Abstract
Chronic heart failure is one of the most common causes of hospitalization and death in industrialized countries. Demographic changes with an aging population are expected to further increase the prevalence of chronic heart failure. The associated increase in comorbidities in patients with chronic heart failure leads to a less favorable prognosis for survival. A selection of the major comorbidities discussed in this review—along with prevalence, impact on prognosis, treatment approaches, and current study status—include atrial fibrillation, arterial hypertension, coronary artery disease, coronary microvascular dysfunction, renal dysfunction, type 2 diabetes, sleep apnea, reduced lymphatic reserve, and the effects on oxygen utilization and physical activity. The complex clinical picture of heart failure with preserved ejection fraction (HFpEF) remains challenging in the nearly absence of evidence-based therapy. Except for comorbidity-specific guidelines, no HFpEF-specific treatment of comorbidities can be recommended at this time. Optimized care is becoming increasingly relevant to reducing hospitalizations through a seamless inpatient and outpatient care structure. Current treatment is focused on symptom relief and management of associated comorbidities. Therefore, prevention through early minimization of risk factors currently remains the best approach.
Zusammenfassung
Eine der häufigsten Todesursachen in den Industrieländern ist die chronische Herzinsuffizienz. Patienten mit dem Krankheitsbild einer chronischen Herzinsuffizienz gehören zu der Gruppe Patienten, die am häufigsten in die Krankenhäuser eingewiesen wird. Durch den demografischen Wandel mit zunehmender Alterung der Bevölkerung ist ein weiterer Anstieg der Prävalenz der chronischen Herzinsuffizienz zu erwarten. Der damit verbundene Anstieg der Komorbiditäten bei chronischen Herzinsuffizienzpatienten führt zu einer ungünstigeren Überlebensprognose. Eine Auswahl der wichtigsten Komorbiditäten, die in dieser Übersicht mit Prävalenz, Prognose, Behandlungsansätzen und aktuellem Studienstand erörtert werden, umfasst: Vorhofflimmern, arterielle Hypertonie, koronare Herzerkrankung, koronare mikrovaskuläre Dysfunktion, Nierenfunktionsstörung, Typ-2-Diabetes, Schlafapnoe, lymphatische Reserve sowie Auswirkungen auf die Sauerstoffverwertung und körperliche Aktivität. Das komplexe Krankheitsbild der Herzinsuffizienz mit erhaltener Ejektionsfraktion (HFpEF) stellt angesichts einer nahezu fehlenden evidenzbasierten Therapie weiterhin eine Herausforderung dar. Eine optimierte Versorgung wird immer wichtiger, um Krankenhausaufenthalte durch eine nahtlose stationäre und ambulante Versorgungsstruktur zu reduzieren. Die derzeitige Behandlung ist auf die Linderung der Symptome und die Behandlung der damit verbundenen Komorbiditäten ausgerichtet. Daher bleibt aktuell die Prävention durch die frühzeitige Minimierung von Risikofaktoren der beste Ansatz.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic heart failure is one of the most common causes of hospitalization and death in industrialized countries [5, 11]. In the Western world, the prevalence of heart failure is approximately 1–2%, and it increases steadily with age. The incidence is less than 1% in those under 55 years of age and reaches approximately 10% in those older than 70 [25]. According to the terminology given in the European Society of Cardiology (ESC) guidelines, patients with heart failure are divided into three different groups. A distinction is made between patients with normal ejection fraction (HFpEF: left ventricular ejection fraction [LVEF] ≥ 50%) and patients with reduced ejection fraction (HFrEF: LVEF < 40%). The group of patients with LVEF in the range of 40–49% represents a “gray area” and is defined as heart failure with mildly reduced ejection fraction (HFmrEF). Epidemiologic data from the Framingham Study, an international cohort study, shows an increase in the prevalence of HFpEF over the past three decades relative to the overall prevalence of heart failure (from 41% to 56%) and, conversely, a decrease in the prevalence of HFrEF (from 44% to 31%) and HFmrEF (from 15% to 13%; [43]).
