Abstract
The coronavirus disease 2019 (COVID-19) pandemic has resulted in numerous cases of illness and death worldwide. Research has shown that there are associations between transmission, as well as the severity of SARS-CoV‑2 (severe acute respiratory syndrome coronavirus 2) infections, and various environmental factors. For example, air pollution with particulate matter is thought to play a crucial role, and both climatic and geographical aspects must be considered. Furthermore, environmental conditions such as industry and urban lifestyle have a significant impact on air quality and thus on health aspects of the population. In this regard, other factors such as chemicals, microplastics, and diet also critically impact health, including respiratory and cardiovascular diseases. Overall, the COVID-19 pandemic has highlighted how closely health and the environment are linked. This review discusses the impact of environmental factors on the COVID-19 pandemic.
Zusammenfassung
Die COVID-19-Pandemie (Coronavirus Disease 2019) hat weltweit zu zahlreichen Krankheits- und Todesfällen geführt. Forschungsergebnisse haben gezeigt, dass es Zusammenhänge zwischen der Übertragung sowie dem Schweregrad von SARS-CoV-2-Infektionen (Severe Acute Respiratory Syndrome Coronavirus 2) mit verschiedenen Umweltfaktoren gibt. Es wird angenommen, dass beispielsweise die Luftverschmutzung mit Feinstaub eine entscheidende Rolle spielt, wobei sowohl klimatische als auch geografische Aspekte berücksichtigt werden müssen. Darüber hinaus haben Umweltbedingungen wie die Industrie und der städtische Lebensstil einen erheblichen Einfluss auf die Luftqualität und damit auf gesundheitliche Aspekte der Bevölkerung. Zudem beeinflussen weitere Faktoren wie Chemikalien, Mikroplastik und die Ernährung ebenfalls die Gesundheit einschließlich Atemwegs- und Herz-Kreislauf-Erkrankungen. Die COVID-19-Pandemie hat insgesamt deutlich gemacht, wie eng Gesundheit und Umwelt miteinander verknüpft sind. In der vorliegenden Übersichtsarbeit werden die Auswirkungen von Umweltfaktoren auf die COVID-19-Pandemie dargestellt..
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and was first described in December 2019, when 27 unexplained cases of pneumonia occurred at a large fish and animal market in Wuhan, Hubei Province, China [1, 2]. From there, a global viral outbreak occurred as the virus spread to other Asian countries and eventually to Europe, leading to the declaration of the COVID-19 pandemic on 11 March 2020 [1, 3]. The origin of SARS-CoV‑2 is still under investigation and remains the subject of scientific debate. However, much evidence suggests that the virus originated in animals and was transmitted to humans through a zoonotic event. The closest known relatives of SARS-CoV‑2 are bat coronaviruses, particularly those found in horseshoe bats in southern China. However, the virus has not been found in these bats or other animals studied to date. Therefore, it is thought that the virus may have originated in an animal intermediate host, where it underwent genetic changes that allowed it to infect humans. The identity of the intermediate host has not yet been determined, but several animals have been suggested as possible candidates, including pangolins and mink. It is possible that the virus was transmitted to humans through the handling or consumption of infected animals, as has been the case with other zoonotic viruses in the past [4]. This hypothesis regarding the zoonotic origin of SARS-CoV‑2 highlights the problem of the dramatic encroachment of the human population on the environment.
