Abstract
The large airways are a critical component of the respiratory tree serving both an immunoprotective role and a physiological role for ventilation. The physiological role of the large airways is to move a large amount of air to and from the gas exchange surfaces of the alveoli. This air becomes divided along the respiratory tree as it moves from the large airways to smaller airways, bronchioles, and alveoli. The large airways are incredibly important from an immunoprotective role as the large airways are an early line of defense against inhaled particles, bacteria, and viruses. The key immunoprotective feature of the large airways is mucus production and mucociliary clearance mechanism. Each of these key features of the lung is important from both a basic physiology perspective and an engineering perspective for regenerative medicine. In this chapter, we will cover the large airways from an engineering perspective to highlight existing models of the large airways as well as future directions for modeling and repair.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Feher J. 6.1 – The Mechanics of Breathing. In: Feher J, editor. Quantitative Human Physiology (Second Edition) [Internet]. Boston: Academic Press; 2017 [cited 2022 Aug 4]. p. 623–32. Available from: https://www.sciencedirect.com/science/article/pii/B9780128008836000604
Eskandari M, Arvayo AL, Levenston ME. Mechanical properties of the airway tree: heterogeneous and anisotropic pseudoelastic and viscoelastic tissue responses. J Appl Physiol. 2018 Sep;125(3):878–88.
Kia’i N, Bajaj T. Histology, Respiratory Epithelium. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Aug 4]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK541061/
Shi HC, Deng WJ, Pei C, Lu D, Zhang XJ, Wang XH, et al. Biomechanical properties of adult-excised porcine trachea for tracheal xenotransplantation. Xenotransplantation. 2009 Jun;16(3):181–6.
Zhang B, Lu Y, Sun F, Wu Q, Shi H. Compression property of trachea: A key mechanical property for artificial trachea graft. Am J Otolaryngol. 2022 Jun;43(3):103413.
Eskandari M, Nordgren TM, O’Connell GD. Mechanics of Pulmonary Airways: Linking Structure to Function Through Constitutive Modeling, Biochemistry, and Histology. Acta Biomater. 2019 Oct 1;97:513–23.
Carbone JE, Marini JJ. Bronchodilatory Effect of Warm Air Inhalation During Quiet Breathing. West J Med. 1984 Mar;140(3):398–402.
Uzeloto JS, Ramos D, Silva BS de A, Lima MBP de, Silva RN, Camillo CA, et al. Mucociliary Clearance of Different Respiratory Conditions: A Clinical Study. Int Arch Otorhinolaryngol. 2021 Jan;25(1):e35–40.
Mertens TCJ, Karmouty-Quintana H, Taube C, Hiemstra PS. Use of airway epithelial cell culture to unravel the pathogenesis and study treatment in obstructive airway diseases. Pulm Pharmacol Ther. 2017 Aug;45:101–13.
Liu G, Betts C, Cunoosamy DM, Åberg PM, Hornberg JJ, Sivars KB, et al. Use of precision cut lung slices as a translational model for the study of lung biology. Respir Res. 2019 Jul 19;20(1):162.
Berrocal T, Madrid C, Novo S, Gutiérrez J, Arjonilla A, Gómez-León N. Congenital Anomalies of the Tracheobronchial Tree, Lung, and Mediastinum: Embryology, Radiology, and Pathology. RadioGraphics. 2004 Jan;24(1):e17–e17.
Rommens JM, Iannuzzi MC, Kerem B, Drumm ML, Melmer G, Dean M, et al. Identification of the cystic fibrosis gene: chromosome walking and jumping. Science. 1989 Sep 8;245(4922):1059–65.
Pini L, Pinelli V, Modina D, Bezzi M, Tiberio L, Tantucci C. Central airways remodeling in COPD patients. Int J Chron Obstruct Pulmon Dis. 2014 Sep 1;9:927–33.