Demographic changes with an aging population are expected to further increase the prevalence of chronic heart failure. The associated increase in comorbidities in patients with chronic heart failure leads to a less favorable prognosis for survival, as shown in Fig. 1 [17, 41].
Survival curve according to Cox model of the frequency distribution of patients with comorbidities (0, 1, 2, ≥ 3 comorbidities) with heart failure with preserved ejection fraction (HFpEF, b) and heart failure with reduced ejection fraction (HFrEF, a). With permission from [17]
The frequency distribution of patients with comorbidities with HFpEF compared with HFrEF differentiated by men and women is shown in Fig. 2. The graph shows that HFpEF patients have a higher number of concomitant diseases—four on average—than do patients with HFrEF in both sexes [12].
Frequency distribution of comorbidities in women (a) and men (b) with heart failure with preserved ejection fraction (HFpEF, orange) and heart failure with reduced ejection fraction (HFrEF, blue). With permission from [12]
Comorbidities: prevalence, impact on prognosis, treatment options
Since no HFpEF-specific treatment methods for comorbidities currently exist, treatment recommendations based on comorbidity-specific guidelines are recommended by current guidelines [24].
Atrial fibrillation
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia. The estimated prevalence of AF in adults is between 2% and 4% worldwide [15]. If both heart failure and AF coexist, the risk for worse outcomes is not only the summation of each individual disease but it increases exponentially, with a major increase in hospitalizations and a two- to three-fold higher mortality [15, 18].
According to epidemiological studies, there is a substantial association between AF and HFpEF: AF is one of the most common precursors and predictors of the development of HFpEF. Conversely, if the arrhythmia is not already present, most people with HFpEF are destined to develop it [48]. Both conditions are associated with a progressive left atrial myopathy driven by the presence of common cardiovascular risk factors [20]. The coexistence of AF and HFpEF is often underestimated in clinical practice, presumably because unrecognized AF occurs years before patients receive a diagnosis, and patients suffer from exertional dyspnea before physicians detect the presence of heart failure. The diagnosis of HFpEF on the basis of natriuretic peptides is very limited or even impossible in AF patients with suspected HFpEF [44].
Studies showing an exceptionally high prevalence of HFpEF in patients with AF, exertional dyspnea, and a normal ejection fraction support these associations. Reddy et al. showed that when patients with exertional dyspnea underwent exercise right heart catheterization, up to 64% suffered from occult HFpEF (pulmonary capillary wedge pressure of ≥ 25 mm Hg on exertion; [31]). To determine the impact of AF ablation on these patients the STALL AF-HFpEF trial (Study Using Invasive Hemodynamic Measurements Following Catheter Ablation for AF and Early HFpEF) evaluated 54 patients referred for catheter ablation for AF (with or without dyspnea on exertion; [39]).
Overall, 65% of these patients met diagnostic criteria for HFpEF in invasive measurements (pulmonary capillary wedge pressure of ≥ 25 mm Hg during exercise) and 92% of those with persistent AF fulfilled diagnostic criteria for HFpEF. After a follow-up of 12 months, nine patients (45%) who underwent ablation showed significant improvement in pulmonary wedge pressure and quality of life. Both studies showed a high rate of undetected HFpEF as an exceptionally common disorder in patients with AF who present with exertional dyspnea.
Treatment strategies for AF mainly differentiate between rate or rhythm control. Pharmacological rate control in HFpEF patients is difficult, treatment options are limited, and many antiarrhythmic drugs are contraindicated or poorly tolerated due to extracardiac side effects and high discontinuation rate (e.g. amiodarone).