SARS-CoV‑2 is an enveloped positive-strand RNA virus that can enter cells via coronavirus spike proteins 1 and 2 [5]. Small genetic alterations in these spike proteins lead to increased pathogenicity of the virus and the formation of different viral variants [6]. During the pandemic, the Delta and Omicron variants played a crucial role as they are significantly more transmissible than other strains [6, 7]. Omicron is considered even more transmissible than the Delta variant and therefore has become the dominant variant in many countries. More than 50 different subvariants are now due to mutations [8]. SARS-CoV‑2 spreads by contact and droplet transmission and often causes nonspecific symptoms such as fever, headache, cough, nausea, diarrhea, fatigue, and myalgia [9]. This mild form of the disease must be distinguished from moderate, severe, and critical manifestations with the development of multiorgan failure [9]. However, it is also important to note the occurrence of asymptomatic courses, the impact of which on SARS-CoV‑2 transmission cannot yet be completely excluded [10]. As of early February 2023, SARS-CoV‑2 may be responsible for a total of more than 755 million confirmed infections worldwide, including nearly 7 million deaths [11]. The availability of vaccines as of December 2020 had a positive impact on the COVID-19 pandemic, as a significant decrease in symptomatic infections, severe courses, and SARS-CoV-2-related deaths was observed [12]. It is also known that SARS-CoV‑2, as we know from other viruses, is characterized by seasonal variations and regional variations [13]. Interestingly, local differences in transmission frequency and disease severity emerged during the pandemic. Here we will discuss the possible influences of environmental factors on the global COVID-19 pandemic (Fig. 1).
Environmental factors and their impact on health aspects and the spread and severity of SARS-CoV‑2. Environmental factors such as urban lifestyle, industrial pollution, mobility and transportation, geographic/climatic conditions, chemicals, microplastics, and nutrition have important influences on health aspects and can cause or exacerbate neurocognitive, upper respiratory tract, pulmonary, cardiovascular, liver, and gastrointestinal diseases. Furthermore, environmental factors influence the spread of SARS-CoV‑2, and the listed effects on preexisting diseases have a decisive influence on the severity of the disease course. This illustrates the critical influence of environmental factors on the COVID-19 pandemic. (Figure created with BioRender.com)
Mobility and transportation
The local outbreak of SARS-CoV‑2 in a market in China rapidly developed into a global health crisis. In the rapid spread of SARS-CoV‑2 across borders and continents, modern mobility and transportation systems proved to be important drivers of the pandemic. Dense flight schedules meant that the virus could be transmitted in the aircraft and to other continents within hours and days. COVID-19 outbreaks also occurred on ships, such as a cruise ship in Yokohama [14] and a French military aircraft carrier [15]. As a result of the rapid spread of SARS-CoV‑2, many countries implemented restrictions on global transportation, travel restrictions, and quarantine measures to contain transmission. Airlines and transportation companies have also taken steps to strengthen cleaning and disinfection procedures, improve air filtration systems, and require the use of masks. In addition, mobility data via cell phones and applications have been used to predict an area’s risk and assess risk to individual COVID-19 contacts [16].
Climate and geographics
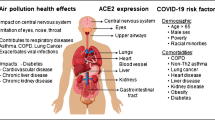
Several factors such as geographic location, climate, ozone, and weather events may favor the infection and spread of SARS-CoV‑2. In particular, countries above the equatorial line appear to be disadvantaged by weather events. Compared to the southern hemisphere, faster spread and higher mortality rates have been observed in these regions [17]. This is partly because the lower the temperature, the greater the number of cases [17]. An increased COVID-19 incidence was reported between 0 and 17 °C [18]. The climate can also indirectly affect the spread of the virus through human behavior. Wind strength and precipitation did not appear to have a particular effect on infection rates, and concerning humidity, a study in the Middle East Gulf States showed that an increase in relative humidity was associated with a decrease in the number of daily COVID-19 cases and deaths [19]. It was also found that patients admitted on days with higher temperatures, higher solar radiation, and lower humidity had a higher mortality rate [20]. In areas with low humidity, the virus can remain in the air for longer periods, increasing the risk of transmission. In addition, ozone (O3) also appears to play a role in the COVID-19 pandemic. Near the ground, O3is formed by a reaction between nitrogen dioxide (NO2), mostly from automobile exhaust, and oxygen (O2) under the influence of UV radiation. Above a permissible level of 180 μg/m3 in the air we breathe, it appears to have harmful consequences. Study results have shown that long-term exposure to fine particulate matter < 2.5 µm (PM2.5), NO2, and O3 is associated with an increased risk of COVID-19 infection [21]. Higher levels of O3 are known to exacerbate cardiovascular disease. Because SARS-CoV‑2 is in part an endothelial disease, O3 could potentially exacerbate SARS-CoV‑2 disease.