Joseph C, Tatler AL. Pathobiology of Airway Remodeling in Asthma: The Emerging Role of Integrins. J Asthma Allergy. 2022;15:595–610.
Hough KP, Curtiss ML, Blain TJ, Liu RM, Trevor J, Deshane JS, et al. Airway Remodeling in Asthma. Front Med [Internet]. 2020 [cited 2022 Aug 5];7. Available from: https://www.frontiersin.org/articles/10.3389/fmed.2020.00191
McCarron A, Parsons D, Donnelley M. Animal and Cell Culture Models for Cystic Fibrosis: Which Model Is Right for Your Application? Am J Pathol. 2021 Feb 1;191(2):228–42.
Sun X, Olivier AK, Liang B, Yi Y, Sui H, Evans TIA, et al. Lung phenotype of juvenile and adult cystic fibrosis transmembrane conductance regulator-knockout ferrets. Am J Respir Cell Mol Biol. 2014 Mar;50(3):502–12.
Klymiuk N, Mundhenk L, Kraehe K, Wuensch A, Plog S, Emrich D, et al. Sequential targeting of CFTR by BAC vectors generates a novel pig model of cystic fibrosis. J Mol Med. 2012 May 1;90(5):597–608.
Ghorani V, Boskabady MH, Khazdair MR, Kianmeher M. Experimental animal models for COPD: a methodological review. Tob Induc Dis. 2017 May 2;15:25.
Adamo D, Galaverni G, Genna VG, Lococo F, Pellegrini G. The Growing Medical Need for Tracheal Replacement: Reconstructive Strategies Should Overcome Their Limits. Front Bioeng Biotechnol. 2022;10:846632.
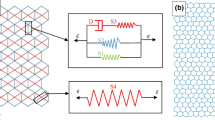
Marconi S, De Lazzari C. In silico study of airway/lung mechanics in normal human breathing. Math Comput Simul. 2020 Nov;177:603–24.
Wang Y, Li Y, Chen W, Zhang C, Liang L, Huang R, et al. Deep Learning for Automatic Upper Airway Obstruction Detection by Analysis of Flow-Volume Curve. Respir Int Rev Thorac Dis. 2022 May 12;1–10.
Foy BH, Soares M, Bordas R, Richardson M, Bell A, Singapuri A, et al. Lung Computational Models and the Role of the Small Airways in Asthma. Am J Respir Crit Care Med. 2019 Oct 15;200(8):982–91.
Moslemi A, Kontogianni K, Brock J, Wood S, Herth F, Kirby M. Differentiating COPD and Asthma using Quantitative CT Imaging and Machine Learning. Eur Respir J. 2022 Feb 24;2103078.
DeBoer EM, Kimbell JS, Pickett K, Hatch JE, Akers K, Brinton J, et al. Lung inflammation and simulated airway resistance in infants with cystic fibrosis. Respir Physiol Neurobiol. 2021 Nov;293:103722.
Longest PW, Bass K, Dutta R, Rani V, Thomas ML, El-Achwah A, et al. Use of computational fluid dynamics deposition modeling in respiratory drug delivery. Expert Opin Drug Deliv. 2019 Jan;16(1):7–26.
Huang F, Zhu Q, Zhou X, Gou D, Yu J, Li R, et al. Role of CFD based in silico modelling in establishing an in vitro-in vivo correlation of aerosol deposition in the respiratory tract. Adv Drug Deliv Rev. 2021 Mar;170:369–85.
Talaat M, Si XA, Dong H, Xi J. Leveraging statistical shape modeling in computational respiratory dynamics: Nanomedicine delivery in remodeled airways. Comput Methods Programs Biomed. 2021 Jun;204:106079.
Phuong NL, Quang TV, Khoa ND, Kim JW, Ito K. CFD analysis of the flow structure in a monkey upper airway validated by PIV experiments. Respir Physiol Neurobiol. 2020 Jan;271:103304.
