Abstract
Background
An outbreak of coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was first detected in Wuhan, Hubei, China. People of all ages are susceptible to SARS-CoV-2 infection. No information on severe pediatric patients with COVID-19 has been reported. We aimed to describe the clinical features of severe pediatric patients with COVID-19.
Methods
We included eight severe or critically ill patients with COVID-19 who were treated at the Intensive Care Unit (ICU), Wuhan Children’s Hospital from January 24 to February 24. We collected information including demographic data, symptoms, imaging data, laboratory findings, treatments and clinical outcomes of the patients with severe COVID-19.
Results
The onset age of the eight patients ranged from 2 months to 15 years; six were boys. The most common symptoms were polypnea (8/8), followed by fever (6/8) and cough (6/8). Chest imaging showed multiple patch-like shadows in seven patients and ground-glass opacity in six. Laboratory findings revealed normal or increased whole blood counts (7/8), increased C-reactive protein, procalcitonin and lactate dehydrogenase (6/8), and abnormal liver function (4/8). Other findings included decreased CD16 + CD56 (4/8) and Th/Ts*(1/8), increased CD3 (2/8), CD4 (4/8) and CD8 (1/8), IL-6 (2/8), IL-10 (5/8) and IFN-γ (2/8). Treatment modalities were focused on symptomatic and respiratory support. Two critically ill patients underwent invasive mechanical ventilation. Up to February 24, 2020, three patients remained under treatment in ICU, the other five recovered and were discharged home.
Conclusions
In this series of severe pediatric patients in Wuhan, polypnea was the most common symptom, followed by fever and cough. Common imaging changes included multiple patch-like shadows and ground-glass opacity; and a cytokine storm was found in these patients, which appeared more serious in critically ill patients.
Similar content being viewed by others
Introduction
The outbreak of coronavirus disease 2019 (COVID-19, previously known as 2019-nCoV) caused by SARS-CoV-2 infection in Wuhan City, China, has spread around the world [1]. As of 24 February, more than 77,262 confirmed patients have been reported in China, and several patients have been confirmed in 29 countries. Among the confirmed patients in china, 9915 were severe patients and 2592 died [2]. In addition, most of those who died had underlying health conditions such as hypertension, diabetes or cardiovascular disease which compromised their immune system [3].
Previous studies have shown that patients with COVID-19 present with fever, dry cough, dyspnea, fatigue and lymphopenia. SARS-CoV-2 is more likely to infect elderly adult men; and those with chronic comorbidities are at higher risk of severe acute respiratory syndrome and even death in severe patients [4,5,6]. Infected children have relatively milder clinical symptoms compared with infected adults [7], and no deaths have been reported in the pediatric population up to now. Mildly affected pediatric patients have been reported with an age of onset ranging from 17 days to 17 years [8]. However, specific information characterizing severely affected pediatric patients remains unknown.
For better understanding of the clinical features of severe pediatric patients with COVID-19 and for improving the diagnosis and treatment, we aimed to describe epidemiological and clinical features, imaging data, laboratory findings, clinical treatments and outcomes of severely or critically ill pediatric patients with COVID-19 in Wuhan City, China.
Methods
Patients
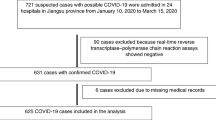
We included eight severely or critically ill patients with COVID-19 who were treated at the Intensive Care Unit (ICU), Wuhan Children’s Hospital from January 24 to February 24. COVID-19 was confirmed in all patients by positive results of real-time reverse transcription-polymerase chain reaction (RT-PCR) assay for nasopharyngeal swab specimens. Clinical staging of the patients was classified according to “Interim Guidance for Diagnosis and Treatment of Coronavirus Disease 2019 (the 6th edition)” released by National Health Commission [9].
Severe COVID-19 was defined when the pediatric patients met any of the following criteria: (1) increased respiratory rate: ≥ 30 times/min; (2) oxygen saturation < 93% under a resting state, and (3) arterial partial pressure of oxygen (PaO2)/oxygen concentration (FiO2) ≤ 300 mmHg (1 mmHg = 0.133 kPa).
Critically ill COVID-19 was defined when the pediatric patients met any of the following criteria: (1) respiratory failure which requires mechanical ventilation; (2) septic shock, and (3) accompanied by other organ failure that needs ICU monitoring and treatment.
