Abstract
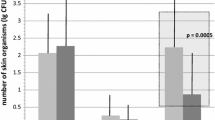
In order to study the distribution of bacteria in the operating room environment, cultures were obtained during 111 unselected shunt operations throughout a 10-month period. After routine skin preparation, bacteria were collected by placing Millipore filters on the patient's prepped skin underneath the drapes, on top of the drapes in the operative field, and/or on the sterile instrument table, and left in place for the duration of the case. In 48 patients, full-thickness skin biopsies taken at the initial incision were cultured in lieu of skin surface cultures. Perioperative cerebrospinal fluid cultures and subsequent shunt infections were monitored. Of the 288 environmental (skin and surfaces) cultures, 24 were positive (20 coagulase-negative Staphylococcus and 4 Staphylococcus aureus). Positive cultures were found in 15 of 111 drape cultures (13.5%), 7 of 77 instrument table cultures (9.1%), and 2 of 97 skin cultures (2.1%). Positive environmental cultures were not correlated with the surgeon, length of case, time of day, or type of shunt operation, but were more likely to occur in a room other than the designated neurosurgical operating room. There was a correlation between the occurrence of positive environmental cultures and positive cerebrospinal fluid cultures, although the organisms were not always the same. Coagulase-negative Staphylococcus was the most common organism isolated from all sites. We conclude that bacteria most often associated with shunt infections are airborne in the operating room, rather than originating from the patient's skin, and are distributed in the highest concentration near the surgical team. Maintaining a designated operating room in which traffic is limited, as well as strict adherence to covering skin surfaces of the operating room personnel, may help to reduce shunt infection rates.
Similar content being viewed by others
References
Bayston R (1975) Antibiotic prophylaxis in shunt surgery. Dev Med Child Neurol 17:99–103
Bayston R, Lari J (1974) A study of the sources of infection in colonised shunts. Dev Med Child Neurol 16:16–22
Conn J, Bornhoeft JW, Almgren C, Mucha DP, Olderman J, Patel K, Herring CM (1986) In vivo study of an antimicrobial surgical drape system. J Clin Microbiol 24:803–808
Henderson RJ (1967) Staphylococcal infection of surgical wounds: the source of infection. Br J Surg 54:756–760
James HE, Walsh JW, Wilson HD, Connor JD, Bean JR, Tibbs PA (1980) Prospective randomized study of therapy in cerebrospinal fluid shunt infections. Neurosurgery 7:459–463
McComb JG (1988) Comment. Neurosurgery 22:872
McLaurin RL (1973) Infected cerebrospinal fluid shunts. Surg Neurol 1:191–195
McLaurin RL, Frame PT, Wald SL (1981) Multiple antibiotic treatment for shunt infection. Concepts Pediatr Neurosurg 1:79–86
Renier D, Lacombe J, Peirre-Kahn A, Sainte-Rose C Hirsch J (1984) Factors causing acute shunt infection. Computer analysis of 1174 operations. J Neurosurg 61:1072–1078
Sampolinsky D, Hermann F, Oeding P, Rippon JE, (1957) A series of post-operative infections. J Infect Dis 100:1–11
Schmidt R, Gjerris F, Osgaard O, Hvidberg EF, Kristiansen JE, Dahlerup B, Kruse-Larsen C (1985) Antibiotic prophylaxis in cerebrospinal fluid shunting: a prospective randomized trial in 152 hydrocephalic patients. Neurosurgery 17:1–5
Schoenbaum SC, Gardner P, Shillito J (1975) Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis 131:543–552
Selwyn S, Ellis H (1972) Skin bacteria and skin disinfection reconsidered. Br Med J 1:136–140
Shapiro S, Boaz J, Kleiman M, Kalsbeck J, Mealey J (1988) Origin of organisms infecting ventricular shunts. Neurosurgery 22:868–872
Steinbok P, Thompson GB (1976) Complications of ventriculovascular shunts: computer analysis of etiologic factors. Surg Neurol 5:31–35
Sugarman B (1986) Infections and prosthetic devices. Am J Med 81:78–84
Venes JL (1979) Control of shunt infection Report of 150 consecutive cases. J Neurosurg 45:311–314
Walters BC, Hoffmann HJ, Hendrick EB, Humphreys RP (1984) Cerebrospinal fluid shunt infection. Influences on initial management and subsequent outcome. J Neurosurg 60:1014–1021
Wright RL (1966) A survey of possible etiologic agents in postoperative craniotomy infections. J Neurosurg 25:125–132
Young RF, Lawner PM (1987) Perioperative antibiotic prophylaxis for the prevention of postoperative neurosurgical infections: a randomized clinical trial. J Neurosurg 66:701–706
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Duhaime, AC., Bonner, K., McGowan, K.L. et al. Distribution of bacteria in the operating room environment and its relation to ventricular shunt infections: a prospective study. Child's Nerv Syst 7, 211–214 (1991). https://doi.org/10.1007/BF00249397
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF00249397