Abstract
Objective
This study assessed whether early levels of biomarkers measured in CSF within 24-h of severe TBI would improve the clinical prediction of 6-months mortality.
Methods
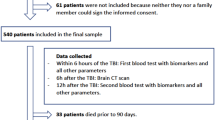
This prospective study conducted at two Level 1 Trauma Centers enrolled adults with severe TBI (GCS ≤8) requiring a ventriculostomy as well as control subjects. Ventricular CSF was sampled within 24-h of injury and analyzed for seven candidate biomarkers (UCH-L1, MAP-2, SBDP150, SBDP145, SBDP120, MBP, and S100B). The International Mission on Prognosis and Analysis of Clinical Trials in TBI (IMPACT) scores (Core, Extended, and Lab) were calculated for each patient to determine risk of 6-months mortality. The IMPACT models and biomarkers were assessed alone and in combination.
Results
There were 152 patients enrolled, 131 TBI patients and 21 control patients. Thirty six (27 %) patients did not survive to 6 months. Biomarkers were all significantly elevated in TBI versus controls (p < 0.001). Peak levels of UCH-L1, SBDP145, MAP-2, and MBP were significantly higher in non-survivors (p < 0.05). Of the seven biomarkers measured at 12-h post-injury MAP-2 (p = 0.004), UCH-L1 (p = 0.024), and MBP (p = 0.037) had significant unadjusted hazard ratios. Of the seven biomarkers measured at the earliest time within 24-h, MAP-2 (p = 0.002), UCH-L1 (p = 0.016), MBP (p = 0.021), and SBDP145 (0.029) had the most significant elevations. When the IMPACT Extended Model was combined with the biomarkers, MAP-2 contributed most significantly to the survival models with sensitivities of 97–100 %.
Conclusions
These data suggest that early levels of MAP-2 in combination with clinical data provide enhanced prognostic capabilities for mortality at 6 months.




Similar content being viewed by others
References
Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 2010;25(2):72–80.
Faul M, Xu L, Wald MM, et al. Traumatic Brain Injury in the United States. In: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010.
Gaetz M. The neurophysiology of brain injury. Clin Neurophysiol. 2004;115(1):4–18.
Pineda JA, Wang KK, Hayes RL. Biomarkers of proteolytic damage following traumatic brain injury. Brain Pathol. 2004;14(2):202–9.
Haskins WE, Kobeissy FH, Wolper RA, et al. Rapid discovery of putative protein biomarkers of traumatic brain injury by SDS-PAGE-capillary liquid chromatography-tandem mass spectrometry. J Neurotrauma. 2005;22(6):629–44.
MisslerU. S-100 protein and neuron-specific enolase concentrations in blood as indicators of infarction volume and prognosis in acute ischemic stroke. Stroke. 1997;28:1956–60.
Ytrebo LMNG, Korvald C, et al. Renal elimination of protein S-100beta in picgs with acute encephalopathy. Scand J Clin Lab Invest. 2001;61:217–25.
Jonsson HJP, Hoglund P, Alling C, Blomquist S. The elimination of S-100b and renal function after cardiac surgery. J Cardiothorac Vasc Aneth. 2000;14:698–701.
Usui AKK, Abe T, Murase M, Tanaka M, Takeuchi E. S-100ao protein in blood and urine during open-heart surgery. Clin Chem. 1989;35:1942–4.
Raabe A, Grolms C, Seifert V. Serum markers of brain damage and outcome prediction in patients after severe head injury. Br J Neurosurg. 1999;13(1):56–9.
Haimoto H, Hosoda S, Kato K. Differential distribution of immunoreactive S100-a and S100-b proteins in normal nonnervous human tissues. Lab Invest. 1987;57:489–98.
Woertgen C, Rothoerl RD, Holzschuh M, et al. Comparison of serial S-100 and NSE serum measurements after severe head injury. Acta Neurochir (Wien). 1997;139(12):1161–4 discussion 1165.
Romner B, Ingebrigtsen T, Kongstad P, et al. Traumatic brain damage: serum S-100 protein measurements related to neuroradiological findings. J Neurotrauma. 2000;17(8):641–7.
Korfias S, Stranjalis G, Boviatsis E, et al. Serum S-100B protein monitoring in patients with severe traumatic brain injury. Intensive Care Med. 2007;33(2):255–60.
