Abstract
Purpose
Masticatory muscles are physically affected by several skeletal features. The muscle performance depends on muscle size, intrinsic strength, fiber direction, moment arm, and neuromuscular control. To date, for the masticatory apparatus, only a two-dimensional cephalometric method for assessing the mechanical advantage, which is a measure for the ratio of the output force to the input force in a system, is available. This study determined the reliability and errors of a three-dimensional (3D) mechanical advantage calculation for the masticatory system.
Methods
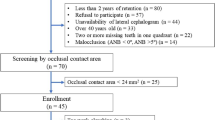
Using cone-beam computed tomography images from teenage patients undergoing orthodontic treatments, 36 craniofacial landmarks were identified, and the moment arms for seven muscles and their load moment arms (biomechanical variables) were determined. The 3D mechanical advantage for each muscle was calculated. This procedure was repeated by three examiners. Reliability was verified using the intraclass correlation coefficient (ICC) and the errors by calculating the absolute differences, variance estimator and coefficient of variation (CV).
Results
Landmark coordinates demonstrated excellent intra- and interexaminer reliability (ICC 0.998–1.000; p < 0.0001). Intraexaminer data showed errors < 1.5 mm. Unsatisfactory interexaminer errors ranged from 1.51–5.83 mm. All biomechanical variables presented excellent intraexaminer reliability (ICC 0.919–1.000, p < 0.0001; CV < 7%). Interexaminer results were almost excellent, but with lower values (ICC 0.750–1.000, p < 0.0001; CV < 10%). However, the muscle moment arm and 3D mechanical advantage of the lateral pterygoid muscles had ICCs < 0.500 (p < 0.05) and CV < 30%. Intra- and interexaminer errors were ≤ 0.01 and ≤ 0.05, respectively.
Conclusions
Both landmarks and biomechanical variables showed high reliability and acceptable errors. The proposed method is viable for the 3D mechanical advantage measure.
Zusammenfassung
Zielsetzung
Die Kaumuskulatur wird körperlich von mehreren Skelettmerkmalen beeinflusst. Die Muskelleistung hängt ab von der Muskelgröße, der intrinsischen Kraft, der Richtung der Muskelfasern, dem Impulsarm und der neuromuskulären Kontrolle. Bisher gibt es für den Kauorganapparat nur eine zweidimensionale kephalometrische Methode zur Beurteilung des mechanischen Vorteils, der ein Maß für das Verhältnis von Ausgangskraft zu Eingangskraft in einem System ist. In der vorliegenden Untersuchung wurden die Zuverlässigkeit und die Fehler einer dreidimensionalen (3-D) Berechnung des mechanischen Vorteils für den Kauapparat ermittelt.
Methoden
Anhand von digitalen Volumentomographie-Aufnahmen jugendlicher Kieferorthopädie-Patienten wurden 36 kraniofaziale Orientierungspunkte identifiziert und die Momentenarme für 7 Muskeln und ihre Lastmomentarme (biomechanische Variablen) bestimmt. Der mechanische 3‑D-Vorteil für jeden Muskel wurde berechnet. Dieses Verfahren wurde von 3 Untersuchern wiederholt. Die Zuverlässigkeit wurde anhand des Intraklassen-Korrelationskoeffizienten (ICC) überprüft, die Fehler durch Berechnung der absoluten Differenzen, des Varianzschätzers und des Variationskoeffizienten (CV).
Ergebnisse
Die Koordinaten der Referenzpunkte wiesen eine ausgezeichnete Intra- und Inter-Untersucher-Reliabilität auf (ICC 0,998–1,000; p < 0,0001). Die Intra-Untersucher-Daten zeigten Fehler < 1,5 mm. Unbefriedigende Inter-Untersucher-Fehler reichten von 1,51‑5,83 mm. Alle biomechanischen Variablen wiesen eine ausgezeichnete Intra-Untersucher-Reliabilität auf (ICC 0,919–1,000, p < 0,0001; CV < 7%). Die Inter-Untersucher-Ergebnisse waren fast hervorragend, jedoch mit niedrigeren Werten (ICC 0,750–1,000, p < 0,0001; CV < 10%). Der Drehmomentarm des Muskels und der mechanische 3‑D-Vorteil der seitlichen Pterygoidmuskeln wiesen jedoch ICCs < 0,500 (p < 0,05) und CV < 30% auf. Intra- und Inter-Untersucher-Fehler waren ≤ 0,01 bzw. ≤ 0,05.
Schlussfolgerungen
Sowohl die Referenzpunkte als auch die biomechanischen Variablen zeigten eine hohe Reliabilität und akzeptable Fehler. Die hier vorgeschlagene Methode ist für die Messung des mechanischen 3‑D-Vorteils geeignet.




