Abstract
Dyslipidaemia is a major risk factor for cardiovascular diseases. Pharmacological lowering of LDL-C levels using statins reduces cardiovascular risk. However, a substantial residual risk persists especially in patients with type 2 diabetes mellitus. Because of the inverse association observed in epidemiological studies of HDL-C with the risk for cardiovascular diseases, novel therapeutic strategies to raise HDL-C levels or improve HDL functionality are developed as complementary therapy for cardiovascular diseases. However, until now most therapies targeting HDL-C levels failed in clinical trials because of side effects or absence of clinical benefits. This chapter will highlight the emerging small molecules currently developed and tested in clinical trials to pharmacologically modulate HDL-C and functionality including new CETP inhibitors (anacetrapib, evacetrapib), novel PPAR agonists (K-877, CER-002, DSP-8658, INT131 and GFT505), LXR agonists (ATI-111, LXR-623, XL-652) and RVX-208.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
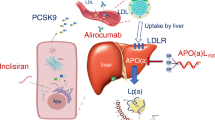
Dyslipidaemia is a major risk factor for cardiovascular diseases, a main cause of morbidity and mortality worldwide, with 17.3 million deaths per year (Laslett et al. 2012). LDL-C-lowering therapy, especially with statins, has shown to be an efficient approach to reduce cardiovascular risk on average by 25–35 %. Although lowering LDL-C with statins has beneficial effects and reduces cardiovascular events, significant numbers of residual cardiovascular events remain in high-risk patients, prompting the search for alternative complementary approaches. Among these strategies, new agents combined with statins, such as proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, microsomal triglyceride transfer protein (MTTP) inhibitors or ezetimibe can provide additional lowering LDL-C effects.
Because HDL-C levels are inversely correlated with cardiovascular risk (Gordon et al. 1977), raising HDL-C levels has spawned high hopes as additional therapy for cardiovascular diseases. However, so far none of the pharmacological interventions aimed at raising HDL-C levels has yielded convincing results with respect to reduction of cardiovascular risk.
In this chapter we will focus on these emerging small molecule drugs in development, including cholesteryl ester transfer protein (CETP) inhibitors, novel peroxisome proliferator-activated receptor (PPAR) agonists, liver X receptor (LXR) agonists and RVX-208. For each drug, the biological mechanisms of these molecules, an overview of the current state of the clinical trials and the future perspectives will be provided.
2 Cholesteryl Ester Transfer Protein Inhibitors
2.1 Biological Mechanisms
The cholesteryl ester transfer protein (CETP) promotes the transfer of triglycerides from apoB-containing lipoproteins (LDL, IDL and VLDL) to HDL-C in exchange for cholesteryl esters. Interest in CETP inhibitor development came from studies in families with CETP deficiency with hyperalphalipoproteinaemia CETP deficiency (Inazu 1990) and epidemiological studies showing that CETP gene variants are associated with increased HDL-C levels and a lower risk of coronary heart disease events (Curb et al. 2004).
2.2 Current State
Four CETP inhibitors have been developed in humans: torcetrapib, anacetrapib, dalcetrapib and evacetrapib. The first CETP inhibitor designed by Pfizer and tested in phase III clinical trials was torcetrapib. The initial results of the ILLUMINATE (Investigation of Lipid Level Management to Understand its Impact in Atherosclerotic Events) trial were encouraging, with a 72 % increase in HDL-C and a 25 % decrease in LDL-C in patients with high CVD risk treated with torcetrapib on top of atorvastatin (Kastelein et al. 2007). However, all studies were interrupted because of an increased risk of cardiovascular events and an excess of mortality upon torcetrapib usage, possibly due to an increase in aldosterone level and blood pressure (Barter et al. 2007). Further analyses have demonstrated that the effect on blood pressure was independent of CETP inhibition. Indeed, torcetrapib increases blood pressure in mice that do not express CETP (Forrest et al. 2008). Furthermore, genetic association studies in 58,948 subjects with polymorphism in CETP gene report that CETP genotype was not associated with systolic nor diastolic blood pressure (Sofat et al. 2010). These results suggest that toxicity upon torcetrapib treatment could be CETP independent.
Even though the dal-OUTCOMES trial with dalcetrapib (Roche) showed an increase of HDL-C by 30 %, the results showed futility and trials were halted due to the absence of obvious benefit (Schwartz et al. 2012). Furthermore, the effect of dalcetrapib on vessel wall structure and vascular inflammation was investigated after a 2-year treatment in the dal-PLAQUE trial (Fayad et al. 2011). No significant benefit was reported in dalcetrapib-treated patients, but in patients with low HDL-C at baseline, beneficial effects on endothelial function were observed. However, in the dal-VESSEL study, designed to validate these results, the beneficial effects were not confirmed (Lüscher et al. 2012). Nevertheless, despite these failures, no vascular toxicity and blood pressure increase were observed on top of dalcetrapib treatment (Lüscher et al. 2012). Based on these results, two other more potent CETP inhibitors, anacetrapib and evacetrapib, have been developed and are still in phase III clinical trials.
