Abstract
Right ventricular (RV) function is a critical determinant of the prognosis of patients with pulmonary hypertension (PH). Upon establishment of PH, RV dysfunction develops, leading to a gradual worsening of the condition over time, culminating in RV failure and premature mortality. Despite this understanding, the underlying mechanisms of RV failure remain obscure. As a result, there are currently no approved therapies specifically targeting the right ventricle. One contributing factor to the lack of RV-directed therapies is the complexity of the pathogenesis of RV failure as observed in animal models and clinical studies. In recent years, various research groups have begun utilizing multiple models, including both afterload-dependent and afterload-independent models, to investigate specific targets and pharmacological agents in RV failure. In this review, we examine various animal models of RV failure and the recent advancements made utilizing these models to study the mechanisms of RV failure and the potential efficacy of therapeutic interventions, with the ultimate goal of translating these findings into clinical practice to enhance the management of individuals with PH.
Zusammenfassung
Die Rechtsherzfunktion spielt eine entscheidende Rolle für die Symptomatik und Prognose von Patienten mit pulmonaler Hypertonie (PH). Im Laufe der Erkrankung führt eine progrediente Rechtsherzbelastung zu einer allmählichen Verschlechterung der rechtsventrikulären (RV-)Funktion, die im Rechtsherzversagen und im vorzeitigen Tod der Patienten gipfelt. Trotz dieses grundlegenden pathophysiologischen Verständnisses bleiben die ursächlichen Mechanismen des Rechtsherzversagens unklar. Daher gibt es derzeit keine zugelassenen Therapien für eine zielgerichtete Behandlung des rechten Ventrikels. Ein Faktor, der hierzu beiträgt, ist die Komplexität der Pathogenese des Rechtsherzversagens, die in tierexperimentellen und klinischen Studien beobachtet wurde. In den letzten Jahren haben daher verschiedene Forschungsgruppen begonnen, Tiermodelle zu verwenden, darunter sowohl nachlastabhängige als auch nachlastunabhängige Modelle, um spezifische therapeutisch angehbare Ziele und pharmakologische Wirkstoffe bei Rechtsherzversagen zu untersuchen. In der vorliegenden Übersichtsarbeit werden verschiedene Tiermodelle des Rechtsherzversagens und die aktuellen Fortschritte dargestellt, die unter Verwendung dieser Modelle erzielt wurden, um die Mechanismen des Rechtsherzversagens und die potenzielle Wirksamkeit therapeutischer Interventionen zu untersuchen. Das ultimative Ziel dabei ist es, diese Ergebnisse in die klinische Praxis zu übersetzen, um somit das Management und die Therapie von PH-Patienten zu verbessern.

Similar content being viewed by others
Change history
09 May 2023
An Erratum to this paper has been published: https://doi.org/10.1007/s00059-023-05190-6
References
Woods RH (1892) A few applications of a physical theorem to membranes in the human body in a state of tension. J Anat Physiol 26(3):362–370
Mirsky I (1969) Left ventricular stresses in the intact human heart. Biophys J 9(2):189–208
Sanz J, Sanchez-Quintana D, Bossone E et al (2019) Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J Am Coll Cardiol 73(12):1463–1482
Todaro MC, Carerj S, Zito C et al (2020) Echocardiographic evaluation of right ventricular-arterial coupling in pulmonary hypertension. Am J Cardiovasc Dis 10(4):272–283
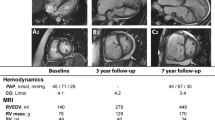
Rako ZA, Kremer N, Yogeswaran A et al (2023) Adaptive versus maladaptive right ventricular remodelling. ESC Heart Fail 10(2):762–775
Tello K, Gall H, Richter M et al (2019) Right ventricular function in pulmonary (arterial) hypertension. Herz 44(6):509–516
Humbert M, Kovacs G, Hoeper MM et al (2022) 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43(38):3618–3731. https://doi.org/10.1093/eurheartj/ehac237
