Abstract
Background
Left ventricular inferoseptal clefts are a localized variant of myocardial structure, easily overlooked but potentially raising concern when identified through imaging.
Case study
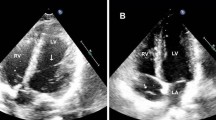
Here we illustrate and describe inferoseptal clefts by means of multimodality imaging and consider them in relation to possible differential diagnoses. A 49-year-old male patient was investigated for chest pain and found to have multiple inferoseptal clefts. The pain subsequently resolved and was thought to have been pleuritic. There was no evidence or family history of hypertrophic cardiomyopathy. The diagnosis of clefts was arrived at after consultation with several cardiac imaging specialists and the few available relevant published reports. Echocardiography, cardiovascular magnetic resonance, invasive ventriculography and computed tomography each showed the clefts in relation to surrounding compact and contractile myocardium of the inferoseptal region, which occluded the clefts in systole. In terms of location, orientation and systolic occlusion the inferoseptal clefts resembled the isolated clefts reported in healthy volunteers, and have features in common with crypts reported in carriers of a genetic mutation associated with hypertrophic cardiomyopathy (HCM). The incidence and implications of multiple inferoseptal clefts have yet to be determined.
Conclusion
Multimodality imaging permits clear depiction of left ventricular inferoseptal clefts, which should be distinguished from different entities such as left ventricular noncompaction cardiomyopathy (LVNC), cardiac diverticula and cardiac aneurysms. Inferoseptal clefts have yet to be widely recognized as a distinct variant of regional left ventricular structure.
Zusammenfassung
Hintergrund
Multiple inferoseptale linksventrikuläre Clefts sind seltene myokardiale Strukturveränderungen. Die Kenntnis dieser Strukturvariante ist Voraussetzung einer präzisen differenzialdiagnostischen Abgrenzung gegenüber der linksventrikulären Noncompaction-Kardiomyopathie (LVNC) sowie gegenüber linksventrikulären Divertikeln und Aneurysmen. In der begrenzt verfügbaren Literatur wurden bislang einzelne oder paarige Clefts beschrieben.
Fallbericht
Berichtet wird über einen Fall eines 49-jährigen männlichen Patienten, der sich aufgrund akuter Thoraxschmerzen bei Vorliegen koronarer Risikofaktoren einer Herzkatheteruntersuchung unterzog mit dem Nachweis multipler inferoseptaler myokardialer Strukturveränderungen sowie einer Koronarsklerose. Die initiale Vermutung einer atypischen LVNC wurde nach Einsatz multimodaler Bildgebung mit Kontrastmittelechokardiographie (KM-Echo), Herzmagnetresonanztomographie (Kardio-MRT) sowie Herzcomputertomographie (Kardio-CT), Konsultation mehrerer Experten sowie Studium der Literatur revidiert zugunsten der Diagnose multipler inferoseptaler Clefts. Die Beschwerden des Patienten stellten sich im Verlauf als pleuritischer Genese dar. Inferoseptale Clefts sind diastolische myokardiale Spaltbildungen der linksventrikulären myokardialen Junktionsregion, die mittels einer schmalen myokardialen Schicht von dem rechten Ventrikel abgegrenzt sind. Die betroffene inferoseptale myokardiale Region zeigt im Bereich der zwischenliegenden myokardialen Bänder ein systolisches Kontraktionsverhalten mit Okklusion der Clefts und ähnelt den in der Literatur als Crypts beschriebenen Veränderungen, die bei Trägern einer genetischen HCM-Mutation (hypertrophische Kardiomyopathie) nachgewiesen wurden. Clefts wurden in einer Kardio-MRT-Beobachtung jedoch auch sowohl bei Gesunden wie auch bei einer Population unterschiedlicher Krankheitsentitäten (HCM, arterielle Hypertonie, Zustand nach operativer Therapie bei Fallot-Tetralogie bzw. Pulmonalklappenstenose) beschrieben.