Interestingly, elevated concentrations of O3, carbon monoxide (CO), and PM2.5 were measured in Riyadh, Saudi Arabia, after a sandstorm. In the context of this event, there was a significant increase in SARS-CoV‑2 infections in the affected region. This leads to the hypothesis that air pollutants act as viral vectors and make the population more susceptible to infection [22].
Industrial pollution and urban lifestyle
In addition to climatic and geographic factors, the built environment, industry, and urban lifestyle have a critical influence on air quality and pollution. These influencing factors may play equally important roles in the transmission and severity of SARS-CoV‑2 infections. Poor indoor air quality may increase the risk of SARS-CoV‑2 transmission by allowing the virus to remain airborne for longer. This can be caused by inadequate ventilation, improper air filtration, and other factors affecting fresh air flow into indoor spaces. In addition, overcrowding, especially in low-income and multigenerational households, can increase the risk of SARS-CoV‑2 transmission because people live very close to each other and it is difficult to maintain a physical distance [23, 24]. The building design also plays a role here, influencing factors such as airflow, occupancy, and the ability to maintain a spatial distance [23]. For example, buildings with open floor plans and large windows may be better suited to promote ventilation. Proper building maintenance, such as regular cleaning and disinfection, can help reduce the risk of COVID-19 transmission by removing virus particles from surfaces and ensuring that HVAC systems are functioning properly [25]. Neighborhood factors such as access to green space, sidewalks, and other amenities that encourage physical activity can also influence overall health and the risk of COVID-19 comorbidities such as obesity and hypertension [23]. Another important factor is the influence of air pollution and related to this are several mechanisms that influence the risk and severity of COVID-19. Fine particulate matter is considered a potential SARS-CoV‑2 carrier and increases the likelihood of infection and severity of the disease [26, 27]. In this context, industrial processes can release a variety of air pollutants, including PM2.5, nitrogen oxides, and sulfur dioxide. Exposure to these air pollutants can increase the likelihood of viral transmission and exacerbate preexisting respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD), which are also risk factors for severe COVID-19 courses.
Several studies show an association between higher levels of air pollution and increased numbers, severity, and mortality rates of SARS-CoV‑2 infections [28,29,30]. Transportation of goods and materials associated with industry may also contribute to air pollution, especially in urban areas with high traffic volumes. In this regard, the effects of industrial air pollution may exacerbate existing health inequalities, particularly for low-income populations who are more likely to live near industrial facilities and be exposed to higher levels of pollution. A short-term increase in PM2.5 concentration of 10 μg/m3 increased the number of daily confirmed cases by 9.41% [31].
Urban lifestyle affects the severity of COVID-19 because cities tend to have high population density, which may increase the risk of COVID-19 transmission due to the proximity of people. In addition, air and environmental pollution and PM2.5 levels are usually higher in cities, which may exacerbate respiratory diseases and increase the severity of COVID-19. Urban lifestyle may also contribute to other risk factors for COVID-19 severity, such as unhealthy dietary habits and physical inactivity. Reducing industrial emissions and improving air quality, especially in densely populated areas, could be critical in reducing respiratory and cardiovascular disease and reducing the risk of severe COVID-19 [32, 44].
Chemicals and microplastics
The protective measures taken during the pandemic play an important role, as they are associated with multiple impacts on humans and the environment [33]. Disinfectants and cleaning agents were used more frequently and more extensively, resulting in significantly higher concentrations of quaternary ammonium compounds being detected indoors during the pandemic. Regular exposure to ammonium-containing substances increases inflammation, impairs cholesterol synthesis, and reduces mitochondrial function [34].
