Summary
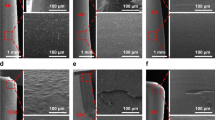
In an experimental comparative study on rabbits, the efficacy of the reduction of surface thrombus formation was investigated using heparinized central venous catheters compared with non-heparinized. Up to a central indwelling period of ten days, there was a reduction of the thrombus layer thickness on the heparinized catheters of 80% (with a trial duration of three days this was as much as 90%).
The action of the stabilized surface heparin, which leads to a substantial thromboresistance, is complex in nature. 1) By intensified adsorption of plasma proteins in the early phase (proteins consist of antithrombin III, factor IX, X and XI), there is very much less thrombocyte adhesion and aggregation on the heparinized catheter surfaces. 2) The externally orientated negative net charge of the heparin shows a similar effect. 3) If there is thrombocyte adhesion despite this, further heparin effects become more prominent. Thus the release of ThF 3 and ADP, which leads to aggregation, is markedly inhibited. On the one hand, this leads to easier dissolution of already aggregated thrombocytes and on the other to a reduction of the catalytic thrombocyte surface for the plasma clotting factors. 4) This effect is supported by the increased adsorption of antithrombin III onto the control surface. 5) Finally there is also an inhibitory effect of heparin on the activated Stuart-Prower factor.
Local thrombosis on the venous catheter surface can thus be effectively reduced by local therapy, without greater risks for the intensive care patient.
Similar content being viewed by others
References
Burri C, Gasser D (1971) Der Vena-Cava-Ketheter. Springer, Berlin-Heidelberg-New York
Burri C (1975) Der Katherismus der Vena Cava. Wissenschaftliche Schriftenreihe 8:23–60
Danishefsky I, Tzeng F (1974) Preparation of heparinlinked agarose and its interaction with plasma. Thromb Res 4:237–246
Deutsch E (1977) Haemorrhagische Diathesen. In: Gross R, Schölmerich P (eds) Lehrbuch der Inneren Medizin. Schattauer, Stuttgart pp 179–206
Eldh P, Jacobsson B (1974) Heparinized vascular catheters: A clinical trial. Radiology 11:289–292
Gofferje H (1977) Infusionstherapie heute. 14. Infusionstechnik. Med Welt 28:1152–1156
Haag R, Tiller FW, Opelt KH, Weidener D (1977) Bedeutung der bakteriellen Kontamination zentraler Venenkatheter für die Entstehung lokaler und allgemeiner infektiöser Komplikationen. Das Deutsche Gesundheitswesen 32:699–703
Jacobsson B, Schlossman D (1973) Thrombogenicity of heparinized vascular catheters. Acta Radiol [Ther] (Stockh) 14:569–576
Kurock W, Schier J (1974) Erfahrungen mit dem Vena-Cava-Katheter. Med Welt 25:135–138
Lagergren H, Olsson P, Swedenborg J (1974) Inhibited platelet adhesion: A non-thrombogenic characteristic of a heparin coated surface. Surgery 75:643–650
Larsson RL, Hjelte WB, Eriksson JC, Lagergren HR, Olsson P (1976) The stability of glutardial-dehyde-stabilized 35S-heparinized surfaces in contact with blood. Thromb Haemostas 37:262–273
Larsson R, Rosengren A, Olsson P (1977) Determination of platelet adhesion to polyethylene and heparinized surfaces with the aid of bioliuminescence and 51Chromium labelled platelets. Thromb Res 11:517–530
Lawin P (1975) Kava-Ketheter and Venae sectio. In: Praxis der Intensivbehandlung. Thieme, Stuttgart
Mlynek HJ, Klötzer B (1969) Erfahrungen mit Kava-Kathetern. Zentralbl Chir 94:486–491
Olsson P, Lagergren H, Larsson R, Radegran K (1977) Prevention of platelet adhesion and aggregation by a glutaraldehyde-stabilized heparin surface. Thromb Haemostas 37:274–282
Pilgerstorfer HW, Finkenstedt G, Kleinberger G, Kotzaurek R, Pall H, Pichier M, Raberger G, Szelless S (1973) Subclavia-Katheter im Rahmen der internistischen Intensivmedizin. Wien Klin Wochenschr 50:822–825
Sawyer PN, Pate JW (1953) Bioelectric phenomena as an etiologic factor in intravascular thrombosis. Am J Physiol 75:103–107
Schocke J (1973) Der Subclavia Katheter in der chirurgischen Intensivtherapie. Zentralbl Chir 98:270–273
Scholz G, Loewe KR (1969) Die Punktion der Vena subclavia und ihre Komplikationen aus pathologisch-anatomischer Sicht. Med Welt 20:2248–2251
Walker FJ, Esmon CT (1979) The molecular mechanisms of heparin action: II. Separation of functionally different heparins by affinity chromatography. Thromb Res 14:219–230
Walsh PN, Biggs R (1972) The role of platelets in intrinsic factor Xa formation. Br J Haematol 22:743–760
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Wenning, M., Höpker, WW. Scanning electron microscopic comparison between the thrombogenic properties of heparinized and non-heparinized vena Cava catheters. Virchows Arch. A Path. Anat. and Histol. 391, 207–215 (1981). https://doi.org/10.1007/BF00437597
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00437597