Vos PE, Jacobs B, Andriessen TM, et al. GFAP and S100B are biomarkers of traumatic brain injury: an observational cohort study. Neurology. 2010;75(20):1786–93.
Berger RP, Pierce MC, Wisniewski SR, et al. Serum S100B concentrations are increased after closed head injury in children: a preliminary study. J Neurotrauma. 2002;19(11):1405–9.
Bw M. A soluble protein characteristic of the nervous system. Biochem Biophys Res Commun. 1965;19:739–44.
Donato R. Functional roles of S100 proteins, calcium-binding proteins of the EF-hand type. Biochim Biophys Acta. 1999;1450:191–231.
Cooper E. Neuron-specific enolase. Int J Biol Markers. 1994;4:205–10.
Yamazaki Y, Yada K, Morii S, et al. Diagnostic significance of serum neuron-specific enolase and myelin basic protein assay in patients with acute head injury. Surg Neurol. 1995;43(3):267 discussion 270–261.
de Kruijk JR, Leffers P, Menheere PP, et al. S-100B and neuron-specific enolase in serum of mild traumatic brain injury patients. A comparison with health controls. Acta Neurol Scand. 2001;103(3):175–9.
Naeimi ZS, Weinhofer A, Sarahrudi K, et al. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj. 2006;20(5):463–8.
Berger RP, Adelson PD, Pierce MC, et al. Serum neuron-specific enolase, S100B, and myelin basic protein concentrations after inflicted and noninflicted traumatic brain injury in children. J Neurosurg. 2005;103(1 Suppl):61–8.
Wang KK, Ottens AK, Liu MC, et al. Proteomic identification of biomarkers of traumatic brain injury. Expert Rev Proteomics. 2005;2(4):603–14.
Berger RP, Beers SR, Richichi R, et al. Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J Neurotrauma. 2007;24(12):1793–801.
Beers SR, Berger RP, Adelson PD. Neurocognitive outcome and serum biomarkers in inflicted versus non-inflicted traumatic brain injury in young children. J Neurotrauma. 2007;24(1):97–105.
Pineda JA, Lewis SB, Valadka AB, et al. Clinical significance of alphaII-spectrin breakdown products in cerebrospinal fluid after severe traumatic brain injury. J Neurotrauma. 2007;24(2):354–66.
Brophy GM, Pineda JA, Papa L, et al. alphaII-Spectrin breakdown product cerebrospinal fluid exposure metrics suggest differences in cellular injury mechanisms after severe traumatic brain injury. J Neurotrauma. 2009;26(4):471–9.
Mondello S, Robicsek SA, Gabrielli A, et al. alphaII-spectrin breakdown products (SBDPs): diagnosis and outcome in severe traumatic brain injury patients. J Neurotrauma. 2010;27(7):1203–13.
Berger RP, Hayes RL, Richichi R, et al. Serum concentrations of ubiquitin C-terminal hydrolase-L1 and alphaII-spectrin breakdown product 145 kDa correlate with outcome after pediatric TBI. J Neurotrauma. 2012;29(1):162–7.
Siman R, Toraskar N, Dang A, et al. A panel of neuron-enriched proteins as markers for traumatic brain injury in humans. J Neurotrauma. 2009;26(11):1867–77.
Papa L, Akinyi L, Liu MC, et al. Ubiquitin C-terminal hydrolase is a novel biomarker in humans for severe traumatic brain injury. Crit Care Med. 2010;38(1):138–44.
Brophy GM, Mondello S, Papa L, et al. Biokinetic Analysis of Ubiquitin C-Terminal Hydrolase-L1 (UCH-L1) in Severe Traumatic Brain Injury Patient Biofluids. J Neurotrauma. 2011;28(6):861–70.
Papa L, Lewis LM, Silvestri S, et al. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J Trauma Acute Care Surg. 2012;72(5):1335–44.
Mondello S, Gabrielli A, Catani S, et al. Increased levels of serum MAP-2 at 6-months correlate with improved outcome in survivors of severe traumatic brain injury. Brain Inj. 2012;26(13–14):1629–35.
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5(8):e165 discussion e165.
Zhang Z, Mondello S, Kobeissy FH, et al. Protein biomarkers for traumatic and ischemic brain injury: from Bench to Bedside. Transl Stroke Res. 2011;2(4):455–62.