The AFFIRM (Atrial Fibrillation Follow-Up Investigation of Rhythm Management) trial showed that if antiarrhythmic drugs (beta-blockers, calcium channel blockers, digoxin, or a combination of these medications) only were used, rate control equaled rhythm control in longer-term follow-up regarding outcomes such as mortality and stroke in patients with HFrEF. Furthermore, the stroke rate in the rhythm control arm was very high, mostly due to (inadequate) termination of oral anticoagulation [10]. These results sparked interest in rhythm control by AF ablation and prompted investigators to study the safety and practicality of AF ablation in heart failure patients. The focus of AF rhythm control therapy shifted toward catheter ablation. Several trials showed that catheter ablation improves clinical outcomes in AF patients with HFrEF [19, 22, 45]. However, the role of catheter ablation in HFpEF is less clear and data on the role of atrial fibrillation ablation in HFpEF are currently sparse.
The CABANA trial (Catheter Ablation vs. Antiarrhythmic Drug Therapy for Atrial Fibrillation) randomized patients with AF to either pulmonary vein isolation or antiarrhythmic drugs (rate or rhythm control). Only 9.3% of the patients had an LVEF < 40% and the median LVEF was 55%, implying a population with HFpEF rather than a population with HFrEF. Pulmonary vein isolation was not superior to drug therapy for cardiovascular outcomes at 5 years [27].
Yamauchi et al. showed in a large observational study of nearly 300 randomized patients with HFpEF, that these patients had similar ablation outcomes to HFrEF patients and patients without heart failure, although a majority of patients suffered from recent-onset or paroxysmal AF [46].
Similar to this observational study, a meta-analysis published in 2021 showed no significant differences in rates of AF recurrence 1 year after catheter ablation as well as improvements in New York Heart Association functional class and symptoms in AF-dedicated quality-of-life scores between patients with HFpEF and those with HFrEF [1].
The current ESC guidelines on heart failure treatment recommend the prudent use of AF catheter ablation (class IIa), and there is no difference between the recommendations for patients with HFpEF and HFrEF [23].
Further randomized clinical trials evaluating the clinical outcomes of catheter ablation and rhythm control therapy in AF patients with HFpEF are needed. In any such trial, a sham-controlled comparator should be used.
Arterial hypertension
The most common comorbidity in HFpEF patients is hypertension, which can be diagnosed in approximately 75% of HFpEF patients. Several studies investigated the impact of blood pressure control on outcomes in hypertensive patients with HFpEF. Tsujimoto et al. analyzed data from the TOPCAT study of 3417 HFpEF patients. Low systolic blood pressure in HFpEF patients was found to be an independent predictor of short- and long-term mortality in this population. In patients with mild hypertension, systolic blood pressure between 120 and 130 mm Hg and diastolic blood pressure between 70 and 80 mm Hg were associated with the lowest all-cause mortality [42]. Arterial hypertension affects myocardial remodeling and dysfunction in HFpEF patients through myocardial overload and systemic inflammation [6, 32]. Furthermore, hypertension causes activation of the renin–angiotensin–aldosterone system and sympathetic nervous system with increased catecholamine release, which leads to down-regulation of beta receptors, an increase in afterload, and thus further worsening of heart failure. Diuretics, spironolactone, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers, based on currently available data, are therefore the first choice, along with nonpharmacological agents, to control blood pressure as the main prevention and treatment strategy in HFpEF patients [28]. In a 2018 meta-analysis of 11 large, randomized trials of beta-blocker therapy across the heart failure spectrum, there were no benefits in reducing cardiovascular morbidity and mortality in a small subcohort with HFpEF and sinus rhythm [8]. In the ELANDD trial, nebivolol failed to positively affect heart failure symptoms in HFpEF. It was shown that peak oxygen uptake (peak VO2) decreased slightly in the nebivolol group, and increased in the placebo group, without reaching statistical significance. Resting and peak blood pressure, as well as systolic blood pressure, decreased significantly from baseline in the nebivolol group, without a change in the placebo arm [9]. Therefore, beta-blocker therapy cannot be recommended in HFpEF patients unless there are other reasons for this therapy, such as coronary artery disease.