Dignam JP, Scott TE, Kemp-Harper BK, Hobbs AJ (2022) Animal models of pulmonary hypertension:getting to the heart of the problem. Br J Pharmacol 179(5):811–837
Schultze AE, Wagner JG, White SM, Roth RA (1991) Early indications of monocrotaline pyrrole-induced lung injury in rats. Toxicol Appl Pharmacol 109(1):41–50
Gomez-Arroyo JG, Farkas L, Alhussaini AA et al (2012) The monocrotaline model of pulmonary hypertension in perspective. Am J Physiol Lung Cell Mol Physiol 302(4):L363–369
Rosenberg HC, Rabinovitch M (1988) Endothelial injury and vascular reactivity in monocrotaline pulmonary hypertension. Am J Physiol 255(6):H1484–1491
Urboniene D, Haber I, Fang YH et al (2010) Validation of high-resolution echocardiography and magnetic resonance imaging vs. high-fidelity catheterization in experimental pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 299(3):L401–412
Ruiter G, de Man FS, Schalij I et al (2013) Reversibility of the monocrotaline pulmonary hypertension rat model. Eur Respir J 42(2):553–556
West J, Hemnes A (2011) Experimental and transgenic models of pulmonary hypertension. Compr Physiol 1(2):769–782
Drexler ES, Bischoff JE, Slifka AJ et al (2008) Stiffening of the extrapulmonary arteries from rats in chronic hypoxic pulmonary hypertension. J Res Natl Inst Stand Technol 113(4):239–249
Meyrick B, Reid L (1980) Hypoxia-induced structural changes in the media and adventitia of the rat hilar pulmonary artery and their regression. Am J Pathol 100(1):151–178
Taraseviciene-Stewart L, Kasahara Y, Alger L et al (2001) Inhibition of the VEGF receptor 2 combined with chronic hypoxia causes cell death-dependent pulmonary endothelial cell proliferation and severe pulmonary hypertension. FASEB J 15(2):427–438
Bogaard HJ, Natarajan R, Mizuno S et al (2010) Adrenergic receptor blockade reverses right heart remodeling and dysfunction in pulmonary hypertensive rats. Am J Respir Crit Care Med 182(5):652–660
de Raaf MA, Schalij I, Gomez-Arroyo J et al (2014) SuHx rat model: partly reversible pulmonary hypertension and progressive intima obstruction. Eur Respir J 44(1):160–168
Suen CM, Chaudhary KR, Deng Y et al (2019) Fischer rats exhibit maladaptive structural and molecular right ventricular remodelling in severe pulmonary hypertension: a genetically prone model for right heart failure. Cardiovasc Res 115(4):788–799
Ciuclan L, Bonneau O, Hussey M et al (2011) A novel murine model of severe pulmonary arterial hypertension. Am J Respir Crit Care Med 184(10):1171–1182
Mamazhakypov A, Weiss A, Zukunft S et al (2020) Effects of macitentan and tadalafil monotherapy or their combination on the right ventricle and plasma metabolites in pulmonary hypertensive rats. Pulm circ 10(4):2045894020947283
Sydykov A, Luitel H, Mamazhakypov A et al (2020) Genetic deficiency and pharmacological stabilization of mast cells ameliorate pressure overload-induced maladaptive right ventricular remodeling in mice. Int J Mol Sci 21(23):9099
Mamazhakypov A, Sommer N, Assmus B et al (2021) Novel therapeutic targets for the treatment of right ventricular remodeling: insights from the pulmonary artery banding model. Int J Environ Res Public Health 18(16):8297
Müller M, Bischof C, Kapries T et al (2022) Right heart failure in mice upon pressure overload is promoted by mitochondrial oxidative stress. JACC Basic Transl Sci 7(7):658–677
Hemnes AR, Maynard KB, Champion HC et al (2012) Testosterone negatively regulates right ventricular load stress responses in mice. Pulm Circ 2(3):352–358
Andersen S, Schultz JG, Holmboe S et al (2018) A pulmonary trunk banding model of pressure overload induced right ventricular hypertrophy and failure. J Vis Exp. https://doi.org/10.3791/58050
Sydykov A, Mamazhakypov A, Petrovic A et al (2018) Inflammatory mediators drive adverse right ventricular remodeling and dysfunction and serve as potential biomarkers. Front Physiol 9:609