Dong SJ, Wang L, Chitano P, Vasilescu DM, Paré PD, Seow CY. Airway and parenchymal tissue resistance and elastance in ex vivo sheep lungs: effects of bronchochallenge and deep inspiration. Am J Physiol Lung Cell Mol Physiol. 2022 Jun 1;322(6):L882–9.
Patil LS, Varner VD. Toward Measuring the Mechanical Stresses Exerted by Branching Embryonic Airway Epithelial Explants in 3D Matrices of Matrigel. Ann Biomed Eng. 2022 Sep;50(9):1143–57.
Fernandes-Silva H, Alves MG, Araújo-Silva H, Silva AM, Correia-Pinto J, Oliveira PF, et al. Lung branching morphogenesis is accompanied by temporal metabolic changes towards a glycolytic preference. Cell Biosci. 2021 Jul 17;11(1):134.
Li G, Cohen JA, Martines C, Ram-Mohan S, Brain JD, Krishnan R, et al. Preserving Airway Smooth Muscle Contraction in Precision-Cut Lung Slices. Sci Rep. 2020 Apr 15;10(1):6480.
Van Dijk EM, Culha S, Menzen MH, Bidan CM, Gosens R. Elastase-Induced Parenchymal Disruption and Airway Hyper Responsiveness in Mouse Precision Cut Lung Slices: Toward an Ex vivo COPD Model. Front Physiol. 2016;7:657.
Lauenstein L, Switalla S, Prenzler F, Seehase S, Pfennig O, Förster C, et al. Assessment of immunotoxicity induced by chemicals in human precision-cut lung slices (PCLS). Toxicol Vitro Int J Publ Assoc BIBRA. 2014 Jun;28(4):588–99.
Lam M, Royce SG, Donovan C, Jelinic M, Parry LJ, Samuel CS, et al. Serelaxin Elicits Bronchodilation and Enhances β-Adrenoceptor-Mediated Airway Relaxation. Front Pharmacol. 2016;7:406.
Preuß EB, Schubert S, Werlein C, Stark H, Braubach P, Höfer A, et al. The Challenge of Long-Term Cultivation of Human Precision-Cut Lung Slices. Am J Pathol. 2022 Feb;192(2):239–53.
Bailey KE, Pino C, Lennon ML, Lyons A, Jacot JG, Lammers SR, et al. Embedding of Precision-Cut Lung Slices in Engineered Hydrogel Biomaterials Supports Extended Ex Vivo Culture. Am J Respir Cell Mol Biol. 2020 Jan;62(1):14–22.
Damiano G, Palumbo VD, Fazzotta S, Curione F, Lo Monte G, Brucato VMB, et al. Current Strategies for Tracheal Replacement: A Review. Life Basel Switz. 2021 Jun 25;11(7):618.
Baranovskii D, Demner J, Nürnberger S, Lyundup A, Redl H, Hilpert M, et al. Engineering of Tracheal Grafts Based on Recellularization of Laser-Engraved Human Airway Cartilage Substrates. Cartilage. 2022 Mar;13(1):19476035221075950.
Tsao CK, Hsiao HY, Cheng MH, Zhong WB. Tracheal reconstruction with the scaffolded cartilage sheets in an orthotopic animal model. Tissue Eng Part A. 2022 Feb 9;
Xu Y, Dai J, Zhu X, Cao R, Song N, Liu M, et al. Biomimetic Trachea Engineering via a Modular Ring Strategy Based on Bone-Marrow Stem Cells and Atelocollagen for Use in Extensive Tracheal Reconstruction. Adv Mater Deerfield Beach Fla. 2022 Feb;34(6):e2106755.