Coronary artery disease
Coronary artery disease (CAD) is a common concomitant disease, detectable in more than 50% of HFpEF patients [26]. When considering the prognosis of CAD, significant differences are seen in HFpEF patients compared with HFrEF patients. The risk of cardiovascular death, as well as the incidence of sudden death, is significantly higher in HFpEF patients with CAD compared with HFrEF patients with CAD [34]. Stenosing coronary arteries cause a reduction in coronary flow reserve as well as oxygen supply in the myocardium, leading to a decrease in diastolic functional reserve. Furthermore, structural remodeling with compensatory hypertrophy, scarring, and impaired relaxation occurs as a result of myocardial infarction. Observational data from HFpEF patients with CAD suggest that complete revascularization is associated with better preservation of left ventricular systolic function and improved prognosis [16]. International guidelines consistently recommend that patients with chronic heart failure and CAD be treated analogously to patients with CAD without heart failure. The treatment and prevention of ischemia and coronary events should be the primary focus [30, 47].
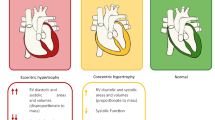
Coronary microvascular dysfunction
Coronary microvascular dysfunction (CMD) is discussed as a novel mechanism underlying the pathogenesis of HFpEF (Fig. 3; [35]). It has been hypothesized that comorbidities associated with HFpEF lead to systemic as well as to coronary endothelial inflammation and CMD, which reduce endothelial nitric oxide bioavailability and cyclic guanosine monophosphate production by adjacent cardiomyocytes. This process leads to downstream titin hypophosphorylation and increased cardiomyocyte stiffness and hypertrophy, myofibroblast activation, and interstitial fibrosis. Both cardiomyocyte and extracellular mechanisms lead to increased left ventricular diastolic stiffening, a well-known feature of HFpEF syndrome [36]. The role of CMD is not yet fully explained but may contribute to the development of new therapeutic strategies for patients with HFpEF.
Systemic and myocardial signaling in heart failure with preserved ejection fraction. cGMP cyclic guanosine monophosphate, CRP C-reactive protein, DM diabetes mellitus, GDF15 growth differentiation factor-15, IL1RL1 interleukin 1 receptor-like 1, NO nitric oxide, ONOO− peroxynitrite, PKG protein kinase G, ROS reactive oxygen species, sGC soluble guanylate cyclase, TGF transforming growth factor, VCAM vascular cellular adhesion molecule. With permission from [35]
Renal dysfunction
Renal dysfunction is also a common comorbidity in HFpEF patients. Over 20–30% of patients with HFpEF have chronic kidney failure. Heart failure and renal dysfunction influence each other, with cardiovascular risk and mortality increasing with decreasing renal function [29, 40]. Renal blood flow and sodium excretion are reduced by increased central venous pressure resulting from pulmonary hypertension and right ventricular dysfunction. Renal dysfunction, in turn, promotes HFpEF by worsening systemic inflammation and endothelial dysfunction, due in part to renal mediators such as high levels of fibroblast growth factors or uremic toxins [35]. The concomitant cardiac and renal insufficiency in patients poses several clinical challenges, as many established heart failure medications can cause worsening renal function or are contraindicated in the presence of renal insufficiency. Clinical experience shows that there are often mild fluctuations in renal function in patients with chronic heart failure, but an increase in serum creatinine above 30% of the baseline is usually not exceeded. In acute worsening of renal function, dose reduction or discontinuation of renin–angiotensin–aldosterone system inhibitors and diuretics in the presence of dehydration is recommended in current guidelines. Close monitoring of electrolyte balance and renal function is required. Basic drug therapy with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, beta receptor blockers, and mineralocorticoid receptor antagonist is recommended, taking contraindications into account and with careful titration or adjustment of the dosage.