Data collection
Demographic information and clinical characteristics including exposure history, anamnesis, signs and symptoms, chest computed tomographic (CT) scan or X-ray results, complications, treatments, clinical outcomes, and laboratory findings of each patient were obtained from the Electronic Medical Record System of Wuhan Children’s Hospital. The dates of patients’ disease onset and hospital admission, incubation period, days from illness onset to diagnosis confirmation, disease duration, as well as history of familial cluster were recorded.
Laboratory tests were conducted upon admission, including a complete blood count (leucocytes, neutrophils, lymphocytes, thrombocyte, hemoglobin), serum biochemistry (C-reactive protein, procalcitonin, lactate dehydrogenase, aspartate aminotransferase, alanine aminotransferase, total bilirubin, creatine kinase, creatinine and D-dimer), TBNK test (CD16 + CD56 + CD3 +, CD4 + T, CD8 + T and Th/Ts), cytokine detection assays (IL-2, IL-4, IL-6, IL-10, TNF-α and IFN-γ) and identification of other respiratory pathogens such as influenza A virus (H1N1, H3N2, H7N9), influenza B virus, respiratory syncytial virus, parainfluenza virus and adenovirus.
Results
Demographic and baseline characteristics
Eight pediatric patients with COVID-19 treated in ICU were included in this study. Among them, three were critically ill patients, and five severely ill. Six were males and two females. The age ranged from 2 months to 15 years (Table 1). Five patients were family-clustered cases and had a close contact history with confirmed or suspected COVID-19 patients; one was infected during hospitalization. The transmission way was still unclear in two patients. The incubation period of four patients ranged from 5 to 10 days. Duration from illness onset to disease confirmation of seven patients ranged from 3 to 15 days. One patient (patient 8) who had a close contact history with infected patients was confirmed by RT-PCR test before symptoms appeared. Disease duration of all patients was over 10 days, and over 20 days in critically ill patients. All children were reported to be living in Wuhan during the outbreak period of COVID-19.
Clinical characteristics and chest imaging results
In the severe pediatric patients, the most common symptom was polypnea (8/8), followed by fever (6/8), cough (6/8), expectoration (4/8), nausea/vomiting (4/8), diarrhea (3/8), fatigue/myalgia (1/8), headache (1/8) and constipation (1/8) (Table 1). Lung auscultation revealed rales in the left or right lower lobe in five patients (5/8) and crackles in the others (3/8).
All patients had remarkable abnormalities in chest (CT) scanning or X-ray (Table 1). Six patients had bilateral pneumonia and two unilateral pneumonia. Imaging changes included multiple patch-like shadows (7/8), ground-glass opacity (GGO) (6/8), pleural effusion (1/8) and "white lung-like" change (1/8). The followings were imaging results of three typical patients.
Patient 1 was an 8-year-old boy, who was infected with COVID-19 when under blood transfusion for treating acute lymphoblastic leukemia during hospitalization. Chest CT demonstrated multiple patch-like shadows (January 31) and high density shadows and GGO (February 13). His condition deteriorated and chest X-rays demonstrated decreased brightness of the lung and "white lung" appearance on February 23 (Fig. 1).
Patient 2 was a 10-month-old infant, who had a close contact with a critically ill COVID-19 patient (her mother). Chest CT demonstrated small dense shadows and pleural effusion on February 4, GGO and consolidation shadow on February 9, and lesions deteriorated on February 12. Chest X-rays obviously improved until February 22 (Fig. 2).
Patient 6 was a 15-year-old girl, who had a close contact with a confirmed COVID-19 patient. Chest CT demonstrated multiple patch-like shadows and GGO bilateral both lungs (February 14), which was obviously improved on February 18 (Fig. 3).
Septic shock and multiple organ dysfunction syndrome (MODS) were the most common complications in critically ill patients. Patient 2 was complicated with septic shock, MODS, intussusception, toxic encephalopathy, status epilepticus and disseminated intravascular coagulation (DIC). Patient 3 was complicated with septic shock, MODS, kidney stone, hydronephrosis, cardiac insufficiency and coagulopathy. Patients 4 and 5 were complicated with hypoglobulinemia and gastroenteritis.
