial operative period, and has to be adjusted to the patient’s physiological response, especially in the borderline patient.
References
Evans JA, van Wessem KJ, McDougall D, Lee KA, Lyons T, Balogh ZJ. Epidemiology of traumatic deaths: comprehensive population-based assessment. World J Surg. 2010;34(1):158–63.
Dewar D, Moore FA, Moore EE, Balogh Z. Postinjury multiple organ failure. Injury. 2009;40(9):912–8.
Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40:S12–22.
Goris RJ, Gimbrère JS, van Niekerk JL, Schoots FJ, Booy LH. Early osteosynthesis and prophylactic mechanical ventilation in the multitrauma patient. J Trauma. 1982;22(11):895–903.
Seibel R, LaDuca J, Hassett JM, Babikian G, Mills B, Border DO, et al. Blunt multiple trauma (ISS 36), femur traction, and the pulmonary failure-septic state. Ann Surg. 1985;202(3):283–95.
Bone LB, Johnson KD, Weigelt J, Scheinberg R. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am. 1989;71(3):336–40.
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR 3rd, Fruchterman TM, Kauder DR, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma. 1993;35(3):375–82. Discussion 382–3.
Moore EE, Burch JM, Franciose RJ, Offner PJ, Biffl WL. Staged physiologic restoration and damage control surgery. World J Surg. 1998;22(12):1184–90. Discussion 1190–1.
Pape HC, Schmidt RE, Rice J, van Griensven M, das Gupta R, Krettek C, et al. Biochemical changes after trauma and skeletal surgery of the lower extremity: quantification of the operative burden. Crit Care Med. 2000;28(10):3441–8.
Balogh Z, McKinley BA, Cocanour CS, Kozar RA, Valdivia A, Sailors RM, et al. Supranormal trauma resuscitation causes more cases of abdominal compartment syndrome. Arch Surg. 2003;138(6):637–42. Discussion 642–3.
Ley EJ, Clond MA, Srour MK, Barnajian M, Mirocha J, Margulies DR, et al. Emergency department crystalloid resuscitation of 1.5 L or more is associated with increased mortality in elderly and nonelderly trauma patients. J Trauma. 2011;70(2):398–400.
Duchesne JC, Kimonis K, Marr AB, Rennie KV, Wahl G, Wells JE, et al. Damage control resuscitation in combination with damage control laparotomy: a survival advantage. J Trauma. 2010;69(1):46–52.
Pape H-C, Auf’m’Kolk M, Paffrath T, Regel G, Sturm JA, Tscherne H. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion—a cause of posttraumatic ARDS? J Trauma. 1993;34(4):540–7. Discussion 547–8.
Jaicks RR, Cohn SM, Moller BA. Early fracture fixation may be deleterious after head injury. J Trauma. 1997;42(1):1–5. Discussion 5–6
Boulanger BR, Stephen D, Brenneman FD. Thoracic trauma and early intramedullary nailing of femur fractures: are we doing harm? J Trauma. 1997;43(1):24–8.
Scalea TM, Scott JD, Brumback RJ, Burgess AR, Mitchell KA, Kufera JA, et al. Early fracture fixation may be “just fine” after head injury: no difference in central nervous system outcomes. J Trauma. 1999;46(5):839–46.
Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg Am. 2000;82(6):781–8.
Scalea TM, Boswell SA, Scott JD, Mitchell KA, Kramer ME, Pollak AN. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma. 2000;48(4):613–21. Discussion 621–3.
Giannoudis PV, Giannoudi M, Stavlas P. Damage control orthopaedics: lessons learned. Injury. 2009;40(Suppl 4):S47–52.
O’Toole RV, O’Brien M, Scalea TM, Habashi N, Pollak AN, Turen CH. Resuscitation before stabilization of femoral fractures limits acute respiratory distress syndrome in patients with multiple traumatic injuries despite low use of damage control orthopedics. J Trauma. 2009;67(5):1013–21.
American College of Surgeons, Committee on Trauma. ATLS, advanced trauma life support for doctors. 8th ed. Chicago, IL: American College of Surgeons; 2008.
Zink KA, Sambasivan CN, Holcomb JB, Chisholm G, Schreiber MA. A high ratio of plasma and platelets to packed red blood cells in the first 6 hours of massive transfusion improves outcomes in a large multicenter study. Am J Surg. 2009;197(5):565–70. Discussion 570.