Type 2 diabetes
Type 2 diabetes (T2D) is a high-risk factor in patients with HFpEF and plays a significant role in diastolic dysfunction. Approximately one third of HFpEF patients have concomitant diabetes mellitus [29]. Furthermore, T2D has been described as a comorbidity with a high risk of mortality and hospitalization [21]. Diabetes mellitus causes functional, morphologic, and biochemical changes in the myocardium that can lead to diastolic dysfunction and heart failure independent of other cardiovascular risk factors [14]. Intensified glycemic control, as shown in numerous studies, did not have a positive effect on cardiovascular mortality or hospitalization for heart failure, but instead increased susceptibility to hypoglycemia [7]. Current guidelines for the treatment of T2D recommend HbA1c levels in the range of 7%, and the treatment goal regarding HbA1c levels should be adjusted considering certain factors, such as age, comorbidities, hypoglycemia risk, and diabetes duration. Sodium-dependent glucose co-transporter 2 inhibitors are currently profiled as a therapeutic option to improve prognosis in heart failure patients with and without T2D.
The EMPEROR-Preserved study, a multicenter, double-blind, phase III trial enrolled 5988 symptomatic HFpEF patients (LVEF over 40%), both with and without T2D, across 23 countries. Participants were randomized in a 1:1 ratio to receive either 10 mg empagliflozin or placebo once daily, in addition to standard-of-care therapies. Over a median follow-up of 26.2 months, 13.8% of empagliflozin-treated patients and 17.1% of placebo-treated patients experienced a primary outcome event, equating to a hazard ratio of 0.79 (p < 0.001). This effect was observed across subgroups, including patients with and without T2D, as well as patients with an LVEF of less than 50%, 50–60%, or 60% and more. The trial results confirm that empagliflozin reduced the risk of a composite of cardiovascular death or hospitalization for heart failure in both diabetic and non-diabetic patients with HFpEF compared to placebo [2]. Another multicenter, international, double-blind, phase III trial, the DELIVER study, evaluating the efficacy of dapagliflozin in HFpEF patients compared to placebo, has already started. The first results from the DELIVER trial showed that dapagliflozin reached a statistically significant reduction in the primary composite endpoint of cardiovascular death or worsening heart failure. The full results are currently expected in the next few months [4, 37, 38].
Sleep apnea
Another very common comorbidity of heart failure is sleep apnea, which occurs in approximately 48% of HFpEF patients. A distinction must be made between obstructive (OSA) and central sleep apnea (CSA). Both OSA and CSA are associated with increased mortality in HFpEF patients [3]. Therefore, heart failure patients should always be monitored for corresponding symptoms such as daytime sleepiness, nocturnal breathing pauses, tendency to fall asleep, etc. In the case of abnormalities, further diagnostics should be initiated. Differentiation between OSA and CSA using polysomnography is important for appropriate therapy. In HFpEF patients, the proportion of patients with OSA predominates. A central role in OSA is the treatment of known triggering factors, such as obesity or excessive alcohol consumption. Furthermore, discontinuation or reduction of triggering medications such as opiates should be discussed. Often, CSA is caused by heart failure as the underlying disease and can be improved by optimal heart failure therapy.
Skeletal muscle, oxygen utilization, and physical activity
Several studies indicate that peak VO2 is significantly reduced in HFpEF patients. These patients exhibit abnormalities in skeletal muscle mass, composition, capillary density, and oxidative metabolism. Haykowsky et al. showed that elderly HFpEF patients have significantly reduced lean body mass and lean leg mass on a percentage basis compared with age-matched healthy patients. When peak VO2 was indexed to total lean body mass or lean leg mass, peak VO2 remained significantly reduced [13]. Thus, HFpEF patients have abnormal oxygen utilization that is independent of, and in addition to, their reduced muscle mass. Furthermore, HFpEF patients showed abnormal skeletal muscle composition with infiltration of adipose tissue, which is directly related to their reduced maximal oxygen uptake.
Endurance training leads to improved exercise capacity in HFpEF patients primarily by improving mitochondrial skeletal muscle mass and function. On the other hand, high-intensity and strength training have not yet been systematically studied.