Laboratory assessments
COVID-19 was confirmed in all patients by RT-PCR. In this cohort (except patient 1 who had acute lymphocytic leukemia), leucocytes, neutrophils, lymphocytes, thrombocyte and hemoglobin counts were all normal or mildly increased (Table 2). Neutrophils, lymphocytes and hemoglobin were decreased in patient 1. Patient 1 was also infected with Influenza A virus. Increased C-reactive protein, procalcitonin and lactate dehydrogenase were found in five patients (5/8), and increased alanine aminotransferase (ALT) in four (4/8). Total bilirubin level in all patients was normal. Creatine kinase level decreased in one patient and increased in two; patient 2 had a far higher bilirubin level (20,702 U/L) than normal (normal range: 30–170 U/L). Creatinine level decreased in three patients and increased in two patients. Two patients (2/5) had high D-dimer level. TBNK lymphocyte subset analysis revealed decreased percentage of CD16 + CD56 + lymphocytes (4/8) and Th/Ts (1/8), and increased percentage of CD3 + (2/8), CD4 + (4/8) and CD8 + (1/8) lymphocytes. Cytokine detection assays showed increased levels of IL-6 (2/8), IL-10 (5/8) and IFN-γ (2/8).
Clinical treatment and outcomes
Treatments of COVID-19 remained focusing on symptomatic and respiratory supports (Table 3). Among the eight patients, six (6/8) received high-flow oxygen therapy and two critically ill (2/8) patients received mechanical ventilation. All patients received antiviral treatments (virazole, oseltamivir and interferon). Antibiotics, traditional Chinese medicine, intravenous glucocorticoids and immunoglobulin were also used dependent on patients’ conditions. Symptomatic treatments were given for treating complications in patient 2 and 3. Up to February 24, 2020, three patients (patients 1, 2 and 8) remained in ICU (including two critically ill patients); the others recovered and were discharged home.
Discussion
Since December, 2019, COVID-19 caused by SARS-CoV-2 infection has spread rapidly around China and the world [5, 10,11,12]. SARS-CoV-2 is a coronavirus that belongs to the β-coronavirus cluster, which can cause the third known zoonotic coronavirus disease after severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [13]. It has been reported that SARS-CoV-2 uses the same cell entry receptor (ACE2) to infect humans, as SARS-CoV, but the clinical features of COVID-19 seem to be more variable [3]. The number of COVID-19 patients currently exceeds SARS and MERS; however, most patients are infected mildly, and the overall case-fatality rate (CFR) was 2.3% (1023 deaths among 44,672 confirmed patients) [14], much lower than that of SARS (10%) and MERS (37%) [3, 15, 16].
In the early reports, all of the patients were adults (middle-aged and elderly) in Wuhan [5]. On entering the outbreak stage and improvement of pathogen detection, pediatric patients (even newborns) have been reported increasingly [17, 18]. According to the latest report from the Chinese Center for Disease Control and Prevention (CCDC), 965 confirmed patients under age 19 years (2.16%, 965/44,672) were reported nationwide [14]; no deaths have occurred in the group aged 9 years and younger, as of February 11. Children have special immune response system which is distinct from adults [19]; therefore, pediatric patients with COVID-19 have their own clinical features and therapeutic responses [20]. To our knowledge, this is the first report on pediatric patients with severe COVID-19.
The patients age ranged from 2 months to 15 years, and mostly were males (75%). Males seemed to be more susceptible to SARS-CoV-2 infection, which was similar to previous reports [5, 21,22,23]. Five patients (62.5%) were infected due to close contacts with family members confirmed with COVID-19; therefore, family daily prevention is an important way to prevent COVID-19. Disease duration is relative to the severity of the disease. Severely affected patients had a disease duration of over 10 days, but critically ill patients had a duration of over 20 days (two remained in ICU after over 20 days of treatment).