In addition to the greater use of cleaning products, disposable packaging was increasingly used to contain the spread of SARS-CoV‑2. In this process, global plastic consumption increased dramatically, in part due to recommended protective measures and the use of personal protective equipment [35, 36]. This waste leads to an increase in microplastics, which are defined as particles smaller than 5 mm. Since 2000, the pollution of the world’s oceans has been the subject of increasing scientific interest [37]. Microplastics can persist in the environment for hundreds of years and enter the natural ecosystem through various pathways. Humans ingest it through food, inhalation, and probably through the skin [38]. The accumulation of microplastics in the human body can lead to physical damage, inflammation, and oxidative stress, which in turn may lead to DNA damage. The association of DNA damage with tumor, cardiovascular, and neurodegenerative diseases suggests the pathological potential of chronic microplastic exposure to further make individuals more susceptible to diseases such as COVID-19 [39]. However, there are still significant gaps in elucidating the underlying pathomechanisms.
Nutrition
In addition to the potential ingestion of microplastics, changes in diet during the pandemic play an important role. Malnutrition, including inflammatory effects, could be an explanation for the severe courses of COVID-19 in the elderly and obese [40]. The trend went from fresh, healthy foods to ultra-processed carbohydrate-based foods. This dietary adaptation has multifactorial influences and is described by the term “food craving” [41]. These adapted behaviors adversely affect long-term health and may promote the development of obesity [42]. In addition to the pro-inflammatory component of obesity, this nutritional state is associated with diabetes mellitus, hyperlipidemia, and cardiovascular disease [43]. These, in turn, are among the risk factors for a severe course of SARS-CoV‑2 infection. However, it was not just diet that was affected, people’s entire lifestyle was negatively impacted. Daily physical activity was severely restricted at times, and increased sleep disturbance and lack of social contact also characterized the pandemic. The consequence of these adapted behaviors is a multifactorial limitation of the immune response [33]. Another issue in the context of food supply in pandemic conditions is the use of bioreactors to produce protein-rich foods such as meat and dairy products without the need for animal husbandry. This could have important implications for food safety and sustainability, especially as disruptions in the food supply chain occurred during the COVID-19 pandemic.
Conclusion
In addition to the origin of SARS-CoV‑2, the environment has also had a major impact on the course of the resulting disease, COVID-19. The global pandemic has had severe social and health impacts worldwide. Besides individual comorbidities, environmental factors were identified as triggers of the disease. Air pollution is one of the major risks, with particulate matter and ozone correlating with SARS-CoV‑2 infection and severity. A striking pathophysiological overlap exists between SARS-CoV‑2 and air pollution, as both affect the endothelium and the immune system. This increases the risk of a higher number and severity of infections in the acute phase, as well as the risk of cardiovascular and immunological diseases. SARS-CoV‑2 also had a tremendous impacted on the global economy. Since environmental factors, in particular air pollution, influence the outcome of the pandemic, they should be addressed more vigorously to prevent individual diseases and future social and financial losses.
References
World Health Organization (2021) Q&A on coronaviruses. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19. Accessed 12 Feb 2023
Centers for Disease Control and Prevention COVID-19.HAN Archive—00426|Health Alert Network (2020). Update and Interim Guidance on Outbreak of 2019 Novel Coronavirus (2019-nCoV) in Wuhan, China. https://emergency.cdc.gov/han/han00426.asp. Accessed 12 Feb 2023