Reduced lymphatic reserve
Microvascular dysfunction plays an important role in the pathogenesis of HFpEF (Fig. 4). In patients with HFpEF, peripheral lymphatics show structural and molecular alterations. In a 2020 study by Rossitto et al. with 32 patients, these morphological and functional alterations in the lymphatic vasculature were demonstrated in HFpEF patients, leading to decreased clearance of extravascular fluid and thus higher interstitial fluid accumulation. A better understanding of these mechanisms may provide a new pharmacological target for HFpEF treatment [33].
Microvascular fluid dynamics and reduced lymphatic reserve in heart failure with preserved ejection fraction (HFpEF). BV blood vasculature, LV lymphatic vasculature. With permission from [33] under the terms of the Creative Commons CC-BY license
Further comorbidities
Other comorbidities such as anemia, depression, obesity, hyperlipidemia, chronic obstructive pulmonary disease, sarcopenia, and pulmonary hypertension should be mentioned in this context. These are independent risk factors for the development of heart failure and are frequently found in heart failure patients.
Conclusion
The complex clinical picture of heart failure with preserved ejection fraction (HFpEF) remains challenging in the absence of evidence-based therapy. Except for comorbidity-specific guidelines, no HFpEF-specific treatment of comorbidities can be recommended at this time. Optimized care, especially for heart failure patients, is becoming increasingly relevant to reducing hospitalizations through a seamless inpatient and outpatient care structure. Current treatment is focused on symptom relief and management of associated comorbidities. Therefore, prevention through early minimization of risk factors currently remains the best approach. Further studies and new scientific knowledge are needed that will contribute to a better understanding of this complex syndrome.
References
Aldaas OM et al (2021) Meta-analysis of the usefulness of catheter ablation of atrial fibrillation in patients with heart failure with preserved ejection fraction. Am J Cardiol 142:66–73
Anker SD et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 385(16):1451–1461
Arzt M et al (2016) Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC Heart Fail 4(2):116–125
AstraZeneca (2022) FARXIGA met primary endpoint in DELIVER Phase III trial, reducing risk of cardiovascular death or worsening heart failure in patients with preserved ejection fraction. https://www.astrazeneca-us.com/content/az-us/media/press-releases/2022/farxiga-met-primary-endpoint-in-deliver-phase-III-trial.html. Accessed 5 May 2022
Benjamin EJ et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139(10):e56–e528
Borlaug BA et al (2015) Effects of sildenafil on ventricular and vascular function in heart failure with preserved ejection fraction. Circ Heart Fail 8(3):533–541
Boussageon R et al (2011) Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 343:d4169
Cleland JGF et al (2018) Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur Heart J 39(1):26–35
Conraads VM et al (2012) Effects of the long-term administration of nebivolol on the clinical symptoms, exercise capacity, and left ventricular function of patients with diastolic dysfunction: results of the ELANDD study. Eur J Heart Fail 14(2):219–225
Corley SD et al (2004) Relationships between sinus rhythm, treatment, and survival in the atrial fibrillation follow-up investigation of rhythm management (AFFIRM) study. Circulation 109(12):1509–1513
Dörr M et al (2021) Hospitalizations for heart failure: still major differences between East and West Germany 30 years after reunification. ESC Heart Fail 8(4):2546–2555
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602
Haykowsky MJ et al (2014) Skeletal muscle composition and its relation to exercise intolerance in older patients with heart failure and preserved ejection fraction. Am J Cardiol 113(7):1211–1216
van Heerebeek L, Somsen A, Paulus WJ (2009) The failing diabetic heart: focus on diastolic left ventricular dysfunction. Curr Diab Rep 9(1):79–86
Hindricks G et al (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42(5):373–498
Hwang SJ, Melenovsky V, Borlaug BA (2014) Implications of coronary artery disease in heart failure with preserved ejection fraction. J Am Coll Cardiol 63(25 Pt A):2817–2827
Iorio A et al (2018) Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: a community-based study. Eur J Heart Fail 20(9):1257–1266