Similar content being viewed by others
References
Hamill J, Knutzen KM, Derrick TR (2014) Biomechanical basis of human movement, 4th edn. Wolters Kluwer Health Adis, Philadelphia
Throckmorton GS, Finn RA, Bell WH (1980) Biomechanics of differences in lower facial height. Am J Orthod 77:410–420. https://doi.org/10.1016/0002-9416(80)90106-2
Throckmorton GS, Dean JS (1994) The relationship between jaw-muscle mechanical advantage and activity levels during isometric bites in humans. Arch Oral Biol 39:429–437. https://doi.org/10.1016/0003-9969(94)90174-0
García-Morales P, Buschang PH, Throckmorton GS, English JD (2003) Maximum bite force, muscle efficiency and mechanical advantage in children with vertical growth patterns. Eur J Orthod 25:265–272. https://doi.org/10.1093/ejo/25.3.265
Charalampidou M, Kjellberg H, Georgiakaki I, Kiliaridis S (2008) Masseter muscle thickness and mechanical advantage in relation to vertical craniofacial morphology in children. Acta Odontol Scand 66:23–30. https://doi.org/10.1080/00016350701884604
van Spronsen PH (2010) Long-face craniofacial morphology: cause or effect of weak masticatory musculature? Semin Orthod 16:99–117. https://doi.org/10.1053/j.sodo.2010.02.001
Sagl B, Schmid-Schwap M, Piehslinger E et al (2019) A dynamic jaw model with a finite-element temporomandibular joint. Front Physiol 10:1–12. https://doi.org/10.3389/fphys.2019.01156
Thomas GP, Throckmorton GS, Ellis E, Sinn DP (1995) The effects of orthodontic treatment on isometric bite forces and mandibular motion in patients before orthognathic surgery. J Oral Maxillofac Surg 53:673–678. https://doi.org/10.1016/0278-2391(95)90168-X
Lagravère MO, Gordon JM, Guedes IH et al (2009) Reliability of traditional cephalometric landmarks as seen in three-dimensional analysis in maxillary expansion treatments. Angle Orthod 79:1047–1056. https://doi.org/10.2319/010509-10R.1
Dicker GJ, Koolstra JH, Castelijns JA et al (2012) Positional changes of the masseter and medial pterygoid muscles after surgical mandibular advancement procedures: An MRI study. Int J Oral Maxillofac Surg 41:922–929. https://doi.org/10.1016/j.ijom.2012.01.007
Dicker GJ, Tuijt M, Koolstra JH et al (2012) Static and dynamic loading of mandibular condyles and their positional changes after bilateral sagittal split advancement osteotomies. Int J Oral Maxillofac Surg 41:1131–1136. https://doi.org/10.1016/j.ijom.2012.03.013
O’Neil R, Kau CH (2021) Comparison of dental arch forms created from assessment of teeth, alveolar bone, and the overlying soft tissue. J Orofac Orthop. https://doi.org/10.1007/s00056-021-00282-6
Becht MP, Mah J, Martin C et al (2014) Évaluation De La Morphologie Du Muscle Masséter Dans Différents Types De Malocclusions En Utilisant La Tomographie Volumétrique À Faisceau Conique. Int Orthod 12:32–48. https://doi.org/10.1016/j.ortho.2013.12.003
Velásquez RL, Coro JC, Londoño A et al (2018) Three-dimensional morphological characterization of malocclusions with mandibular lateral displacement using cone-beam computed tomography. Cranio 36:143–155. https://doi.org/10.1080/08869634.2017.1300994
Luebbert J, Ghoneima A, Lagravère MO (2016) Skeletal and dental effects of rapid maxillary expansion assessed through three-dimensional imaging: a multicenter study. Int Orthod 14:15–31. https://doi.org/10.1016/j.ortho.2015.12.013
Draenert FG, Erbe C, Zenglein V et al (2010) 3D analysis of condylar position after sagittal split osteotomy of the mandible in mono- and bimaxillary orthognathic surgery—a methodology study in 18 patients. J Orofac Orthop 71:421–429. https://doi.org/10.1007/s00056-010-1021-9
Alhammadi MS, Elfeky HY, Fayed MS et al (2019) Three-dimensional skeletal and pharyngeal airway changes following therapy with functional appliances in growing skeletal Class II malocclusion patients. J Orofac Orthop 80:254–265. https://doi.org/10.1007/s00056-019-00185-7
Haskell B, Day M, Tetz J (1986) Computer-aided modeling in the assessment of the biomechanical determinants of diverse skeletal patterns. Am J Orthod 89:363–382. https://doi.org/10.1016/0002-9416(86)90068-0
Springate SD (2012) The effect of sample size and bias on the reliability of estimates of error: a comparative study of Dahlberg’s formula. Eur J Orthod 34:158–163. https://doi.org/10.1093/ejo/cjr010
Lagravère MO, Low C, Flores-Mir C et al (2010) Intraexaminer and interexaminer reliabilities of landmark identification on digitized lateral cephalograms and formatted 3‑dimensional cone-beam computerized tomography images. Am J Orthod Dentofac Orthop 137:598–604. https://doi.org/10.1016/j.ajodo.2008.07.018
Naji P, Alsufyani NA, Lagravère MO (2014) Reliability of anatomic structures as landmarks in three-dimensional cephalometric analysis using CBCT. Angle Orthod 84:762–772. https://doi.org/10.2319/090413-652.1