2.3 Future Perspectives
Anacetrapib is a potent CETP inhibitor developed by Merck. In a first clinical trial, anacetrapib increased HDL-C by 138 % and reduced LDL-C by 40 % in patients with coronary artery disease or at high risk for coronary heart disease on statin therapy. This clinical trial with the acronym DEFINE (Determining the EFficacy and Tolerability of CETP Inhibition with Anacetrapib), demonstrated the safety of anacetrapib and absence of significant changes in blood pressure, aldosterone and electrolyte levels (Cannon et al. 2010). Currently, a phase III clinical trial is ongoing, acronym REVEAL (Randomized EValuation of the Effects of Anacetrapib Through Lipid-modification), which will determine whether lipid modification on anacetrapib therapy reduces the risk of coronary death, myocardial infarction (MI) or coronary revascularisation in patients with circulatory problems and low LDL-C on statin therapy (ClinicalTrials.gov identifier: NCT01252953). The results of this trial are expected at the beginning of 2017.
Evacetrapib, designed by Eli Lilly & Company, is the fourth member of the CETP inhibitor class that is tested in clinical trials. A phase II clinical trial evaluated the efficacy of evacetrapib as monotherapy or in combination with the most prescribed statins in patients with either hypercholesterolaemia or low HDL-C levels. As monotherapy, evacetrapib (30 mg, 100 mg or 500 mg/day) dose-dependently reduced LDL-C from 14 to 36 % and increased HDL-C from 54 to 129 %. Although the decrease of LDL-C was higher in combination with statins (49 % vs. 24 %), the increase of HDL-C was not stronger when compared to evacetrapib monotherapy (Nicholls et al. 2011). No adverse effects were observed in this trial, with no changes in blood pressure or aldosterone levels. Thus evacetrapib appears to be well-tolerated (Nicholls et al. 2011). The benefits of evacetrapib in combination with statins will be determined in a phase III randomised outcome trial, acronym ACCELERATE (Assessment of Clinical Effects of Cholesteryl Ester Transfer Protein Inhibition with Evacetrapib in Patients at a High-Risk for Vascular Outcomes) (Estimated end date: January 2016; ClinicalTrials.gov identifier: NCT01687998).
3 Novel PPAR Agonists
3.1 Biological Mechanisms
Peroxisome proliferator-activated receptors (PPARs) are a nuclear receptor subfamily with three members, PPARα, PPARγ and PPARβ/δ, encoded by distinct genes. The three isoforms display distinct patterns of expression with PPARα being highly expressed in liver, kidney, heart, muscle and brown adipose tissue, PPARγ is most abundant in adipose tissue, whereas PPARβ/δ is ubiquitously expressed (Lefebvre et al. 2006). Upon heterodimerisation with the retinoic X receptor, PPARs bind to PPAR response elements (PPRE) located in the promoters of their target genes and thus exert negative or positive control on their transcription.
The role of PPARα was initially studied in the liver where it enhances fatty acid oxidation, regulates gluconeogenesis through an increase of pyruvate dehydrogenase kinase 4 expression and ketone body production in response to the fasting state. Through its natural ligands, such as long-chain unsaturated fatty acids, arachidonic acid derivatives and oxidised phospholipids, PPARα regulates also some genes involved in lipid and lipoprotein metabolism. The increase of apoAV and lipoprotein lipase expression by PPARα activation associated with the reduction of apoCIII expression contributes to reduced plasma triglyceride levels in humans. Moreover, plasma HDL cholesterol levels increase as a result of the stimulation of two major HDL-associated apolipoproteins, apoAI and apoAII, by PPARα (Staels et al. 1998). In addition to these hepatic effects, PPARα activation enhances reverse cholesterol transport related to the increase of ATP-binding cassette transporter A1 (ABCA1) in macrophages (Chinetti et al. 2001) and exerts many pleiotropic effects on vascular remodelling and inflammatory responses.
PPARγ is activated by natural ligands such as polyunsaturated fatty acids, 15-deoxy-Δ12,14-prostaglandin J2 and oxidised fatty acids. In addition, pharmacological PPARγ agonists, the thiazolidinediones, are used as insulin sensitisers. Furthermore, PPARγ is the major regulator of adipogenesis (Tontonoz and Spiegelman 2008). PPARγ regulates the expression of adipokines such as adiponectin (Yu et al. 2002). In addition to this adipogenic effect, PPARγ displays anti-inflammatory actions and promotes the polarisation of monocytes towards alternative M2 macrophages (Bouhlel et al. 2007).
PPARβ/δ is activated by long-chain unsaturated fatty acids, and several synthetic ligands have been designed including L-165041, GW501516 and GW0742. However, no PPARβ/δ agonists are in clinical use yet. PPARβ/δ is highly expressed in skeletal muscle where it increases the expression of fatty acid oxidation-related genes. This nuclear receptor also improves lipid metabolism by reducing triglycerides and LDL-C levels and by increasing HDL-C levels. Moreover, PPARβ/δ activation increases insulin sensitivity (Oliver et al. 2001).