Schlussfolgerung
Multimodales Imaging ermöglicht die präzise Diagnose multipler inferoseptaler Clefts. Zur besseren Einschätzung wird ein Überblick über die Literatur und die Differenzialdiagnose präsentiert. Bei genauer Kenntnis dieser myokardialen Strukturvariante kann eine kardiale Bildgebung ohne Strahlenbelastung (KM-Echo, Kardio-MRT) zur Diagnose ausreichend sein. Eine valide Diagnose ist erforderlich, um möglicherweise unnötige weitere diagnostische und therapeutische Schritte (Herzkatheteruntersuchung, Antikoagulation) zu vermeiden. Die Prävalenz dieser Strukturvariante sowie die Inzidenz klinischer Komplikationen sollten Gegenstand weiterer Untersuchungen bleiben.





Similar content being viewed by others
References
McCrohon JA, Richmond DR, Pennell DJ, Mohiaddin RH (2002) Images in cardiovascular medicine. Isolated noncompaction of the myocardium: a rarity or missed diagnosis? Circulation 106:e22–e23
Srichai MB, Hecht EM, Kim DC, Jacobs JE (2007) Ventricular diverticula on cardiac CT: more common than previously thought. AJR Am J Roentgenol 189:204–208
Germans T, Wilde AA, Dijkmans PA et al (2006) Structural abnormalities of the inferoseptal left ventricular wall detected by cardiac magnetic resonance imaging in carriers of hypertrophic cardiomyopathy mutations. J Am Coll Cardiol 48:2518–2523
Germans T, Dijkmans PA, Wilde AA et al (2007) Images in cardiovascular medicine. Prominent crypt formation in the inferoseptum of a hypertrophic cardiomyopathy mutation carrier mimics noncompaction cardiomyopathy. Circulation 115:e610–e611
Johansson B, Maceira AM, Babu-Narayan SV et al (2007) Clefts can be seen in the basal inferior wall of the left ventricle and the interventricular septum in healthy volunteers as well as patients by cardiovascular magnetic resonance. J Am Coll Cardiol 50:1294–1295
Maron MS (2009) The current and emerging role of cardiovascular magnetic resonance imaging in hypertrophic cardiomyopathy. J Cardiovasc Transl Res 2:415–425
Jenni R, Oechslin E, Schneider J et al (2001) Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart 86:666–671
Petersen SE, Selvanayagam JB, Wiesmann F et al (2005) Left ventricular non-compaction: insights from cardiovascular magnetic resonance imaging. J Am Coll Cardiol 46:101–105
Ohlow MA (2006) Congenital left ventricular aneurysms and diverticula: definition, pathophysiology, clinical relevance and treatment. Cardiology 106:63–72
Kuribayashi T, Roberts WC (1992) Myocardial disarray at junction of ventricular septum and left and right ventricular free walls in hypertrophic cardiomyopathy. Am J Cardiol 70:1333–1340
Okoye MI, Congdon DE, Mueller WF Jr (1985) Asymmetric septal hypertrophy of the heart. New findings concerning the possible etiology of sudden deaths in five males. Am J Forensic Med Pathol 6:105–124
Maron BJ, Lindberg J, Lesser JR (2010) Ventricular septal crypt in hypertrophic cardiomyopathy. Eur Heart J 31:1923
Cooper LT, Baughman KL, Feldman AM et al (2007) American Heart Association; American College of Cardiology; European Society of Cardiology. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation 116:2216–2233
Aquaro GD, Di Bella G, Strata E et al (2007) Cardiac magnetic resonance findings in isolated congenital left ventricular diverticuli. Int J Cardiovasc Imaging 23:43–47
Krasemann T, Gehrmann J, Fenge H et al (2001) Ventricular aneurysm or diverticulum? Clinical differential diagnosis. Pediatr Cardiol 22:409–411
Ohlow MA, Secknus MA, Geller JC et al (2009) Prevalence and outcome of congenital left ventricular aneurysms and diverticula in an adult population. Cardiology 112:287–293
Acknowledgement
The authors would like to thank Professor Raimund Erbel, MD (University of Essen, Germany) and Professor Waldemar Hort, MD (University of Duesseldorf, Germany) for their helpful advice and discussions.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wein, M., Wolf-Puetz, A., Niehues, R. et al. Multiple left ventricular inferoseptal clefts. Herz 36, 438–443 (2011). https://doi.org/10.1007/s00059-011-3424-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-011-3424-9
Keywords
- Left ventricular inferoseptal clefts (LVIC)
- Cardiac computed tomography angiography (CTA)
- Cardiac magnetic resonance imaging (CMR)
- Contrast enhanced echocardiography
- Multimodality cardiac imaging