Abstract
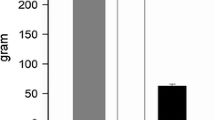
The effects on the sphincter of Oddi of intravenous administration of dipyrone, 2.5 g; tramadol, 50 mg; indomethacin, 75 mg;N-butylscopolamine, 20 mg; and nitroglycerin, 1 mg, in comparison to physiological saline were assessed in a single-blind study in 36 patients hospitalized with upper abdominal pain. Basal sphincter pressure and sphincter motility were measured for a 5-min period after treatment by endoscopic manometry. Nitroglycerin and dipyrone both caused a significant fall in basal sphincter pressure, whileN-butylscopolamine and nitroglycerin produced a significant decrease in contraction frequency. Therefore, dipyrone, in contrast to tramadol and indomethacin, exhibits spasmolytic activity in addition to analgesia in biliary pain.
Similar content being viewed by others
References
Eigler FW: Schmerz und akutes Abdomen.In Gastroenterologie. H Goebell (ed). Munich Urban & Schwarzenberg, 1992
Delmont J, Harris AG: Limitations of endoscopic manometry of the sphincter of Oddi.In New York, Raven Press, HJ Siegel (ed). Endoscopic Retrograde Pancreatography; 1992
Hogan WJ: Sphincter of Oddi human physiology; the manometric era. Ital J Gastroenterol 18:31–45, 1986
Staritz M, Poralla T, Ewe K, Meyer zum Büschenfelde KH: Effect of glyceryl trinitrate on sphincter of Oddi motility and baseline pressure. Gut 26:194, 1985
Brandstätter G: Pharmacological pressure reduction in the human common bile duct. Z Gastroenterol 21:168, 1983
Nowakowska-Dulawa E, Nowak A, Kaczor R: Effects of isosorbide dinitrate and Hymecromone on the motor activity of the sphincter of Oddi in man. World Congress of Gastroenterology, Sydney, 1990, p 160
Neugebauer V, Schaible HG: Electrophysiological evidence for a spinal antinociceptive action of dipyrone. Agents Actions 41:62–70, 1994
Mutschler E (ed): Arzneimittelwirkungen, 6. Auflage. Stuttgart, Wissenschaftliche Verlagsgesellschaft 1991
Remjan F: Intravenous indomethacin in biliary pain IRCS Med Sci 112:398–400, 1984
Corazziari E, Biliotti D: Sphincter of Oddi manometry. Gastroenterol Int 2:180–184, 1989
Nebel OT: Manometric evaluation of the papilla of Vater. Gastrointest Endosc 21:126–128, 1975
Staritz M, Meyer zum Büschenfelde KH: Investigation of the effect of diazepam and other drugs on the sphincter of Oddi motility. Ital J Gastroenterol 18:41, 1986
Ponce J, Garrigues V, Sala T, Pertejo V, Berenguer J: Diazepam does not modify the motility of the sphincter of Oddi. Endoscopy 20:87, 1988
Funch-Jensen P: Sphincter of Oddi motility. Acta Chir Scand Suppl 553, 1990
Allescher HD, Neuhaus H, Hagenmüller F, Classen M: Effect ofN-butylscopolamine on sphincter of Oddi motility in patients during routine ERCP—a manometric study. Endoscopy 20:73, 1988
Kaczor R, Nowakowska-Dulawa E, Rybicka J: Effects of Scopolamine butylbromide, papaverine and glucagon on the sphincter of Oddi motility. Endoscopy 20:73, 1988
Staritz M, Poralla T, Mann M, Meyer zum Büschenfelde KH: Effect of modern analgesic drugs (tramadol, pentazocine and buprenorphine) on the bile duct sphincter in man. Gut 27:567–569, 1986
Binmoeller KF, Dumas R, Harris AG, Delmont JP: Effect of somatostatin analog octreotide on human sphincter of Oddi. Dig Dis Sci 37(5):773–777, 1992
Cuer JC, Dapoigny M, Bommelaer G: The effect of midazolam on motility of the sphincter of Oddi in human subjects. Endoscopy 25:384–386, 1993
Biliotti D, Habib FI, De Masi E, Primerano L, Pallotta N, Corazziari E: Effect of glucagon on sphincter of Oddi motor activity. Digestion 43:185–189, 1989
Cuer JC, Dapoigny M, Ajmi S, Larpent JL, Lunaud B, Ferrier C, Bommelaer G: Effects of buprenorphine on motor activity of the sphincter of Oddi in man. Eur J Clin Pharmacol 36:203–204, 1989
Thune A, Saccone GTP, Scicchitano JP, Toouli J: Distension of the gall bladder inhibits Sphincter of Oddi motility in humans. Gut 32:690–693, 1991
Rolny P, Funch-Jensen P, Kruse A, Thommesen P: Effect of cholecystectomy on the relationship between hydrostatic common bile duct pressure and Sphincter of Oddi motility. Endoscopy 23:111–113, 1991
Guelrud M, Mendoza S, Rossiter G, Villegas MI: Sphincter of Oddi manometry in healthy volunteers. Dig Dis Sci 35(1):38–46, 1990
Games PA: An improvedt table for simultaneous control ong-contrasts. J Am Stat Assoc 72:531–534, 1977
Sidak Z: Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc 62:626–633, 1967
Author information
Authors and Affiliations
Additional information
This study was sponsored by Hoechst AG, Frankfurt/M., Germany
Rights and permissions
About this article
Cite this article
Brandstätter, G., Schinzel, S. & Wurzer, H. Influence of spasmolytic analgesics on motility of sphincter of oddi. Digest Dis Sci 41, 1814–1818 (1996). https://doi.org/10.1007/BF02088751
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02088751