Overall, PPARs are involved in the control of lipid lipoprotein and glucose metabolism as well as in the inflammatory response (Lefebvre et al. 2006).
3.2 Current State
Among the pharmacologically used PPARα ligands are the fibrates, which are currently clinically used as hypolipidaemic drugs. Clinical benefits of fibrates were reported in primary and secondary intervention trials and reviewed in a meta-analysis (Jun et al. 2010). In line with their capacity to increase HDL-C and reduce triglycerides and LDL-C (Jun et al. 2010), their effects on the incidence of coronary heart disease appear most pronounced in patients with high triglycerides (>200 mg/dL) and/or low HDL-C (<40 mg/dL), although this has not yet been formally proven in a dedicated trial in type 2 diabetes patients (Suh et al. 2012; Keech et al. 2005).
Each PPAR isoform displays specific roles, with PPARα controlling lipid metabolism, whereas PPARδ improves also glucose metabolism. An interesting strategy consisted in the development of dual agonists with synergistic effects on different PPAR isoforms and minimal side effects (Rosenson et al. 2012). In this context, Roche developed a dual PPAR α/γ agonist, aleglitazar. Despite promising results in the synchrony study, with an improvement of lipid and glucose parameters in type 2 diabetes patients (Henry et al. 2009), the AleCardio phase III trial failed due to adverse effects on heart failure. Subsequently, all trials with aleglitazar were stopped (press report: http://www.roche.com/media/media_releases/med-cor-2013-07-10.htm).
3.3 Future Perspectives
Some limitations of fibrate therapy are their relatively weak activity on PPARα and their efficacy that depends on the targeted population (Staels 2010). To address these issues, several highly selective and potent PPAR agonists were developed (Fruchart 2013). The KOWA Company is developing K-877, a potent PPARα agonist. In a comparative clinical trial (International Clinical Trials identifier: JPRN-JapicCTI-121764), patients with hypertriglyceridaemia and low HDL-C were treated with K-877 or fenofibrate for 12 weeks. The first results showed that the increase of HDL-C is stronger by K-877 than by fenofibrate. In addition, none of the adverse effects induced by fenofibrate, such as increased levels of serum homocysteine and creatinine, were observed in K-877-treated patients (http://www.kenes.com/eas2012/abstracts/pdf/525.pdf). This molecule is currently in phase II in the USA and EU (International Clinical Trials identifier: EUCTR2013-001517-32-SE) and in phase III clinical trials for atherosclerotic dyslipidaemia in Japan (International Clinical Trials identifier: JPRN-JapicCTI-132067).
A HDL-inducer developed by Cerenis Therapeutics is a specific PPARδ agonist, CER-002. The phase I clinical trial demonstrated that CER-002 is well-tolerated without major adverse effects (press report: http://www.drugs.com/clinical_trials/cerenis-therapeutics-announces-successful-completion-phase-clinical-trial-cer-002-cardiovascular-4272.html). Another selective PPARδ agonist, HPP593, is currently tested in healthy subjects, and its effect on LDL and HDL cholesterol as well as triglycerides will be determined (press report: http://www.ttpharma.com/TherapeuticAreas/MetabolicDisorders/Dyslipidemia/HPP593/tabid/118/Default.aspx).
The synthetic, non-thiazolidinedione PPARγ compound, INT131, improves glucose tolerance in rodent models of diabetes to a similar extent as rosiglitazone. However, no major adverse events, such as weight gain, haemodilution or plasma volume increase, were observed in INT131-treated rats compared to rosiglitazone-treated rats (Motani et al. 2009). In a randomised, double-blind study, type 2 diabetes patients were treated 4 weeks with 1 or 10 mg of INT131. Consistent with the in vitro data, INT131 displayed a glucose-lowering activity and increased HDL-C levels without changing other lipid parameters (Dunn et al. 2011). This molecule is currently tested in a comparative clinical study in type 2 diabetes patients treated for 24 weeks with INT131 or pioglitazone (ClinicalTrials.gov Identifier: NCT00631007).
In addition, a phase I clinical trial is ongoing to evaluate safety, tolerability and pharmacokinetic behaviour of a new PPAR α/γ modulator, DSP-8658, in type 2 diabetes mellitus and healthy subjects (ClinicalTrials.gov Identifier: NCT01042106). DSP-8658 is a non-thiazolidinedione compound which exhibits potent anti-hyperglycaemic effects, reduces plasma triglycerides and increases HDL-C levels with less side effects on, e.g., body weight gain (press report: www.ds-pharma.com/ir/library/presentation/pdf).