Chan C, Liu L, Dharmadhikari S, Shontz KM, Tan ZH, Bergman M, et al. A Multimodal Approach to Quantify Chondrocyte Viability for Airway Tissue Engineering. The Laryngoscope [Internet]. [cited 2022 Aug 5];n/a(n/a). Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/lary.30206
Ohno M, Fuchimoto Y, Higuchi M, Yamaoka T, Komura M, Umezawa A, et al. Long-term observation of airway reconstruction using decellularized tracheal allografts in micro-miniature pigs at growing stage. Regen Ther. 2020 Dec;15:64–9.
Martínez-Hernández NJ, Díaz-Cuevas A, Milián-Medina L, Sancho-Tello M, Roselló-Ferrando J, Morcillo-Aixelá A, et al. Decellularized tracheal prelamination implant: A proposed bilateral double organ technique. Artif Organs. 2021 Dec;45(12):1491–500.
Pennarossa G, Ghiringhelli M, Gandolfi F, Brevini TAL. Tracheal In Vitro Reconstruction Using a Decellularized Bio-Scaffold in Combination with a Rotating Bioreactor. Methods Mol Biol Clifton NJ. 2022;2436:157–65.
Young BM, Antczak LAM, Shankar K, Heise RL. A Two-Step Bioreactor for Decellularized Lung Epithelialization. Cells Tissues Organs. 2021;210(4):301–10.
Zhou Q, Ye X, Ran Q, Kitahara A, Matsumoto Y, Moriyama M, et al. Trachea Engineering Using a Centrifugation Method and Mouse-Induced Pluripotent Stem Cells. Tissue Eng Part C Methods. 2018 Sep;24(9):524–33.
Townsend JM, Weatherly RA, Johnson JK, Detamore MS. Standardization of Microcomputed Tomography for Tracheal Tissue Engineering Analysis. Tissue Eng Part C Methods. 2020 Nov;26(11):590–5.
Jin Y, Liu L, Yu P, Lin F, Shi X, Guo J, et al. Emergent Differential Organization of Airway Smooth Muscle Cells on Concave and Convex Tubular Surface. Front Mol Biosci. 2021;8:717771.
Dang LH, Hung SH, Tseng Y, Quang LX, Le NTN, Fang CL, et al. Partial Decellularized Scaffold Combined with Autologous Nasal Epithelial Cell Sheet for Tracheal Tissue Engineering. Int J Mol Sci. 2021 Sep 25;22(19):10322.
Ravindra A, D’Angelo W, Zhang L, Reing J, Johnson S, Myerburg M, et al. Human Bronchial Epithelial Cell Growth on Homologous Versus Heterologous Tissue Extracellular Matrix. J Surg Res. 2021 Jul;263:215–23.
Pouliot RA, Young BM, Link PA, Park HE, Kahn AR, Shankar K, et al. Porcine Lung-Derived Extracellular Matrix Hydrogel Properties Are Dependent on Pepsin Digestion Time. Tissue Eng Part C Methods. 2020 Jun;26(6):332–46.
Pouliot RA, Link PA, Mikhaiel NS, Schneck MB, Valentine MS, Kamga Gninzeko FJ, et al. Development and characterization of a naturally derived lung extracellular matrix hydrogel. J Biomed Mater Res A. 2016 Aug;104(8):1922–35.
de Hilster RHJ, Sharma PK, Jonker MR, White ES, Gercama EA, Roobeek M, et al. Human lung extracellular matrix hydrogels resemble the stiffness and viscoelasticity of native lung tissue. Am J Physiol Lung Cell Mol Physiol. 2020 Apr 1;318(4):L698–704.
Nakamura R, Katsuno T, Tsuji T, Oyagi S, Kishimoto Y, Suehiro A, et al. Airway ciliated cells regenerated on collagen sponge implants acquire planar polarities towards nearby edges of implanted areas. J Tissue Eng Regen Med. 2021 Aug;15(8):712–21.
Chen J, Mir SM, Pinezich MR, O’Neill JD, Guenthart BA, Bacchetta M, et al. Homogeneous Distribution of Exogenous Cells onto De-epithelialized Rat Trachea via Instillation of Cell-Loaded Hydrogel. ACS Biomater Sci Eng. 2022 Jan 10;8(1):82–8.