Egemnazarov B, Crnkovic S, Nagy BM et al (2018) Right ventricular fibrosis and dysfunction: actual concepts and common misconceptions. Matrix Biol 68–69:507–521
Lahm T, Douglas IS, Archer SL et al (2018) Assessment of right ventricular function in the research setting: knowledge gaps and pathways forward. An official American thoracic society research statement. Am J Respir Crit Care Med 198(4):e15–e43
Axelsen JB, Andersen S, Sun XQ et al (2019) Effects of 6‑mercaptopurine in pressure overload induced right heart failure. PLoS ONE 14(11):e225122
Nagendran J, Sutendra G, Paterson I et al (2013) Endothelin axis is upregulated in human and rat right ventricular hypertrophy. Circ Res 112(2):347–354
Bogaard HJ, Natarajan R, Henderson SC et al (2009) Chronic pulmonary artery pressure elevation is insufficient to explain right heart failure. Circulation 120(20):1951–1960
Akazawa Y, Okumura K, Ishii R et al (1985) Pulmonary artery banding is a relevant model to study the right ventricular remodeling and dysfunction that occurs in pulmonary arterial hypertension. J Appl Physiol 129(2):238–246
Amsallem M, Sweatt AJ, Arthur Ataam J et al (2021) Targeted proteomics of right heart adaptation to pulmonary arterial hypertension. Eur Respir J 57(4):2002428. https://doi.org/10.1183/13993003.02428-2020
Keranov S, Dorr O, Jafari L et al (2020) SPARCL1 as a biomarker of maladaptive right ventricular remodelling in pulmonary hypertension. Biomarkers 25(3):290–295
Piao L, Fang YH, Parikh K et al (2013) Cardiac glutaminolysis: a maladaptive cancer metabolism pathway in the right ventricle in pulmonary hypertension. J Mol Med 91(10):1185–1197
Borgdorff MA, Koop AM, Bloks VW et al (2015) Clinical symptoms of right ventricular failure in experimental chronic pressure load are associated with progressive diastolic dysfunction. J Mol Cell Cardiol 79:244–253
Boehm M, Tian XM et al (2020) Delineating the molecular and histological events that govern right ventricular recovery using a novel mouse model of pulmonary artery de-banding. Cardiovasc Res 116(10):1700–1709
Schermuly RT, Kreisselmeier KP, Ghofrani HA et al (2004) Chronic sildenafil treatment inhibits monocrotaline-induced pulmonary hypertension in rats. Am J Respir Crit Care Med 169(1):39–45
Lang M, Kojonazarov B, Tian X et al (2012) The soluble guanylate cyclase stimulator riociguat ameliorates pulmonary hypertension induced by hypoxia and SU5416 in rats. PLoS One 7(8):e43433
Boucherat O, Agrawal V, Lawrie A, Bonnet S (2022) The latest in animal models of pulmonary hypertension and right ventricular failure. Circ Res 130(9):1466–1486
Funding
Support: This work was supported by the Excellence Cluster Cardio-Pulmonary System (ECCPS) and the Collaborative Research Center (SFB) 1213—Pulmonary Hypertension and Cor Pulmonale, grant number SFB1213/1, projects A08 and B08 (German Research Foundation, Bonn, Germany).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Weiß, A. Mamazhakypov and R.T. Schermuly declare that they have no competing interests. A. Yogeswaran reports personal fees from MSD outside the submitted work.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
The original online version of this article was revised: Due to an editing error, the authors appeared in the wrong order, correct is: Athiththan Yogeswaran, Argen Mamazhakypov, Ralph T. Schermuly, Astrid Weiß
Rights and permissions
About this article
Cite this article
Yogeswaran, A., Mamazhakypov, A., Schermuly, R.T. et al. Right ventricular failure in pulmonary hypertension: recent insights from experimental models. Herz 48, 285–290 (2023). https://doi.org/10.1007/s00059-023-05180-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-023-05180-8
Keywords
- Pulmonary arteries
- Heart ventricle
- Right heart
- Right ventricular afterload
- Pulmonary vascular resistance