Finally, the new dual PPAR α/δ agonist GFT505, developed by Genfit, reduced plasma triglycerides and increased HDL-C levels in abdominally obese patients with either dyslipidaemia or prediabetes (Cariou et al. 2011). A phase IIb clinical trial is ongoing to evaluate the efficacy of GFT505 in patients with non-alcoholic steatohepatitis (ClinicalTrials.gov identifier: NCT01694849), an unmet clinical need because of the continuous increasing incidence of fatty liver disease due to abdominal obesity (Tailleux et al. 2012).
These novel selective PPAR agonists, K-877, CER-002, DSP-8658, INT131 and GFT505 appear promising drugs to treat the cardiovascular risk associated with metabolic syndrome and type 2 diabetes.
4 Novel LXR Agonists
4.1 Biological Mechanisms
Liver X receptors (LXRs) are nuclear receptors. There are two isoforms, LXRα and LXRβ, with LXRα mainly expressed in the liver, intestine, kidney and spleen, whereas LXRβ is ubiquitously expressed (Repa and Mangelsdorf 2000). Oxysterols and other cholesterol metabolites are natural ligands for LXRs, and several synthetic ligands were also developed (T0901317, GW3965). After their binding, LXRs modulate the expression of genes involved in cholesterol metabolism and transport and glucose metabolism (Schultz et al. 2000; Laffitte et al. 2003). Activation of LXR in macrophages induces ABCA1, ABCG1 and apoE expression which promotes cholesterol efflux and reverses cholesterol transport (Sabol et al. 2005; Venkateswaran et al. 2000; Laffitte et al. 2001). Besides their effects on lipid metabolism, LXRs display anti-inflammatory properties (Joseph et al. 2003) and improve glucose tolerance. In contrast to their beneficial effects, LXR activation induces fatty acid synthesis (de novo lipogenesis) related to a modulation of the hepatic expression of sterol regulatory element-binding protein (SREBP-1), stearoyl-CoA desaturase-1 (SCD-1), fatty acid synthase (FAS) and acetyl-CoA carboxylase (ACC) (Schultz et al. 2000). This upregulation of hepatic SREBP-1c expression may contribute to the elevation of plasma triglycerides.
4.2 Current State
T0901317 and GW3965, the most studied agonists, have been extensively described to exert beneficial effects in preclinical animal models of cardiovascular diseases, neurodegenerative diseases and inflammation (Terasaka et al. 2003; Joseph et al. 2002, 2003; Zelcer et al. 2007). However, LXR ligands have not yet been tested in clinical trials because of their adverse effects such as an increase of hepatic lipogenesis, hypertriglyceridaemia and hepatosteatosis (Calkin and Tontonoz 2012). These lipogenic effects have been assigned to LXRα which is highly expressed in the liver (Lehrke et al. 2005; Bradley et al. 2007). Therapeutic strategies are now focusing on the development of selective LXR modulators, LXRβ-specific agonists and/or ligands which act selectively in specific tissues in order to maintain positive effects on cholesterol metabolism and minimise the lipid side effects.
LXR-623 (WAY-252623) is a novel synthetic ligand with higher potency for LXRβ, which induces plaque regression in combination with statins in a rabbit model of atherosclerosis (Giannarelli et al. 2012). LXR-623 entered in a phase I trial (NCT00366522) to test tolerance and safety in humans (Katz et al. 2009). However, its development was interrupted because of adverse effects in the central nervous system with potential induction of psychiatric disorders.
4.3 Future Perspectives
A novel synthetic, steroidal LXR ligand, ATI-111, has been developed. This molecule is most potent on LXRα with modest effects on LXRβ. The higher efficiency on LXRα allows its utilisation at lower concentrations than T0901317, which probably reduces cytotoxicity and also adverse effects such as hypertriglyceridaemia. To determine whether ATI-111 does not provoke hypertriglyceridaemia, mice were treated with 5 mg.kg-1.day-1 of ATI-111 for 8 weeks. Interestingly, a decrease of plasma triglyceride levels and VLDL cholesterol was observed in ATI-111-treated mice (Peng et al. 2011). In addition, ATI-111 exhibits anti-inflammatory properties with a decrease of LPS-induced inflammatory gene expression. Furthermore, ATI-111 reduced atherosclerotic lesions in LDL-receptor-deficient mice (Peng et al. 2011). Altogether, accumulating proofs from in vitro and in vivo animal studies show beneficial effects of ATI-111 on atherosclerosis with anti-inflammatory effects, a reduction of hypertriglyceridaemia and a consequential decrease of atherosclerotic lesions. Further molecular investigations are necessary to assess the full potential of ATI-111 in clinical trials.
A phase I clinical trial with XL-652 (XL-014), a novel LXR ligand, is currently ongoing to evaluate its safety (www.exelixis.com/pipeline/xl652).
5 RVX-208
5.1 Biological Mechanisms
An alternative strategy to raise the serum level of HDL-C is to increase one of the major HDL proteins, apolipoprotein AI (apoAI). In this context, after a screening assay in HepG2 cells to identify molecules inducing apoAI, Resverlogix Corporation has selected and developed an oral quinazoline molecule, RVX-208 (RVX-000222). This molecule, a derivative of resveratrol, increases hepatic apoAI production (Bailey et al. 2010). Thus RVX-208 is a small molecule for potential treatment of cardiovascular diseases.
