Abstract
Background
Previous studies have demonstrated that female gender could be a prognostic factor in limited-disease (LD) small-cell lung cancer (SCLC), but the correlation between patient gender and survival parameters remains unclear.
Patients and methods
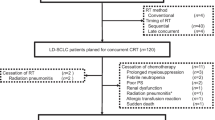
Data from 179 LD SCLC patients treated with definitive chemoradiotherapy (CRT) were reviewed. Influence of patient gender on time to progression (TTP), local control (LC), brain metastasis-free (BMFS), distant metastasis-free (DMFS) and overall survival (OS) was analysed.
Results
Definitive CRT was completed by 179 (110 men/69 women) patients. Of these, 68 (38%; 34 men/34 women) patients were treated in concurrent and 111 (62%; 76 men/35 women) in sequential mode. Prophylactic cranial irradiation (PCI) was subsequently applied in 70 (39%; 36 men/34 women) patients with partial or complete response after CRT. Median OS was 20 (95% confidence interval [CI] 10–22) and 14 (95% CI 10–18) months in female and male patients, respectively (p = 0.021). In subgroups defined by remission status (complete and partial response) after CRT, an OS benefit for females compared to males was also detected. There was no correlation between patient gender and TTP, LC or DMFS, and no difference in OS in the female and male subgroups treated with PCI. The incidence of metachronous brain metastases (BMs) in the male and female subgroups differed significantly (40/110 men vs. 18/69 women, p = 0.03). Also, mean BMFS was significantly longer in women (p = 0.023). Patient gender also significantly correlated with OS on multivariate analysis after adjustment for other prognostic factors (p = 0.04, HR 1.38, 95% CI 1.08–1.92).
Conclusion
In this heterogeneous LD SCLC patient cohort treated with definitive CRT, female gender was significantly associated with longer BMFS and OS, as well as with a lower incidence of metachronous brain failure.
Zusammenfassung
Hintergrund
Studien haben gezeigt, dass weibliches Geschlecht ein prognostischer Faktor beim kleinzelligen Lungenkarzinom (SCLC) im Stadium „limited disease“ (LD) sein könnte. Eine Korrelation zwischen Geschlecht und weiteren Überlebensparametern ist weiterhin unklar.
Patienten und Methoden
Behandlungsdaten von 179 LD-SCLC-Patienten mit definitiver Radiochemotherapie (CRT) wurden retrospektiv analysiert. Der Einfluss des Patientengeschlechts auf die Zeit bis zur Krankheitsprogression (TTP), lokale Kontrolle (LC), hirnmetastasenfreies (BMFS), fernmetastasenfreies (DMFS) und Gesamtüberleben (OS) wurden untersucht.
Ergebnisse
Eine CRT beendeten 179 Patienten (110 Männer/69 Frauen) erfolgreich. Die CRT erfolgte bei 68 Patienten simultan (38%; 34 Männern/34 Frauen), bei 111 Patienten sequentiell (62%; 76 Männern/35 Frauen). Eine anschließende prophylaktische Ganzhirnbestrahlung (PCI) erhielten 70 Patienten (39%; 36 Männern/34 Frauen) mit kompletter oder partieller Remission nach CRT. Das mediane OS betrug je 20 (95%-Konfidenzintervall [KI] 10–22) und 14 (95%-KI 10–18) Monate bei weiblichen und männlichen Patienten (p = 0,021). Subgruppenanalysen, definiert nach dem erreichten Remissionsstatus (komplett und partiell), ergaben einen Überlebensvorteil für Frauen gegenüber Männern. Es bestand keine Korrelation zwischen Geschlecht und TTP, LC und DMFS und kein Unterschied im OS zwischen Männern und Frauen mit PCI. Die Inzidenz für metachrone Hirnmetastasen unterschied sich zwischen den Geschlechtern signifikant (40/110 Männern vs. 18/69 Frauen; p = 0,03). Das BMFS war jedoch signifikant länger bei Frauen (p = 0,023). Geschlecht und OS korrelierten auch in der multivariaten Analyse signifikant (p = 0,04; HR 1,38; 95%-KI 1,08–1,92).
Schlussfolgerung
In dieser heterogenen Kohorte von LD-SCLC-Patienten, behandelt mit definitiver CRT, korreliert weibliches Geschlecht signifikant mit längerem OS und BMFS sowie mit geringer Inzidenz für metachrone Hirnmetastasierung.