Scalea TM, Bochicchio KM, Lumpkins K, Hess JR, Dutton R, Pyle A, et al. Early aggressive use of fresh frozen plasma does not improve outcome in critically injured trauma patients. Ann Surg. 2008;248(4):578–84.
Duchesne JC, Hunt JP, Wahl G, Marr AB, Wang YZ, Weintraub SE, et al. Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma. 2008;65:272–6. Discussion 276–8.
Gonzalez EA, Moore FA, Holcomb JB, Miller CC, Kozar RA, Todd SR, et al. Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma. 2007;62(1):112–9.
Pape HC, Giannoudis PV, Krettek C, Trentz O. Timing of fixation of major fractures in blunt polytrauma: role of conventional indicators in clinical decision making. J Orthop Trauma. 2005;19(8):551–62.
Abramson D, Scalea TM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J. Lactate clearance and survival following injury. J Trauma. 1993;35(4):584–8. Discussion 588–9.
Waydhas C, Nast-Kolb D, Jochum M, Trupka A, Lenk S, Fritz H, et al. Inflammatory mediators, infection, sepsis, and multiple organ failure after severe trauma. Arch Surg. 1992;127(4):460–7.
Roumen RM, Redl H, Schlag G, Sandtner W, Koller W, Goris RJ. Scoring systems and blood lactate concentrations in relation to the development of adult respiratory distress syndrome and multiple organ failure in severely traumatized patients. J Trauma. 1993;35(3):349–55.
Boldt J, Kumle B, Suttner S, Haisch G. Point-of-care (POC) testing of lactate in the intensive care patient. Accuracy, reliability, and costs of different measurement systems. Acta Anaesthesiol Scand. 2001;45(2):194–9.
Slomovitz BM, Lavery RF, Tortella BJ, Siegel JH, Bachl BL, Ciccone A. Validation of a hand-held lactate device in determination of blood lactate in critically injured patients. Crit Care Med. 1998;26(9):1523–8.
Hoyt DB, Dutton RP, Hauser CJ, Hess JR, Holcomb JB, Kluger Y, et al. Management of coagulopathy in the patients with multiple injuries: results from an international survey of clinical practice. J Trauma. 2008;65(4):755–64. Discussion 764–5.
Siegel JH, Rivkind AI, Dalal S, Goodarzi S. Early physiologic predictors of injury severity and death in blunt multiple trauma. Arch Surg. 1990;125(4):498–508.
Randolph LC, Takacs M, Davis KA. Resuscitation in the pediatric trauma population: admission base deficit remains an important prognostic indicator. J Trauma. 2002;53(5):838–42.
Davis JW, Kaups KL, Parks SN. Base deficit is superior to pH in evaluating clearance of acidosis after traumatic shock. J Trauma. 1998;44(1):114–8.
Wolberg AS, Meng ZH, Monroe DM 3rd, Hoffman M. A systematic evaluation of the effect of temperature on coagulation enzyme activity and platelet function. J Trauma. 2004;56(6):1221–8.
Beilman GJ, Blondet JJ, Nelson TR, Nathens AB, Moore FA, Rhee P, et al. Early hypothermia in severely injured trauma patients is a significant risk factor for multiple organ dysfunction syndrome but not mortality. Ann Surg. 2009;249(5):845–50. doi:10.1097/SLA.0b013e3181a41f6f.
Shafi S, Elliott AC, Gentilello L. Is hypothermia simply a marker of shock and injury severity or an independent risk factor for mortality in trauma patients? Analysis of a large national trauma registry. J Trauma. 2005;59(5):1081–5. pii:00005373-200511000-00010.
Martin RS, Kilgo PD, Miller PR, Hoth JJ, Meredith JW, Chang MC. Injury-associated hypothermia: an analysis of the 2004 National Trauma Data Bank. Shock. 2005;24(2):114–8. pii:00024382-200508000-00003.
Watts DD, Trask A, Soeken K, Perdue P, Dols S, Kaufmann C. Hypothermic coagulopathy in trauma: effect of varying levels of hypothermia on enzyme speed, platelet function, and fibrinolytic activity. J Trauma. 1998;44(5):846–54.
Gentilello LM, Jurkovich GJ, Stark MS, Hassantash SA, O’Keefe GE. Is hypothermia in the victim of major trauma protective or harmful? A randomized, prospective study. Ann Surg. 1997;226(4):439–47. Discussion 447–9.
Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003;54(6):1127–30.
Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38(3):298–304.
Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38(2):185–93.
Stinger HK, Spinella PC, Perkins JG, Grathwohl KW, Salinas J, Martini WZ, et al. The ratio of fibrinogen to red cells transfused affects survival in casualties receiving massive transfusions at an army combat support hospital. J Trauma. 2008;64(2 Suppl):S79–85. doi:10.1097/TA.0b013e318160a57b. Discussion S85.
Fries D, Innerhofer P, Reif C, Streif W, Klingler A, Schobersberger W, et al. The effect of fibrinogen substitution on reversal of dilutional coagulopathy: an in vitro model. Anesth Analg. 2006;102(2):347–51. doi:10.1213/01.ane.0000194359.06286.d4.
Fries D, Martini WZ. Role of fibrinogen in trauma-induced coagulopathy. Br J Anaesth. 2010;105(2):116–21. doi:10.1093/bja/aeq161.
Manikis P, Jankowski S, Zhang H, Kahn RJ, Vincent JL. Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am J Emerg Med. 1995;13(6):619–22.
Yuan S, Ferrell C, Chandler WL. Comparing the prothrombin time INR versus the APTT to evaluate the coagulopathy of acute trauma. Thromb Res. 2007;120(1):29–37.
Niles SE, McLaughlin DF, Perkins JG, Wade CE, Li Y, Spinella PC, et al. Increased mortality associated with the early coagulopathy of trauma in combat casualties. J Trauma. 2008;64(6):1463–5.
Rugeri L, Levrat A, David JS, Delecroix E, Floccard B, Gros A, et al. Diagnosis of early coagulation abnormalities in trauma patients by rotation thrombelastography. J Thromb Haemost. 2007;5(2):289–95.
Kaufmann CR, Dwyer KM, Crews JD, Dols SJ, Trask AL. Usefulness of thrombelastography in assessment of trauma patient coagulation. J Trauma. 1997;42(4):716–20. Discussion 720–2.
Poole GV, Miller JD, Agnew SG, Griswold JA. Lower extremity fracture fixation in head-injured patients. J Trauma. 1992;32(5):654–9.
Oppenheimer L, Craven KD, Forkert L, Wood LD. Pathophysiology of pulmonary contusion in dogs. J Appl Physiol. 1979;47(4):718–28.
Fulton RL, Peter ET. The progressive nature of pulmonary contusion. Surgery. 1970;67(3):499–506.
Stellin G. Survival in trauma victims with pulmonary contusion. Am Surg. 1991;57(12):780–4.
Johnson JA, Cogbill TH, Winga ER. Determinants of outcome after pulmonary contusion. J Trauma. 1986;26(8):695–7.
Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, et al. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51(2):223–8. Discussion 229–30.
Pape H-C, Rixen D, Morley J, Husebye EE, Mueller M, Dumont C, et al. Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg. 2007;246(3):491–9. doi:10.1097/SLA.0b013e3181485750. Discussion 499–501.
Nicholas B, Toth L, van Wessem K, Evans J, Enninghorst N, Balogh ZJ. Borderline femur fracture patients: early total care or damage control orthopaedics? ANZ J Surg. 2011;81(3):148–53. doi:10.1111/j.1445-2197.2010.05582.x.
Enninghorst N, Toth L, King KL, McDougall D, Mackenzie S, Balogh ZJ. Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: a feasible option. J Trauma. 2010;68(4):935–41.
Nahm NJ, Como JJ, Wilber JH, Vallier HA. Early appropriate care: definitive stabilization of femoral fractures within 24 hours of injury is safe in most patients with multiple injuries. J Trauma. 2011;71(1)175–85. doi:10.1097/TA.0b013e3181fc93a2.
Johnson KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: effect of early operative stabilization of fractures. J Trauma. 1985;25(5):375–84.
Giannoudis PV, Veysi VT, Pape HC, Krettek C, Smith MR. When should we operate on major fractures in patients with severe head injuries? Am J Surg. 2002;183(3):261–7.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enninghorst, N., Peralta, R., Yoshino, O. et al. Physiological assessment of the polytrauma patient: initial and secondary surgeries. Eur J Trauma Emerg Surg 37, 559–566 (2011). https://doi.org/10.1007/s00068-011-0161-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-011-0161-y