5.2 Current State
First in vitro experiments have shown that RVX-208 increases apoAI mRNA, protein and the release of apoAI in the medium of HepG2 cells (Bailey et al. 2010). To test its efficiency in vivo, male monkeys were orally treated with RVX-208 for 63 days. This in vivo study in nonhuman primates demonstrated that RVX-208 increases in a dose-dependent manner serum levels of apoAI and preβ-HDL-C (Bailey et al. 2010). No adverse effects were observed in monkeys. In humans, 7 days of treatment increased preβ-HDL, apoAI and cholesterol efflux (Bailey et al. 2010). The efficacy and safety of RVX-208 was furthermore investigated in a phase II randomised trial including 299 statin-treated patients with coronary artery diseases (ASSERT study: NTC01058018). Twice daily administration of RVX-208 (50, 100 and 150 mg) was well tolerated; however, a transient elevation in transaminase levels was found in some RVX-208-treated patients. Furthermore, only a modest increase of HDL-C level (3.2–8.3 %) was observed (Nicholls et al. 2011). In a next phase IIb clinical study, the ASSURE (ApoAI Synthesis Stimulation and Intravascular Ultrasound for Coronary Atheroma Regression Evaluation) trial, the effect of 26 weeks treatment with RVX-208 (100 mg) was determined on the progression of coronary atherosclerosis in 323 patients with symptomatic coronary artery disease and low HDL-C levels. The primary end point, change in atheroma volume determined by intravascular ultrasound (IVUS), was not met. No significant change in plaque regression was observed between placebo and RVX-208 group. The question is whether this lack of beneficial effect on plaque regression is due to the weak efficacy of RVX-208 or the impossibility to confer beneficial effects on top of statins, since 84 % of patients were on statin therapy. Furthermore, the increases of apoAI and HDL-C levels did not differ from placebo, whereas transaminases were again found to be elevated. Thus, so far, no clinical benefit has been demonstrated with RVX-208 (press report: communication Nicholls SJ www.clinicaltrialresults.org/Nicholls_ASSURE).
Conclusion
To reduce residual cardiovascular risk persisting after statin therapy, novel therapeutic strategies based on raising HDL-C are currently under investigation. However, the utility of increasing HDL-C is not yet established, and pharmaceutical manipulation of HDL-C appears to be less efficient than lowering LDL-C to reduce cardiovascular risk. Moreover, the failure of several clinical trials with the first members of the CETP inhibitor class, torcetrapib and dalcetrapib, and the lack of beneficial effects of an increase of HDL-C and the reduction of cardiovascular events raises doubts about the relevance of the “HDL-C hypothesis”. These disappointing results highlight the complexity of HDL metabolism in contrast to that of LDL.
Many biological activities of HDL, such as antioxidant, anti-inflammatory and antiapoptotic properties, are mediated by different HDL subclasses, and solely increasing HDL-C may not enhance these functions. Moreover, plasma HDL contains heterogeneous particle subpopulations whose composition, metabolism and functionality differ depending on the metabolic status (Besler et al. 2011). Thus far, the larger randomised placebo controlled phase III clinical trials have shown that an increase in HDL-C does not benefit the patient, and thus, future strategies should aim at improving HDL function.
