Abstract
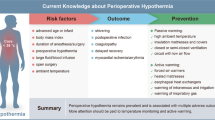
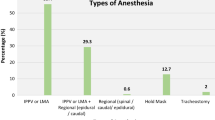
Prevention of intraoperative hypothermia (<36 °C) is a standard of care for all patients undergoing surgery. Patients undergoing both general and regional anesthesia are at risk of hypothermia, which, if it occurs, has well-recognized consequences, including increases in surgical site infections, surgical blood loss and transfusion requirements, cardiac complications, reduced drug metabolism, and prolonged recovery. Two key areas in its prevention are regular accurate core body temperature measurement and the required steps that may be undertaken to prevent further loss and/or allow patient warming, aiming for a target core temperature of at least 36.5 °C. Great care must be taken to ensure that any devices are appropriately serviced, assembled, and used, to minimize accidental thermal injury to patients. Preoperatively, anesthesia should not begin if the patient’s temperature is <36 °C, and they should be actively warmed if from the start of the procedure the duration of anesthesia is expected to be >30 minutes. In the postoperative period, the patient’s temperature should be monitored and actively warmed if their temperature is <36 °C.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Tansey EA, Johnson CD. Recent advances in thermoregulation. Adv Physiol Educ. 2015;39:139–48.
Sessler DI. Perioperative thermoregulation and heat balance. Lancet. 2016;387:2655–64.
Sun Z, Honar H, Sessler DI, Dalton JE, Yang D, Panjasawatwong K, Deroee AF, Salmasi V, Saager L, Kurz A. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015;122:276–85.
Sullivan G, Edmondson C. Heat and temperature. Contin Educ Anaesth Crit Care Pain. 2008;8:104–7.
Luscombe M, Andrzejowski JC. Clinical applications of induced hypothermia. Contin Educ Anaesth Crit Care Pain. 2008;6:23–7.
Lau A, Lowlaavar N, Cooke EM, West N, German A, Morse DJ, Görges M, Merchant RN. Effect of preoperative warming on intraoperative hypothermia: a randomized-controlled trial. Can J Anaesth. 2018;65(9):1029–40.
Leslie K, Sessler DI. Reduction in the shivering threshold is proportional to spinal block height. Anesthesiology. 1996;84:1327–31.
Joris J, Ozaki M, Sessler DI, Hardy AF, Lamy M, McGuire J, et al. Epidural anesthesia impairs both central and peripheral thermoregulatory control during general anesthesia. Anesthesiology. 1994;80:268–77.
Sessler DI. Chapter 48. Temperature regulation and monitoring. In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, editors. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone/Elsevier; 2010. p. 1533–6.
The National Institute for Health and Care Excellence (NICE). Hypothermia: prevention and management in adults having surgery. Clinical guideline (CG65). Last updated December 2016. https://www.nice.org.uk/guidance/cg65. Accessed Oct 2018.
The National Institute for Health and Care Excellence (NICE). Bair Hugger for measuring core temperature during perioperative care. Medtech innovation briefing (MIB99). March 2017. https://www.nice.org.uk/advice/mib99. Accessed Oct 2018.
Eshraghi Y, Nasr V, Parra-Sanchez I, Van Duren A, Botham M, Santoscoy T, et al. An evaluation of a zero-heat-flux cutaneous thermometer in cardiac surgical patients. Anesth Analg. 2014;119:543–9.
Mäkinen MT, Pesonen A, Jousela I, Päivärinta J, Poikajärvi S, Albäck A, Salminen US, Pesonen E. Novel zero-heat-flux deep body temperature measurement in lower extremity vascular and cardiac surgery. J Cardiothorac Vasc Anesth. 2016;30:973–8.
Campbell G, Alderson P, Smith AF, Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2015;(4):CD009891.
John M, Ford J, Harper M. Peri-operative warming devices: performance and clinical application. Anaesthesia. 2014;69:623–38.
Dean M, Ramsay R, Heriot A, Mackay J, Hiscock R, Lynch AC. Warmed, humidified CO2 insufflation benefits intraoperative core temperature during laparoscopic surgery: a meta-analysis. Asian J Endosc Surg. 2017;10(2):128–36.
Birch DW, Dang JT, Switzer NJ, Manouchehri N, Shi X, Hadi G, Karmali S. Heated insufflation with or without humidification for laparoscopic abdominal surgery. Cochrane Database Syst Rev. 2016;(10):CD007821.
Roberson MC, Dieckmann LS, Rodriguez RE, Austin PN. A review of the evidence for active preoperative warming of adults undergoing general anesthesia. AANA J. 2013;81:351–6.
Connelly L, Cramer E, DeMott Q, Piperno J, Coyne B, Winfield C, et al. The optimal time and method for surgical prewarming: a comprehensive review of the literature. J Perianesth Nurs. 2017;32(3):199–209.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fawcett, W.J. (2020). Prevention of Intraoperative Hypothermia. In: Ljungqvist, O., Francis, N., Urman, R. (eds) Enhanced Recovery After Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-33443-7_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-33443-7_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-33442-0
Online ISBN: 978-3-030-33443-7
eBook Packages: MedicineMedicine (R0)