Javed S et al (2021) Catheter ablation for atrial fibrillation in heart failure: untying the Gordian knot. J Geriatr Cardiol 18(4):297–306
Kirchhof P et al (2020) Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 383(14):1305–1316
Kotecha D et al (2016) Heart failure with preserved ejection fraction and atrial fibrillation: vicious twins. J Am Coll Cardiol 68(20):2217–2228
MacDonald MR et al (2008) Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J 29(11):1377–1385
Marrouche NF, Kheirkhahan M, Brachmann J (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 379(5):492
McDonagh TA et al (2021) Corrigendum to: 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 42(48):4901
McDonagh TA et al (2022) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 24(1):4–131
Mosterd A, Hoes AW (2007) Clinical epidemiology of heart failure. Heart 93(9):1137–1146
Owan TE et al (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355(3):251–259
Packer DL et al (2021) Ablation versus drug therapy for atrial fibrillation in heart failure: results from the CABANA trial. Circulation 143(14):1377–1390
Paulus WJ, van Ballegoij JJ (2010) Treatment of heart failure with normal ejection fraction: an inconvenient truth! J Am Coll Cardiol 55(6):526–537
Pfeffer MA, Shah AM, Borlaug BA (2019) Heart failure with preserved ejection fraction in perspective. Circ Res 124(11):1598–1617
Ponikowski P et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol (Engl Ed) 69(12):1167
Reddy YNV et al (2018) High prevalence of occult heart failure with preserved ejection fraction among patients with atrial fibrillation and dyspnea. Circulation 137(5):534–535
Rodriguez-Iturbe B et al (2014) The immunological basis of hypertension. Am J Hypertens 27(11):1327–1337
Rossitto G et al (2020) Reduced lymphatic reserve in heart failure with preserved ejection fraction. J Am Coll Cardiol 76(24):2817–2829
Rusinaru D et al (2014) Coronary artery disease and 10-year outcome after hospital admission for heart failure with preserved and with reduced ejection fraction. Eur J Heart Fail 16(9):967–976
Shah SJ et al (2016) Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation 134(1):73–90
Shah SJ et al (2018) Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J 39(37):3439–3450
Solomon SD et al (2021) Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial. Eur J Heart Fail 23(7):1217–1225
Solomon SD et al (2022) Baseline characteristics of patients with HF with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail 10(3):184–197
Sugumar H et al (2021) A prospective STudy using invAsive haemodynamic measurements foLLowing catheter ablation for AF and early HFpEF: STALL AF-HFpEF. Eur J Heart Fail 23(5):785–796
Ter Maaten JM et al (2016) Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail 18(6):588–598
Triposkiadis F et al (2016) Reframing the association and significance of co-morbidities in heart failure. Eur J Heart Fail 18(7):744–758
Tsujimoto T, Kajio H (2018) Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol 263:69–74
Vasan RS et al (2018) Epidemiology of left ventricular systolic dysfunction and heart failure in the Framingham study: an echocardiographic study over 3 decades. JACC Cardiovasc Imaging 11(1):1–11
Werhahn SM et al (2022) NT-proBNP as a marker for atrial fibrillation and heart failure in four observational outpatient trials. ESC Heart Fail 9(1):100–109
Willems S et al (2019) Cabins, castles, and constant hearts: rhythm control therapy in patients with atrial fibrillation. Eur Heart J 40(46):3793–3799c
Yamauchi R et al (2021) Catheter ablation for non-paroxysmal atrial fibrillation accompanied by heart failure with preserved ejection fraction: feasibility and benefits in functions and B‑type natriuretic peptide. Europace 23(8):1252–1261
Yancy CW et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16):e147–e239
Zakeri R et al (2013) Temporal relationship and prognostic significance of atrial fibrillation in heart failure patients with preserved ejection fraction: a community-based study. Circulation 128(10):1085–1093
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Deichl, R. Wachter and F. Edelmann declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deichl, A., Wachter, R. & Edelmann, F. Comorbidities in heart failure with preserved ejection fraction. Herz 47, 301–307 (2022). https://doi.org/10.1007/s00059-022-05123-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-022-05123-9