Abstract
Objective: To understand the diagnostic and short-term prognostic significance of electrocardiographic left ventricular hypertrophy (ECG-LVH) for patients who present to the emergency department with symptoms suggesting acute cardiac ischemia, defined as new or unstable angina pectoris or acute myocardial infarction.
Design: Subgroup analysis of a multicenter, prospective study of coronary care unit admitting practices in the prethrombolytic era.
Setting: The emergency departments of six New England hospitals: two urban medical school teaching hospitals, two medical school—affiliated community hospitals in smaller cities, and two rural nonteaching hospitals.
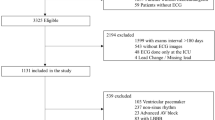
Patients: 5,768 patients presenting with symptoms suggesting possible acute cardiac ischemia, including 413 patients who had ECG-LVH defined by the Romhilt-Estes point score criteria and 5,355 patients who had other electrocardiogram (ECG) findings.
Main results: Only 26% of the 413 patients who had ECG-LVH were ultimately judged to have had acute cardiac ischemia, compared with 72% of patients who had primary ST-segment and T-wave abnormalities (p<0.001) and 36% of those who had other ECG abnormalities (p<0.001). Overall, the ECG-LVH patients were one-third less likely than the patients who did not have ECG-LVH to have had acute cardiac ischemia, after controlling for other predictors of acute ischemia by logistic regression (relative risk=0.66, 95% CI 0.46 to 0.94). The patients who had ECG-LVH were only one-fourth as likely to have had acute myocardial infarctions as were the patients presenting with primary ST-segment and T-wave changes (12% vs 48%, p<0.001). Instead, a much larger proportion had had congestive heart failure or hypertension. The admitting physicians had identified ECG-LVH poorly on the admitting ECGs: only 22% of those who had ECG-LVH had been correctly identified, and for more than 70%, the secondary ST-segment and T-wave changes of ECG-LVH had been read as being primary. The short-term mortality for the patients who had ECG-LVH was 7.5%. This was intermediate between the mortality for patients who had primary ST-segment and T-wave abnormalities (10.6%) and those who had other ECG abnormalities (5.1%). Mortality was not affected by whether the admitting physician had recognized ECG-LVH initially.
Conclusion: ECG-LVH was not a benign ECG finding among the patients who had presented with symptoms suggesting an acute cardiac ischemic syndrome: short-term mortality among the patients who had ECG-LVH (7.5%) approached that for the patients who had primary ST-segment and T-wave abnormalities (10.6%, p=0.10). However, the patients who had ECG-LVH were one-thirdless likely to have had any acute cardiac ischemia than were the patients who did not have ECG-LVH, after logistic regression was used to control for other predictors of acute ischemia. Specifically, acute myocardial infarction was only one-fourth as likely when LVH was present on the admitting ECG (12%) as it was when primary ST-segment and T-wave abnormalities were present (48%, p<0.001). Instead, congestive heart failure and hypertensive heart disease were more common. Thus, routine use of thrombolytic therapy for patients who have ECG-LVH does not seem warranted. ECG-LVH was poorly recognized (in only 22% of cases) by the physicians in the present study. Better recognition of this common ECG finding may lead to more effective patient management.
Similar content being viewed by others
References
Kannel WB, Gordon T, Offutt D. Left ventricular hypertrophy by electrocardiogram: prevalence, incidence, and mortality in the Framingham Study. Ann Intern Med. 1969;71:89–105.
Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary disease. Ann Intern Med. 1970;72:813–22.
Kannel WB, Dannenberg AL, Levy D. Population implications of electrocardiographic left ventricular hypertrophy. Am J Cardiol. 1987;60:851–931.
Pozen MW, D’Agostino RB, Selker HP, Sytkowski PA, Hood WB Jr. A predictive instrument to improve coronary-care-unit admission practices in acute ischemic heart disease. N Engl J Med. 1984;310:1273–8.
Van Der Does E, Lubsen J, Pool J, et al. Acute coronary events in a general practice: objectives and design of the imminent myocardial infarction Rotterdam Study. Heart Bull. 1976;7:91–8.
Romhilt DW, Estes EH Jr. A point score system for the ECG diagnosis of left ventricular hypertrophy. Am Heart J. 1968;75:752–8.
Prineas RJ, Crow R, Blackburn H. The Minnesota Code Manual of Electrocardiographic Findings. Littleton, MA: John Wright-PSG, 1982.
Dixon WJ (ed). BMDP Statistical Software. Berkeley, CA: University of California Press, 1985;330–44.
Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico (GISSI). Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986;1:397–401.
ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988;II:349–60.
Wilcox RG, von der Lippe G, Olsson CG, et al. Trial of tissue plasminogen activator for mortality reduction in acute myocardial infarction. Lancet. 1988;II:525–30.
Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949;37:161–86.
Casale PN, Devereux RB, Kligfield P, et al. Electrocardiographic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol. 1985;6:572–80.
Devereux RB, Casale PN, Eisenberg RR, Miller DH, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy using echocardiogram determination of left ventricular mass as the reference standard: comparison of standard criteria, computer diagnosis and physician interpretation. J Am Coll Cardiol. 1984;3:82–7.
Willems JL, Abreu-Lima C, Arnaud P, et al. The diagnosis performance of computer programs for the interpretation of electrocardiograms. N Engl J Med. 1991; 325:1767–73.
Jayes RL, Larsen GC, Beshansky JR, D’Agostino RB, Selker HP. Physician electrocardiogram reading in the emergency department—accuracy and effect on triage decisions. J Gen Intern Med. 1992;7:387–92.
Grines CL, DeMaria AN. Optimal utilization of thrombolytic therapy for acute myocardial infarction: concepts and controversies. J Am Coll Cardiol. 1990;16:223–31.
Surawicz B, Saito S. Exercise testing for detection of myocardial ischemia in patients with abnormal electrocardiograms at rest. Am J Cardiol. 1978;41:943–51.
Beach C, Kenmure ACF, Short D. Electrocardiogram of pure left ventricular hypertrophy and its differentiation from lateral ischemia. Br Heart J. 1981;46:385–9.
Author information
Authors and Affiliations
Additional information
Supported by grants R01-HS02068 and R01-HS05549 from the Agency for Health Care Policy and Research, and training grant LM7044 and research grant LM4493 from the National Library of Medicine Medical Information Program.
Rights and permissions
About this article
Cite this article
Larsen, G.C., Griffith, J.L., Beshansky, J.R. et al. Electrocardiographic left ventricular hypertrophy in patients with suspected acute cardiac ischemia—Its influence on diagnosis, triage, and short-term prognosis. J Gen Intern Med 9, 666–673 (1994). https://doi.org/10.1007/BF02599006
Issue Date:
DOI: https://doi.org/10.1007/BF02599006