In our cohort, the most common symptoms were polypnea (100%), fever (75%), cough (75%), expectoration (50%) and nausea/vomiting (50%). Fatigue/myalgia and headache, commonly described in adults, were rarely described in children. The reason may be that these symptoms are difficult to be described by young children. Half of our patients were infants or young children, who were unable to speak or speak clearly. So more data on clinical features of pediatric patients need to be studied. The ratio of patients with fever in this cohort of severe patients was lower than that of critically ill adult patients. Among the 52 critically ill adult patients reported by Yang et al. [22], common symptoms were fever (98%), cough (77%) and dyspnoea (63.5%). Nevertheless, the ratio of patients with fever in this series was higher than those children not treated in ICU. Among the 34 infected children (most are mild patients) reported by Wang et al. [24], fever (50%) and cough (38%) were the most common symptoms. According to our results, polypnea should be highlighted in severe pediatric patients, even without fever.
Infected patients who develop acute respiratory distress syndrome (ARDS) may present with characteristic pulmonary ground-glass changes on imaging [4, 6, 12, 25]. The CT images of our patients mainly showed multiple patch-like shadows and ground glass opacity, consistent with previous reports. Chest X-rays of patient 1 who remains in ICU demonstrate decreased brightness of the lung and "white lung-like" changes. This patient is still under intensive treatment and close monitoring.
Septic shock and MODS were common complications in critically ill patients. Multi-organ involvements were found in critically ill patients including the nervous, blood, urinary and cardiac systems. Complications were relatively mild in severe patients in our cohort, such as hypoglobulinemia and gastroenteritis.
The treatment modalities of COVID-19 infection were mainly symptomatic and respiratory supporting. High-flow oxygen therapy, invasive ventilation and antiviral treatments (virazole, oseltamivir and interferon) were given to the patients. Antibiotic therapy, traditional Chinese medicine, intravenous glucocorticoid and immunoglobulin therapies were also used according to the patients’ conditions. Up to February 24, 2020, three patients remained in ICU (including two critically ill patients), the others recovered and were discharged without death. The overall case fatality rate of severe pediatric patients is far lower than those of adults (49.0%, 1023/2087) [14], which indicates a better clinical outcome in pediatric patients.
Leucocytes, neutrophils, lymphocytes, thrombocyte and hemoglobin counts were normal or mildly increased in severe patients. Among critically ill patients, patient 1 with acute lymphocytic leukemia, undergoing blood transfusion, showed low level of neutrophils, lymphocytes and hemoglobin; patient 2 with serious complications (septic shock, DIC, MODS) showed high level of leucocytes and neutrophils and low level of thrombocyte and hemoglobin. Blood purification and transfusion were performed to improve symptoms. Elevated C-reactive protein, lactate dehydrogenase, procalcitonin, ALT and D-dimer were also discovered in the cohort. The level of creatine kinase was significantly high in patient 2, which required high attention.
Coronaviruses of COVID-19, SARS and MERS can induce excessive and aberrant non-effective host immune responses that are associated with severe lung pathology. The lung injury is more pronounced in critically ill patients, associated with a cytokine storm, which is characterized by increased plasma concentrations of pro-inflammatory cytokines (IL-1β, IL-6, IL-12, TNF, IFN-γ) and anti-inflammatory cytokines (IL-4, IL-10, IL-13, TGF-β) [5, 6, 26,27,28,29]. In our cohort, decreased CD16 + CD56+ lymphocytes and increased IL-6, IL-10 and IFN-γ were observed. The levels of IL-6 and IL-10 were significantly increased in two critically ill patients, who remained in ICU with disease durations of over 20 days. More abnormalities in cytokine spectrum were seen in critically ill patients than in severe patients. Huang et al. [5] also found that COVID-19 patients in ICU had higher plasma levels of IL-2, IL-7, IL-10, GSCF, IP10, MCP1, MIP1A, and TNF-α, compared with non-ICU patients. Conversely, severe SARS patients had very low levels of IL-10 [30]. Different inflammatory responses were found between SARS and COVID-19, so more researches are needed. In addition, the level of CD4 increased, which indicating overactivation of the immune system leading to fatal immune disorders.
In conclusion, for severe or critically ill pediatric patients who survive intensive care, a number of specific laboratory abnormalities and aberrant and excessive immune responses may lead to long-term lung damage and severe health complications. Therefore, early identification of the specific features of severe pediatric patients and timely treatment are of crucial importance.
References
Shen KL, Yang YH. Diagnosis and treatment of 2019 novel coronavirus infection in children: a pressing issue. World J Pediatr. 2020. https://doi.org/10.1007/s12519-020-00344-6(epub ahead of print).