Abbreviations
- ABCA1:
-
ATP-binding cassette transporter A1
- ABCG1:
-
ATP-binding cassette transporter G1
- ACC:
-
Acetyl-CoA carboxylase
- Apo:
-
apolipoprotein
- CETP:
-
Cholesteryl ester transfer protein
- CVD:
-
Cardiovascular disease
- FAS:
-
Fatty acid synthase
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- LXR:
-
Liver X receptor
- MTTP:
-
Microsomal triglyceride transfer protein
- PPAR:
-
Peroxisome proliferator-activated receptor
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- SCD-1:
-
Stearoyl-CoA desaturase-1
- SREBP-1:
-
Sterol regulatory element-binding protein
References
Bailey D, Jahagirdar R, Gordon A, Hafiane A, Campbell S, Chatur S, Wagner GS, Hansen HC, Chiacchia FS, Johansson J, Krimbou L, Wong NCW, Genest J (2010) RVX-208: a small molecule that increases apolipoprotein AI and high-density lipoprotein cholesterol in vitro and in vivo. J Am Coll Cardiol 55:2580–2589
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJP, Komajda M, Lopez-Sendon J, Mosca L, Tardif J, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B (2007) Effects of Torcetrapib in patients at high risk for coronary events. N Engl J Med 357:2109–2122
Besler C, Heinrich K, Rohrer L, Doerries C, Riwanto M, Shih DM, Chroni A, Yonekawa K, Stein S, Schaefer N, Mueller M, Akhmedov A, Daniil G, Manes C, Templin C, Wyss C, Maier W, Tanner FC, Matter CM, Corti R, Furlong C, Lusis AJ, von Eckardstein A, Fogelman AM, Lüscher TF, Landmesser U (2011) Mechanisms underlying adverse effects of HDL on enos-activating pathways in patients with coronary artery disease. J Clin Invest 121:2693–2708
Bouhlel MA, Derudas B, Rigamonti E, Dièvart R, Brozek J, Haulon S, Zawadzki C, Jude B, Torpier G, Marx N, Staels B, Chinetti-Gbaguidi G (2007) PPARgamma activation primes human monocytes into alternative m2 macrophages with anti-inflammatory properties. Cell Metab 6:137–143
Bradley MN, Hong C, Chen M, Joseph SB, Wilpitz DC, Wang X, Lusis AJ, Collins A, Hseuh WA, Collins JL, Tangirala RK, Tontonoz P (2007) Ligand activation of LXR beta reverses atherosclerosis and cellular cholesterol overload in mice lacking LXR alpha and apoE. J Clin Invest 117:2337–2346
Calkin AC, Tontonoz P (2012) Transcriptional integration of metabolism by the nuclear sterol-activated receptors LXR and FXR. Nat Rev Mol Cell Biol 13:213–224
Cannon CP, Shah S, Dansky HM, Davidson M, Brinton EA, Gotto AM, Stepanavage M, Liu SX, Gibbons P, Ashraf TB, Zafarino J, Mitchel Y, Barter P (2010) Safety of Anacetrapib in patients with or at high risk for coronary heart disease. N Engl J Med 363:2406–2415
Cariou B, Zaïr Y, Staels B, Bruckert E (2011) Effects of the new dual PPAR α/δ agonist GFT505 on lipid and glucose homeostasis in abdominally obese patients with combined dyslipidemia or impaired glucose metabolism. Diabetes Care 34:2008–2014
Chinetti G, Lestavel S, Bocher V, Remaley AT, Neve B, Torra IP, Teissier E, Minnich A, Jaye M, Duverger N, Brewer HB, Fruchart JC, Clavey V, Staels B (2001) PPAR-alpha and PPAR-gamma activators induce cholesterol removal from human macrophage foam cells through stimulation of the ABCA1 pathway. Nat Med 7:53–58
Curb JD, Abbott RD, Rodriguez BL, Masaki K, Chen R, Sharp DS, Tall AR (2004) A prospective study of HDL-C and cholesteryl ester transfer protein gene mutations and the risk of coronary heart disease in the elderly. J Lipid Res 45:948–953
Dunn FL, Higgins LS, Fredrickson J, DePaoli AM (2011) Selective modulation of PPARγ activity can lower plasma glucose without typical thiazolidinedione side-effects in patients with type 2 diabetes. J Diabetes Complicat 25:151–158
Fayad ZA, Mani V, Woodward M, Kallend D, Abt M, Burgess T, Fuster V, Ballantyne CM, Stein EA, Tardif J, Rudd JHF, Farkouh ME, Tawakol A (2011) Safety and efficacy of Dalcetrapib on atherosclerotic disease using novel non-invasive multimodality imaging (dal-plaque): a randomised clinical trial. Lancet 378:1547–1559
Forrest MJ, Bloomfield D, Briscoe RJ, Brown PN, Cumiskey AM, Ehrhart J, Hershey JC, Keller WJ, Ma X, McPherson HE, Messina E, Peterson LB, Sharif-Rodriguez W, Siegl PK, Sinclair PJ, Sparrow CP, Stevenson AS, Sun SY, Tsai C, Vargas H, Walker M 3rd, West SH, White V, Woltmann RF (2008) Torcetrapib-induced blood pressure elevation is independent of cetp inhibition and is accompanied by increased circulating levels of aldosterone. Br J Pharmacol 154:1465–1473
Fruchart J (2013) Selective peroxisome proliferator-activated receptor α modulators (SPPARMα): the next generation of peroxisome proliferator-activated receptor α-agonists. Cardiovasc Diabetol 12:82