Similar content being viewed by others
Abbreviations
- BM:
-
Brain metastasis
- CRT:
-
Chemoradiotherapy
- CT:
-
Computed tomography
- DMFS:
-
Distant metastasis-free survival
- LD:
-
Limited disease
- OS:
-
Overall survival
- PCI:
-
Prophylactic cranial irradiation
- PS:
-
Performance status
- SCLC:
-
Small-cell lung cancer
- TRT:
-
Thoracic radiation therapy
- TTP:
-
Time to progression
References
Govindan R, Page N, Morgensztern D et al (2006) Changing epidemiology of small-cell lung cancer in the united states over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol 24:4539–4544. doi:10.1200/JCO.2005.04.4859
Pignon J‑P, Arriagada R, Ihde DC et al (1992) A Meta-analysis of thoracic radiotherapy for small-cell lung cancer. N Engl J Med 327:1618–1624. doi:10.1056/NEJM199212033272302
Pijls-Johannesma MCG, De Ruysscher D, Lambin P et al (2005) Early versus late chest radiotherapy for limited stage small cell lung cancer. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004700.pub2
Fried DB, Morris DE, Poole C et al (2004) Systematic review evaluating the timing of thoracic radiation therapy in combined modality therapy for limited-stage small-cell lung cancer. J Clin Oncol 22:4837–4845. doi:10.1200/JCO.2004.01.178
Murray N, Coy P, Pater JL et al (1993) Importance of timing for thoracic irradiation in the combined modality treatment of limited-stage small-cell lung cancer. The National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 11:336–344
Fiegl M, Pircher A, Waldthaler C et al (2014) Small steps of improvement in small-cell lung cancer (SCLC) within two decades: a comprehensive analysis of 484 patients. Lung Cancer 84:168–174. doi:10.1016/j.lungcan.2014.02.005
Kubota K, Hida T, Ishikura S et al (2014) Etoposide and cisplatin versus irinotecan and cisplatin in patients with limited-stage small-cell lung cancer treated with etoposide and cisplatin plus concurrent accelerated hyperfractionated thoracic radiotherapy (JCOG0202): a randomised phase 3 study. Lancet Oncol 15:106–113. doi:10.1016/S1470-2045(13)70511-4
Lally BE, Geiger AM, Urbanic JJ et al (2009) Trends in the outcomes for patients with limited stage small cell lung cancer: an analysis of the surveillance, epidemiology, and end results database. Lung Cancer 64:226–231. doi:10.1016/j.lungcan.2008.08.010
Takei H, Kondo H, Miyaoka E et al (2014) Surgery for small cell lung cancer. J Thorac Oncol 9:1140–1145. doi:10.1097/JTO.0000000000000226
Takada M, Fukuoka M, Kawahara M et al (2002) Phase III study of concurrent versus sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small-cell lung cancer: results of the Japan Clinical Oncology Group Study 9104. J Clin Oncol 20:3054–3060
Turrisi AT, Kim K, Blum R et al (1999) Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. N Engl J Med 340:265–271. doi:10.1056/NEJM199901283400403
Manapov F, Klautke G, Fietkau R (2008) Prevalence of brain metastases immediately before prophylactic cranial irradiation in limited disease small cell lung cancer patients with complete remission to chemoradiotherapy: a single institution experience. J Thorac Oncol 3:652–655. doi:10.1097/JTO.0b013e3181757a76
Manapov F, Niyazi M, Gerum S et al (2016) Evaluation of the role of remission status in a heterogeneous limited disease small-cell lung cancer patient cohort treated with definitive chemoradiotherapy. BMC Cancer 16:216. doi:10.1186/s12885-016-2245-x
Albain KS, Crowley JJ, LeBlanc M, Livingston RB (1990) Determinants of improved outcome in small-cell lung cancer: an analysis of the 2,580patient Southwest Oncology Group data base. J Clin Oncol 8:1563–1574
Wolf M, Holle R, Hans K et al (1991) Analysis of prognostic factors in 766 patients with small cell lung cancer (SCLC): the role of sex as a predictor for survival. Br J Cancer 63:986–992
Svensson G, Ewers S, Ohlsson O, Olsson H (2014) Gender-related survival in different stages of lung cancer – a population study over 20 years. Open J Intern Med 04(03):47–58. doi:10.4236/ojim.2014.43008
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O. Roengvoraphoj, C. Eze, M. Niyazi, M. Li, G. Hildebrandt, R. Fietkau, C. Belka and F. Manapov declare no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Olarn Roengvoraphoj and Chukwuka Eze contributed equally to this work
Rights and permissions
About this article
Cite this article
Roengvoraphoj, O., Eze, C., Niyazi, M. et al. Prognostic role of patient gender in limited-disease small-cell lung cancer treated with chemoradiotherapy. Strahlenther Onkol 193, 150–155 (2017). https://doi.org/10.1007/s00066-016-1073-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1073-x