National Health Commission of People's Republic of China. http://en.nhc.gov.cn/2020-02/24/c_76911.htm. Accessed 24 Feb 2020
Chen J. Pathogenicity and transmissibility of 2019-nCoV—a quick overview and comparison with other emerging viruses. Microbes Infect. 2020. https://doi.org/10.1016/j.micinf.2020.01.004(epub ahead of print).
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected by SARS-CoV-2 in Wuhan, China. Allergy. 2020. https://doi.org/10.1111/all.14238(epub ahead of print).
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–13.
Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4.
Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020. https://doi.org/10.1001/jama.2020.2131(epub ahead of print).
National Health Commission. Diagnosis and treatment of pneumonia caused by 2019-nCoV (trial version 6). https://baijiahao.baidu.com/s?id=1658945855347500695&wfr=spider&for=pc. Accessed 18 Feb 2020
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020. https://doi.org/10.1056/NEJMoa2001316(epub ahead of print).
Liu T, Hu J, Kang M, Lin L, Zhong H, Xiao J, et al. Transmission dynamics of 2019 novel coronavirus (2019-nCoV). BioRxiv. 2020. https://doi.org/10.1101/2020.01.25.919787.
Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020;9:575.
Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020. https://doi.org/10.1002/jmv.25722(epub ahead of print).
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020. https://doi.org/10.1001/jama.2020.2648(epub ahead of print).
Mahase E. Coronavirus: covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641.
de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–34.
Zhang YH, Lin DJ, Xiao MF, Wang JC, Wei Y, Lei ZX, et al. 2019-novel coronavirus infection in a three-month-old baby. Zhonghua Er Ke Za Zhi. 2020;58:E006 (in Chinese).
Pediatric Branch of Hubei Medical Association; Pediatric Branch of Wuhan Medical Association; Pediatric Medical Quality Control Center of Hubei. Recommendation for the diagnosis and treatment of novel coronavirus infection in children in Hubei (trial version 1). Zhongguo Dang Dai Er Ke Za Zhi. 2020;22:96–9 (in Chinese).
Valiathan R, Ashman M, Asthana D. Effects of ageing on the immune system: infants to elderly. Scand J Immunol. 2016;83:255–66.
Chen ZM, Fu JF, Shu Q. New coronavirus: new challenges for pediatricians. World J Pediatr. 2020. https://doi.org/10.1007/s12519-020-00346-4(epub ahead of print).
Ki M, TFF-nCoV. Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-nCoV) disease in republic of Korea. Epidemiol Health. 2020. https://doi.org/10.4178/epih.e2020007(epub ahead of print).
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020. https://doi.org/10.1016/S2213-2600(20)30079-5(epub ahead of print).
Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606.
Wang XF, Yuan J, Zheng YJ, Chen J, Bao YM, Wang YR, et al. Clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen. Zhonghua Er Ke Za Zhi. 2020;58:E008 (in Chinese).
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585(epub ahead of print).
Zumla A, Hui DS, Azhar EI, Memish ZA, Maeurer M. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet. 2020;395:e35–6.
Hui DSC, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin N Am. 2019;33:869–89.
Azhar EI, Hui DSC, Memish ZA, Drosten C, Zumla A. The Middle East respiratory syndrome (MERS). Infect Dis Clin N Am. 2019;33:891–905.
Li G, Fan Y, Lai Y, Han T, Li Z, Zhou P, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92:424–32.
Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–39.
Acknowledgements
We would like to thank the parents and children for participating in the study. We thank the doctors and nursing staff of Intensive Care Unit for their detailed assessments and dedicated care of these young patients.
Funding
None.
Author information
Authors and Affiliations
Contributions
DS and HL contributed equally to this paper. DS, HL, XXL, HX and JR collected and analyzed data and drafted the first manuscript. F-RZ and Z-SL designed the project and revised the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Wuhan Children’s Hospital. Informed consents for publication have been obtained from parents or guardians of patients.
Conflict of interest
All the authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, D., Li, H., Lu, XX. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J Pediatr 16, 251–259 (2020). https://doi.org/10.1007/s12519-020-00354-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-020-00354-4