Abstract
Objective
To study the clinical presentation, management, and results of treatment of 41 consecutive cases of choledochal cyst (CC) managed from 1999 to 2006.
Methods
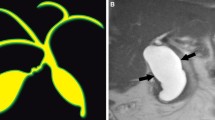
The age of the patients ranged from 20 days to 11 years. Eleven cases were 1 year or less in age (infantile group), and 30 patients were more than 1 year old (classical pediatric group). Children less than 1 year old presented with jaundice (72%), hepatomegaly (54%) and clay-colored stools (63%); whereas those above one year in age presented with pain (83.3%) and jaundice (47.6%). Three cases had biliary perforation with localized or generalized biliary peritonitis. Ultrasonography (US) diagnosed/suggested CC in all 41 patients, however, contrast-enhanced computed tomographic (CECT) scan (n=12), radionuclide DISIDA scan (n=5), and magnetic resonance cholangiopancreatogram (MRCP) (n=3) also contributed to the diagnosis. 19 patients, including 4 from the ‘infantile’ group, had significant dilatation of intrahepatic biliary ducts.
Results
Nine patients from the ‘infantile’ group had cystic type I CC (type Ic), while 2 patients had fusiform dilatation of the common bile duct (type if disease). In contrast, 21 of the older patients had type If disease while 9 had type Ic disease. Operative management included primary complete excision of the cyst with a Roux-en-Y hepaticodochojejunostomy (HDJ) (n=32), Lilly’s modification of submucosal resection with a HDJ (n=8), and cyst excision with a hepaticodochoduodenostomy (HDD) (n=1). All 3 patients with biliary perforation had primary excision of the CC with a HDJ. Unusual operative findings included accessory hepatic ducts (n=2), anteriorly placed common or right hepatic arteries (n=3), and partially or completely blocked proximal extrahepatic bile ducts (n=3). There were 2 postoperative deaths, one had cirrhotic liver disease with portal hypertension, the other had deep icterus with poor general condition. Both patients succumbed to overwhelming sepsis. One patient required reexploration and refashioning of the HDJ for biliary leak. Short-term follow-up was satisfactory in all 39 patients.
Conclusion
Infants with CC constitute a distinct group with regard to clinical presentation and the pathological anatomy. CC should be kept in mind while evaluating neonates and infants with cholestatic jaundice, and older children with recurrent abdominal pain. Primary excision of the cyst with a HDJ provides satisfactory results in the management of the vast majority of cases of CC including those in infants, massive CC, and in the presence of biliary perforation and peritonitis.
Similar content being viewed by others
References
Howard ER. Choledochal cysts. In Howard ER, ed. Surgery of liver disease in children. Oxford; Butterworth-Hienemann, 1991; 78–90.
Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg 2000; 9: 187–195.
Mukhopadhyay B, Bommayya N, Mukhopadhyay M et al. Choledochal cyst-experience in five years. Journal Indian Assoc Pediatr Surg 1999; 4: 118–122.
Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts: lessons from a 20 year experience. Archives Dis Childhood 1995; 73: 528–531.
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Classification, operative procedures and review of thirty seven cases including cancer arising from choledochal cyst. Am J Surg 1977; 134: 263–269.
Lilly JR. Total excision of choledochal cyst. Surg Gynaecol Obstet 1978; 146: 254–256.
O’Neill, Jr. JA. Choledochal cyst. In O’Neill, Jr. JA, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG. eds. Pediatric Surgery, 5th ed Vol. 2, St. Louis, Missouri; Mosby-Year Book, Inc, 1998; 1483–1494.
Vijayaraghavan P, Lal R, Sikora SS, Poddar U, Yachha SK. Experience with choledochal cysts in infants. Pediatr Surg Int 2006; 22: 803–807.
Joseph VT. Surgical techniques and long-term results in the treatment of choledochal cyst. J Pediatr Surg 1990; 25: 782–787.
Le L, Pham AV, Dessanti A. Congenital dilatation of extrahepatic bile ducts in children. Experience in the central hospital of Hue, Vietnam. Eur J Pediatr Surg 2006; 16: 24–27.
Suzuki M, Shimizu T, Kudo T et al. Usefulness of nonbreath-hold 1-shot magnetic resonance cholangiopancreatography for the evaluation of choledochal cyst in children. J Pediatr Gastroenterol Nutr 2006; 42: 539–544.
Sarin YK. Biliary ductal and vascular anomalies associated with choledochal cyst. J Indian Ass Pediatric Surgeons 2005; 10: 86–88.
Narasimhan KL, Chaudhury SK, Rao KLN. Management of accessory hepatic ducts in choledochal cyst. J Pediatr Surg 2001; 7: 1092–1093.
Muise AM, Turner D, Wine E, Kim P, Marcon M, Ling SC. Biliary atresia with choledochal cyst: implications for classification. Clin Gastroenterol Hepatol 2006; 4: 1411–1414.
Koshinaga T, Wakabayashi K, Inoue M et al. Pancreatitis after a primary and secondary excision of choledochal cysts. Surg Today 2006; 36: 686–691.
Martinez-Ferro M, Esteves E, Laje P. Laparoscopic treatment of biliary atresia and choledochal cyst. Semin Pediatr Surg 2005; 14: 206–215.
Srimurthy KR, Ramesh S, Babu N. Laparoscopic correction of choledochal cyst in 10 children. Paper presented at the 30th Annual Conference of the Indian Association of Pediatric Surgeons, 28th–31st October, 2004, at Jabalpur, India.
Li L, Feng W, Jing-Bo F et al. Laparoscopic-assisted total cyst excision of choledochal cyst and Roux-en-Y hepatoenterostomy. J Pediatr Surg 2004; 39: 1663–1666.
Todani T, Watanabe Y, Mizuguchi T et al. Hepaticoduodenostomy at the hepatic hilum after excision of choledochal cyst. Am J Surg 1981; 142: 584–587.
Shimotakahara A, Yamataka A, Yanai T et al. Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy for biliary reconstruction during the surgical treatment of choledochal cyst: which is better? Pediatr Surg Int 2005; 21: 5–7.
Takada K, Hamada Y, Watanabe K, Tanano A, Tokuhara K, Kamiyama Y. Duodenogastric reflux following biliary reconstruction after excision of choledochal cyst. Pediatr Surg Int 2004; 21: 1–4.
Morotomi Y, Todani T, Watanabe Y, Noda T, Otsuka K. Modified Kasai’s procedure for a choledochal cyst with a very narrow hilar duct. Pediatr Surg Int 1995; 11: 58–59.
Karnak I, Tanyel FC, Buyukpamucku N, Hicsonmez A. Spontaneous rupture of choledochal cyst: an unusual cause of acute abdomen in children. J Pediatr Surg 1997; 32: 736–738.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mishra, A., Pant, N., Chadha, R. et al. Choledochal cysts in infancy and childhood. Indian J Pediatr 74, 937–942 (2007). https://doi.org/10.1007/s12098-007-0173-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-007-0173-0