Giannarelli C, Cimmino G, Connolly TM, Ibanez B, Ruiz JMG, Alique M, Zafar MU, Fuster V, Feuerstein G, Badimon JJ (2012) Synergistic effect of Liver X Receptor activation and simvastatin on plaque regression and stabilization: an magnetic resonance imaging study in a model of advanced atherosclerosis. Eur Heart J 33:264–273
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR (1977) High density lipoprotein as a protective factor against coronary heart disease the framingham study. Am J Med 62:707–714
Henry RR, Lincoff AM, Mudaliar S, Rabbia M, Chognot C, Herz M (2009) Effect of the dual peroxisome proliferator-activated receptor-alpha/gamma agonist aleglitazar on risk of cardiovascular disease in patients with type 2 diabetes (synchrony): a phase II, randomised, dose-ranging study. Lancet 374:126–135
Inazu A, Brown ML, Hesler CB, Agellon LB, Koizumi J, Takata K, Maruhama Y, Mabuchi H, Tall AR (1990) Increased high-density lipoprotein levels caused by a common cholesteryl-ester transfer protein gene mutation. N Engl J Med 323:1234–1238
Joseph SB, McKilligin E, Pei L, Watson MA, Collins AR, Laffitte BA, Chen M, Noh G, Goodman J, Hagger GN, Tran J, Tippin TK, Wang X, Lusis AJ, Hsueh WA, Law RE, Collins JL, Willson TM, Tontonoz P (2002) Synthetic LXR ligand inhibits the development of atherosclerosis in mice. Proc Natl Acad Sci USA 99:7604–7609
Joseph SB, Castrillo A, Laffitte BA, Mangelsdorf DJ, Tontonoz P (2003) Reciprocal regulation of inflammation and lipid metabolism by Liver X Receptors. Nat Med 9:213–219
Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, Grobbee DE, Cass A, Chalmers J, Perkovic V (2010) Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet 375:1875–1884
Kastelein JJP, van Leuven SI, Burgess L, Evans GW, Kuivenhoven JA, Barter PJ, Revkin JH, Grobbee DE, Riley WA, Shear CL, Duggan WT, Bots ML (2007) Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med 356:1620–1630
Katz A, Udata C, Ott E, Hickey L, Burczynski ME, Burghart P, Vesterqvist O, Meng X (2009) Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel Liver X-Receptor agonist, in healthy participants. J Clin Pharmacol 49:643–649
Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, Forder P, Pillai A, Davis T, Glasziou P, Drury P, Kesäniemi YA, Sullivan D, Hunt D, Colman P, D’Emden M, Whiting M, Ehnholm C, Laakso M (2005) Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the field study): randomised controlled trial. Lancet 366:1849–1861
Laffitte BA, Repa JJ, Joseph SB, Wilpitz DC, Kast HR, Mangelsdorf DJ, Tontonoz P (2001) LXRs control lipid-inducible expression of the apolipoprotein E gene in macrophages and adipocytes. Proc Natl Acad Sci USA 98:507–512
Laffitte BA, Chao LC, Li J, Walczak R, Hummasti S, Joseph SB, Castrillo A, Wilpitz DC, Mangelsdorf DJ, Collins JL, Saez E, Tontonoz P (2003) Activation of Liver X Receptor improves glucose tolerance through coordinate regulation of glucose metabolism in liver and adipose tissue. Proc Natl Acad Sci USA 100:5419–5424
Laslett LJ, Alagona PJ, Clark BA, Drozda JPJ, Saldivar F, Wilson SR, Poe C, Hart M (2012) The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the american college of cardiology. J Am Coll Cardiol 60:S1–S49
Lefebvre P, Chinetti G, Fruchart J, Staels B (2006) Sorting out the roles of PPAR alpha in energy metabolism and vascular homeostasis. J Clin Invest 116:571–580
Lehrke M, Lebherz C, Millington SC, Guan H, Millar J, Rader DJ, Wilson JM, Lazar MA (2005) Diet-dependent cardiovascular lipid metabolism controlled by hepatic LXRalpha. Cell Metab 1:297–308
Lüscher TF, Taddei S, Kaski J, Jukema JW, Kallend D, Münzel T, Kastelein JJP, Deanfield JE (2012) Vascular effects and safety of Dalcetrapib in patients with or at risk of coronary heart disease: the dal-vessel randomized clinical trial. Eur Heart J 33:857–865
Motani A, Wang Z, Weiszmann J, McGee LR, Lee G, Liu Q, Staunton J, Fang Z, Fuentes H, Lindstrom M, Liu J, Biermann DHT, Jaen J, Walker NPC, Learned RM, Chen J, Li Y (2009) INT131: a selective modulator of PPAR gamma. J Mol Biol 386:1301–1311
Nicholls SJ, Brewer HB, Kastelein JJP, Krueger KA, Wang M, Shao M, Hu B, McErlean E, Nissen SE (2011) Effects of the cetp inhibitor Evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial. JAMA 306:2099–2109
Oliver WRJ, Shenk JL, Snaith MR, Russell CS, Plunket KD, Bodkin NL, Lewis MC, Winegar DA, Sznaidman ML, Lambert MH, Xu HE, Sternbach DD, Kliewer SA, Hansen BC, Willson TM (2001) A selective peroxisome proliferator-activated receptor delta agonist promotes reverse cholesterol transport. Proc Natl Acad Sci USA 98:5306–5311