Zhang X, Ye L, Li H et al (2018) Surgical navigation improves reductions accuracy of unilateral complicated zygomaticomaxillary complex fractures: a randomized controlled trial. Sci Rep 8:1–9. https://doi.org/10.1038/s41598-018-25053-z
Coombs MC, Bonthius DJ, Nie X et al (2019) Effect of measurement technique on TMJ mandibular condyle and articular disc morphometry: CBCT, MRI, and physical measurements. J Oral Maxillofac Surg 77:42–53. https://doi.org/10.1016/j.joms.2018.06.175
Lagravère MO, Major PW (2005) Proposed reference point for 3‑dimensional cephalometric analysis with cone-beam computerized tomography. Am J Orthod Dentofac Orthop 128:657–660. https://doi.org/10.1016/j.ajodo.2005.07.003
Baron P, Debussy T (1979) A biomechanical functional analysis of the masticatory muscles in man. Arch Oral Biol 24:547–553. https://doi.org/10.1016/0003-9969(79)90134-1
Koolstra JH, van Eijden TMGJ, van Spronsen PH et al (1990) Computer-assisted estimation of lines of action of human masticatory muscles reconstructed in vivo by means of magnetic resonance imaging of parallel sections. Arch Oral Biol 35:549–556. https://doi.org/10.1016/0003-9969(90)90086-P
Van Eijden TMGJ, Korfage JAM, Brugman P (1997) Architecture of the human jaw-closing and jaw-opening muscles. Anat Rec 248:464–474
Tuijt M, Koolstra JH, Lobbezoo F, Naeije M (2010) Differences in loading of the temporomandibular joint during opening and closing of the jaw. J Biomech 43:1048–1054. https://doi.org/10.1016/j.jbiomech.2009.12.013
Nicolielo LFP, Van Dessel J, Shaheen E et al (2017) Validation of a novel imaging approach using multi-slice CT and cone-beam CT to follow-up on condylar remodeling after bimaxillary surgery. Int J Oral Sci 9:139–144. https://doi.org/10.1038/ijos.2017.22
Kim H‑Y (2013) Statistical notes for clinical researchers: Evaluation of measurement error 1: using intraclass correlation coefficients. Restor Dent Endod 38:98. https://doi.org/10.5395/rde.2013.38.2.98
Maspero C, Abate A, Bellincioni F et al (2019) Comparison of a tridimensional cephalometric analysis performed on 3T-MRI compared with CBCT: a pilot study in adults. Prog Orthod 20:40. https://doi.org/10.1186/s40510-019-0293-x
Bartlett JW, Frost C (2008) Reliability, repeatability and reproducibility: Analysis of measurement errors in continuous variables. Ultrasound Obstet Gynecol 31:466–475. https://doi.org/10.1002/uog.5256
Shechtman O (2013th) The coefficient of variation as an index of measurement reliability. In: Doi SAR, Williams GM (eds) Methods of clinical epidemiology. Springer, Heidelberg, New York, pp 39–49 https://doi.org/10.1007/978-3-642-37131-8_4
Throckmorton GS, Ellis E (2001) The relationship between surgical changes in dentofacial morphology and changes in maximum bite force. J Oral Maxillofac Surg 59:620–627. https://doi.org/10.1053/joms.2001.23373
Hannam AG, McMillan AS (1994) Internal organization in the human jaw muscles. Crit Rev Oral Biol Med 5:55–89. https://doi.org/10.1177/10454411940050010301
Castro IO, Gribel FB, de Alencar AHG et al (2018) Evaluation of crown inclination and angulation after orthodontic treatment using digital models. J Orofac Orthop 79:227–234. https://doi.org/10.1007/s00056-018-0136-2
Takeuchi-Sato T, Arima T, Mew M, Svensson P (2019) Relationships between craniofacial morphology and masticatory muscle activity during isometric contraction at different interocclusal distances. Arch Oral Biol 98:52–60. https://doi.org/10.1016/j.archoralbio.2018.10.030
Du W, Bhojwani A, Hu JK (2021) FACEts of mechanical regulation in the morphogenesis of craniofacial structures. Int J Oral Sci 13:1–16. https://doi.org/10.1038/s41368-020-00110-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Sánchez-Ayala, A. Sánchez-Ayala, R.C. Kolodzejezyk, V.M. Urban, M.Ó. Lagravère and N.H. Campanha declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. This work was approved by the Health Research Ethics Board at the University of Alberta (#5563). All subjects who participated in the study signed written informed consent to participate.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplemental video 1: Identification of the 36 craniofacial landmarks, and determination of the spatial reference planes, moment arms for seven muscles (superficial masseter, anterior and posterior deep masseter, anterior and posterior temporal, and medial and lateral pterygoid), and their corresponding load moment arms at the incisor and molar position
Rights and permissions
About this article
Cite this article
Sánchez-Ayala, A., Sánchez-Ayala, A., Kolodzejezyk, R.C. et al. A three-dimensional method to calculate mechanical advantage in mandibular function. J Orofac Orthop 84, 321–339 (2023). https://doi.org/10.1007/s00056-022-00378-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-022-00378-7