World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 12 Feb 2023
Shereen MA, Khan S, Kazmi A et al (2020) COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res 24:91–98. https://doi.org/10.1016/j.jare.2020.03.005
Belouzard S, Millet JK, Licitra BN et al (2012) Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 4(6):1011–1033. https://doi.org/10.3390/v4061011
Centers for Disease Control and Prevention (2022) SARS-CoV‑2 variant classifications and definitions. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html. Accessed 12 Feb 2023
Liu Y, Rocklöv J (2021) The reproductive number of the delta variant of SARS-CoV‑2 is far higher compared to the ancestral SARS-CoV‑2 virus. J Travel Med 28(7):taab124. https://doi.org/10.1093/jtm/taab124
Centers for Disease Control and Prevention (2023) COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#variant-proportions. Accessed 12 Feb 2023
Umakanthan S, Sahu P, Ranade AV et al (2020) Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med J 96(1142):753–758. https://doi.org/10.1136/postgradmedj-2020-138234
Byambasuren O, Cardona M, Bell K et al (2020) Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. J Assoc Med Microbiol Infect Dis Can 5(4):223–234. https://doi.org/10.3138/jammi-2020-0030
World Health Organization (2023) WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed 12 Feb 2023
Fiolet T, Kherabi Y, MacDonald CJ et al (2022) Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV‑2 and variants of concern: a narrative review. Clin Microbiol Infect 28(2):202–221. https://doi.org/10.1016/j.cmi.2021.10.005
Rayan RA (2021) Seasonal variation and COVID-19 infection pattern: a gap from evidence to reality. Curr Opin Environ Sci Health 20:100238. https://doi.org/10.1016/j.coesh.2021.100238
Jimi H, Hashimoto G (2020) Challenges of COVID-19 outbreak on the cruise ship Diamond Princess docked at Yokohama, Japan: a real-world story. Glob Health Med 2(2):63–65. https://doi.org/10.35772/ghm.2020.01038
Chassery L, Texier G et al (2021) A COVID-19 outbreak on board ship: Analysis of the sociotechnical system of epidemiological management in the French Navy. Saf Sci 140:105296. https://doi.org/10.1016/j.ssci.2021.105296
Rahman MM, Paul KC, Hossain MA et al (2021) Machine learning on the COVID-19 pandemic, human mobility and air quality: a review. IEEE Access 9:72420–72450. https://doi.org/10.1109/ACCESS.2021.3079121
Adedokun KA, Olarinmoye AO et al (2020) A close look at the biology of SARS-CoV‑2, and the potential influence of weather conditions and seasons on COVID-19 case spread. Infect Dis Poverty 9(1):77. https://doi.org/10.1186/s40249-020-00688-1
McClymont H, Hu W (2021) Weather variability and COVID-19 transmission: a review of recent research. Int J Environ Res Public Health 18(2):396. https://doi.org/10.3390/ijerph18020396
Meo SA, Abukhalaf AA, Alomar AA et al (2020) Effect of temperature and humidity on the dynamics of daily new cases and deaths due to COVID-19 outbreak in Gulf countries in Middle East Region. Eur Rev Med Pharmacol Sci 24(13):7524–7533. https://doi.org/10.26355/eurrev_202007_21927
Hachim MY, Hachim IY, Naeem K et al (2021) Higher temperatures, higher solar radiation, and less humidity is associated with poor clinical and laboratory outcomes in COVID-19 patients. Front Public Health 9:618828. https://doi.org/10.3389/fpubh.2021.618828
Sidell MA, Chen Z, Huang BZ et al (2022) Ambient air pollution and COVID-19 incidence during four 2020–2021 case surges. Environ Res 208:112758. https://doi.org/10.1016/j.envres.2022.112758
Meo SA, Almutairi FJ, Abukhalaf AA et al (2021) Sandstorm and its effect on particulate matter PM 2.5, carbon monoxide, nitrogen dioxide, ozone pollutants and SARS-CoV-2 cases and deaths. Sci Total Environ 795:148764. https://doi.org/10.1016/j.scitotenv.2021.148764
Frumkin H (2021) COVID-19, the built environment, and health. Environ Health Perspect 129(7):75001. https://doi.org/10.1289/EHP8888
Alidadi M, Sharifi A (2022) Effects of the built environment and human factors on the spread of COVID-19: A systematic literature review. Sci Total Environ 850:158056. https://doi.org/10.1016/j.scitotenv.2022.158056