Liu Y, Dabrowska C, Mavousian A, Strauss B, Meng F, Mazzaglia C, et al. Bio-assembling Macro-Scale, Lumenized Airway Tubes of Defined Shape via Multi-Organoid Patterning and Fusion. Adv Sci Weinh Baden-Wurtt Ger. 2021 May;8(9):2003332.
Zhao Y, Tian C, Wu K, Zhou X, Feng K, Li Z, et al. Vancomycin-Loaded Polycaprolactone Electrospinning Nanofibers Modulate the Airway Interfaces to Restrain Tracheal Stenosis. Front Bioeng Biotechnol. 2021;9:760395.
Tan ZH, Dharmadhikari S, Liu L, Wolter G, Shontz KM, Reynolds SD, et al. Tracheal Macrophages During Regeneration and Repair of Long-Segment Airway Defects. The Laryngoscope. 2022 Apr;132(4):737–46.
Young BM, Shankar K, Allen BP, Pouliot RA, Schneck MB, Mikhaiel NS, et al. Electrospun Decellularized Lung Matrix Scaffold for Airway Smooth Muscle Culture. ACS Biomater Sci Eng. 2017 Dec 11;3(12):3480–92.
Lagowala DA, Kwon S, Sidhaye VK, Kim DH. Human microphysiological models of airway and alveolar epithelia. Am J Physiol Lung Cell Mol Physiol. 2021 Dec 1;321(6):L1072–88.
De Santis MM, Alsafadi HN, Tas S, Bölükbas DA, Prithiviraj S, Da Silva IAN, et al. Extracellular-Matrix-Reinforced Bioinks for 3D Bioprinting Human Tissue. Adv Mater Deerfield Beach Fla. 2021 Jan;33(3):e2005476.
Frejo L, Goldstein T, Swami P, Patel NA, Grande DA, Zeltsman D, et al. A two-stage in vivo approach for implanting a 3D printed tissue-engineered tracheal replacement graft: A proof of concept. Int J Pediatr Otorhinolaryngol. 2022 Apr;155:111066.
Oberoi G, Eberspächer-Schweda MC, Hatamikia S, Königshofer M, Baumgartner D, Kramer AM, et al. 3D Printed Biomimetic Rabbit Airway Simulation Model for Nasotracheal Intubation Training. Front Vet Sci. 2020;7:587524.
Peterson DM, Beal EW, Reader BF, Dumond C, Black SM, Whitson BA. Electrical Impedance as a Noninvasive Metric of Quality in Allografts Undergoing Normothermic Ex Vivo Lung Perfusion. ASAIO J Am Soc Artif Intern Organs 1992. 2022 Jul 1;68(7):964–71.
Antunes MB, Cohen NA. Mucociliary clearance--a critical upper airway host defense mechanism and methods of assessment. Curr Opin Allergy Clin Immunol. 2007 Feb;7(1):5–10.
Safshekan F, Tafazzoli-Shadpour M, Abdouss M, Shadmehr MB. Mechanical Characterization and Constitutive Modeling of Human Trachea: Age and Gender Dependency. Materials. 2016 Jun;9(6):456.
Huang Z, Wang L, Zhang CX, Cai ZH, Liu WH, Li WM, et al. Biomechanical strength dependence on mammalian airway length. J Thorac Dis. 2021 Feb;13(2):918–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Heise, R.L. (2023). Computational, Ex Vivo, and Tissue Engineering Techniques for Modeling Large Airways. In: Magin, C.M. (eds) Engineering Translational Models of Lung Homeostasis and Disease. Advances in Experimental Medicine and Biology, vol 1413. Springer, Cham. https://doi.org/10.1007/978-3-031-26625-6_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-26625-6_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-26624-9
Online ISBN: 978-3-031-26625-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)