Peng D, Hiipakka RA, Xie J, Dai Q, Kokontis JM, Reardon CA, Getz GS, Liao S (2011) A novel potent synthetic steroidal Liver X Receptor agonist lowers plasma cholesterol and triglycerides and reduces atherosclerosis in LDLR(-/-) mice. Br J Pharmacol 162:1792–1804
Repa JJ, Mangelsdorf DJ (2000) The role of orphan nuclear receptors in the regulation of cholesterol homeostasis. Annu Rev Cell Dev Biol 16:459–481
Roche Group Communications (2013) Roche halts investigation of aleglitazar following regular safety review of phase III trial. http://www.roche.com/media/media_releases/med-cor-2013-07-10.html
Rosenson RS, Wright RS, Farkouh M, Plutzky J (2012) Modulating peroxisome proliferator-activated receptors for therapeutic benefit? Biology, clinical experience, and future prospects. Am Heart J 164:672–680
Sabol SL, Brewer HBJ, Santamarina-Fojo S (2005) The human ABCG1 gene: identification of LXR response elements that modulate expression in macrophages and liver. J Lipid Res 46:2151–2167
Schultz JR, Tu H, Luk A, Repa JJ, Medina JC, Li L, Schwendner S, Wang S, Thoolen M, Mangelsdorf DJ, Lustig KD, Shan B (2000) Role of LXRs in control of lipogenesis. Genes Dev 14:2831–2838
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, Chaitman BR, Holme IM, Kallend D, Leiter LA, Leitersdorf E, McMurray JJV, Mundl H, Nicholls SJ, Shah PK, Tardif J, Wright RS (2012) Effects of Dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 367:2089–2099
Sofat R, Hingorani AD, Smeeth L, Humphries SE, Talmud PJ, Cooper J, Shah T, Sandhu MS, Ricketts SL, Boekholdt SM, Wareham N, Khaw KT, Kumari M, Kivimaki M, Marmot M, Asselbergs FW, van der Harst P, Dullaart RP, Navis G, van Veldhuisen DJ, Van Gilst WH, Thompson JF, McCaskie P, Palmer LJ, Arca M, Quagliarini F, Gaudio C, Cambien F, Nicaud V, Poirer O, Gudnason V, Isaacs A, Witteman JC, van Duijn CM, Pencina M, Vasan RS, D’Agostino RB Sr, Ordovas J, Li TY, Kakko S, Kauma H, Savolainen MJ, Kesäniemi YA, Sandhofer A, Paulweber B, Sorli JV, Goto A, Yokoyama S, Okumura K, Horne BD, Packard C, Freeman D, Ford I, Sattar N, McCormack V, Lawlor DA, Ebrahim S, Smith GD, Kastelein JJ, Deanfield J, Casas JP (2010) Separating the mechanism-based and off-target actions of cholesteryl ester transfer protein inhibitors with cetp gene polymorphisms. Circulation 121:52–62
Staels B (2010) Fibrates in CVD: a step towards personalised medicine. Lancet 375:1847–1848
Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC (1998) Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation 98:2088–2093
Suh HS, Hay JW, Johnson KA, Doctor JN (2012) Comparative effectiveness of statin plus fibrate combination therapy and statin monotherapy in patients with type 2 diabetes: use of propensity-score and instrumental variable methods to adjust for treatment-selection bias. Pharmacoepidemiol Drug Saf 21:470–484
Tailleux A, Wouters K, Staels B (2012) Roles of PPARs in NAFLD: potential therapeutic targets. Biochim Biophys Acta 1821:809–818
Terasaka N, Hiroshima A, Koieyama T, Ubukata N, Morikawa Y, Nakai D, Inaba T (2003) T-0901317, a synthetic Liver X Receptor ligand, inhibits development of atherosclerosis in LDL receptor-deficient mice. FEBS Lett 536:6–11
Tontonoz P, Spiegelman BM (2008) Fat and beyond: the diverse biology of PPARgamma. Annu Rev Biochem 77:289–312
Venkateswaran A, Laffitte BA, Joseph SB, Mak PA, Wilpitz DC, Edwards PA, Tontonoz P (2000) Control of cellular cholesterol efflux by the nuclear oxysterol receptor LXR alpha. Proc Natl Acad Sci USA 97:12097–12102
www.ttpharma.com/therapeuticAreas/MetabolicDisorders/Dyslipidemia/HPP593
Yu JG, Javorschi S, Hevener AL, Kruszynska YT, Norman RA, Sinha M, Olefsky JM (2002) The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 51:2968–2974
Zelcer N, Khanlou N, Clare R, Jiang Q, Reed-Geaghan EG, Landreth GE, Vinters HV, Tontonoz P (2007) Attenuation of neuroinflammation and alzheimer’s disease pathology by Liver X Receptors. Proc Natl Acad Sci USA 104:10601–10606
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this chapter
Cite this chapter
Colin, S., Chinetti-Gbaguidi, G., Kuivenhoven, J.A., Staels, B. (2015). Emerging Small Molecule Drugs. In: von Eckardstein, A., Kardassis, D. (eds) High Density Lipoproteins. Handbook of Experimental Pharmacology, vol 224. Springer, Cham. https://doi.org/10.1007/978-3-319-09665-0_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-09665-0_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09664-3
Online ISBN: 978-3-319-09665-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)