Talic S, Shah S, Wild H et al (2021) Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV‑2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ 375:e68302. https://doi.org/10.1136/bmj-2021-068302
Nor NSM, Yip CW, Ibrahim N et al (2021) Particulate matter (PM2.5) as a potential SARS-CoV‑2 carrier. Sci Rep 11(1):2508. https://doi.org/10.1038/s41598-021-81935-9
Conticini E, Frediani B, Caro D (2020) Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV‑2 lethality in Northern Italy? Environ Pollut 261:114465. https://doi.org/10.1016/j.envpol.2020.114465
Zhu Y, Xie J, Huang F, Cao L (2020) Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ 727:138704. https://doi.org/10.1016/j.scitotenv.2020.138704
Travaglio M, Yu Y, Popovic R et al (2021) Links between air pollution and COVID-19 in England. Environ Pollut 268(Pt A):115859. https://doi.org/10.1016/j.envpol.2020.115859
SanJuan-Reyes S, Gómez-Oliván LM, Islas-Flores H (2021) COVID-19 in the environment. Chemosphere 263:127973. https://doi.org/10.1016/j.chemosphere.2020.127973
Xu L, Taylor JE, Kaiser J (2022) Short-term air pollution exposure and COVID-19 infection in the United States. Environ Pollut 292(Pt B):118369. https://doi.org/10.1016/j.envpol.2021.118369
Brauer M, Casadei B et al (2021) Taking a stand against air pollution-the impact on cardiovascular disease: a joint opinion from the world heart federation, American College of Cardiology, American Heart Association, and the European Society of Cardiology. J Am Coll Cardiol 77(13):1684–1688. https://doi.org/10.1016/j.jacc.2020.12.003
Tagorti G, Kaya B (2022) Genotoxic effect of microplastics and COVID-19: The hidden threat. Chemosphere 286(Pt 3):131898. https://doi.org/10.1016/j.chemosphere.2021.131898
Hrubec TC, Seguin RP, Xu L et al (2021) Altered toxicological endpoints in humans from common quaternary ammonium compound disinfectant exposure. Toxicol Rep 8:646–656. https://doi.org/10.1016/j.toxrep.2021.03.006
Mohana AA, Islam MM, Rahman M et al (2022) Generation and consequence of nano/microplastics from medical waste and household plastic during the COVID-19 pandemic. Chemosphere 311(Pt 2):137014. https://doi.org/10.1016/j.chemosphere.2022.137014
Lee M, Kim H (2022) COVID-19 pandemic and microplastic pollution. Nanomaterials 12(5):851. https://doi.org/10.3390/nano12050851
Borja A, Elliott M (2019) So when will we have enough papers on microplastics and ocean litter? Mar Pollut Bull 146:312–316. https://doi.org/10.1016/j.marpolbul.2019.05.069
Schwabl P, Köppel S et al (2019) Detection of various microplastics in human stool: a prospective case series. Ann Intern Med 171(7):453–457. https://doi.org/10.7326/M19-0618
Barnes JL, Zubair M, John K et al (2018) Carcinogens and DNA damage. Biochem Soc Trans 46(5):1213–1224. https://doi.org/10.1042/BST20180519
Calder PC (2021) Nutrition and immunity: lessons for COVID-19. Eur J Clin Nutr 75(9):1309–1318. https://doi.org/10.1038/s41430-021-00949-8
Rodríguez-Martín BC, Meule A (2015) Food craving: new contributions on its assessment, moderators, and consequences. Front Psychol 6:21. https://doi.org/10.3389/fpsyg.2015.00021
Bracale R, Vaccaro CM (2020) Changes in food choice following restrictive measures due to Covid-19. Nutr Metab Cardiovasc Dis 30(9):1423–1426. https://doi.org/10.1016/j.numecd.2020.05.027
Mattioli AV, Sciomer S, Cocchi C et al (2020) Quarantine during COVID-19 outbreak: changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis 30(9):1409–1417. https://doi.org/10.1016/j.numecd.2020.05.020
Eyf W, Mathur S, Zhang R et al (2023) Association of COVID-19 with short- and long-term risk of cardiovascular disease and mortality: a prospective cohort in UK Biobank. Cardiovasc Res. https://doi.org/10.1093/cvr/cvac195
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Kreutz, J. Heitmann, A.-C. Schäfer, S. Aldudak, B. Schieffer and E. Schieffer declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Kreutz, J., Heitmann, J., Schäfer, AC. et al. Environmental factors and their impact on the COVID-19 pandemic. Herz 48, 234–238 (2023). https://doi.org/10.1007/s00059-023-05178-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-023-05178-2