Papa L, Robinson G, Oli M, et al. Use of Biomarkers for Diagnosis and Management of Traumatic Brain Injury Patients. Expert Opin Med Diagn. 2008;2(8):937–45.
Papa L. Exploring the Role of Biomarkers for the Diagnosis and Management of Traumatic Brain Injury Patients. In: Man TK, Flores RJ, editors. Proteomics - Human Diseases and Protein Functions. 1st ed. Veinna: In Tech Open Access Publisher; 2012.
Perel P, Arango M, Clayton T, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336(7641):425–9.
Xiong H, Liang WL, Wu XR. Pathophysiological alterations in cultured astrocytes exposed to hypoxia/reoxygenation. Sheng Li Ke Xue Jin Zhan. 2000;31(3):217–21.
Goodman SR, Zimmer WE, Clark MB, et al. Brain spectrin: of mice and men. Brain Res Bull. 1995;36(6):593–606.
Riederer BM, Zagon IS, Goodman SR. Brain spectrin(240/235) and brain spectrin(240/235E): two distinct spectrin subtypes with different locations within mammalian neural cells. J Cell Biol. 1986;102(6):2088–97.
Wang KK, Posmantur R, Nath R, et al. Simultaneous degradation of alphaII- and betaII-spectrin by caspase 3 (CPP32) in apoptotic cells. J Biol Chem. 1998;273(35):22490–7.
McGinn MJ, Kelley BJ, Akinyi L, et al. Biochemical, structural, and biomarker evidence for calpain-mediated cytoskeletal change after diffuse brain injury uncomplicated by contusion. J Neuropathol Exp Neurol. 2009;68(3):241–9.
Jackson P, Thompson RJ. The demonstration of new human brain-specific proteins by high-resolution two-dimensional polyacrylamide gel electrophoresis. J Neurol Sci. 1981;49(3):429–38.
Czeiter E, Mondello S, Kovacs N, et al. Brain injury biomarkers may improve the predictive power of the IMPACT outcome calculator. J Neurotrauma. 2012;29(9):1770–8.
da Rocha AB, Schneider RF, de Freitas GR, et al. Role of serum S100B as a predictive marker of fatal outcome following isolated severe head injury or multitrauma in males. Clin Chem Lab Med. 2006;44(10):1234–42.
Chen LJ, Wang YJ, Tseng GF. Compression alters kinase and phosphatase activity and tau and MAP2 phosphorylation transiently while inducing the fast adaptive dendritic remodeling of underlying cortical neurons. J Neurotrauma. 2010;27(9):1657–69.
Diez-Guerra FJ, Avila J. Rapid dephosphorylation of microtubule-associated protein 2 in the rat brain hippocampus after pentylenetetrazole-induced seizures. Eur J Biochem. 1993;215(1):181–7.
Posmantur RM, Kampfl A, Taft WC, et al. Diminished microtubule-associated protein 2 (MAP2) immunoreactivity following cortical impact brain injury. J Neurotrauma. 1996;13(3):125–37.
Kobeissy FH, Ottens AK, Zhang Z, et al. Novel differential neuroproteomics analysis of traumatic brain injury in rats. Mol Cell Proteomics. 2006;5(10):1887–98.
Khan SH, Kureshi IU, Mulgrew T, et al. Comparison of percutaneous ventriculostomies and intraparenchymal monitor: a retrospective evaluation of 156 patients. Acta Neurochir Suppl. 1998;71:50–2.
Iberti TJ, Leibowitz AB, Papadakos PJ, et al. Low sensitivity of the anion gap as a screen to detect hyperlactatemia in critically ill patients. Crit Care Med. 1990;18(3):275–7.
Hunter CL, Silvestri S, Dean M, et al. End-tidal carbon dioxide is associated with mortality and lactate in patients with suspected sepsis. Am J Emerg Med. 2013;31(1):64–71.
Lingsma HF, Roozenbeek B, Li B, et al. Large between-center differences in outcome after moderate and severe traumatic brain injury in the international mission on prognosis and clinical trial design in traumatic brain injury (IMPACT) study. Neurosurgery. 2011;68(3):601–7 discussion 607–608.
Ferguson I, Lewis L, Papa L. Neuronal Biomarkers may require age-adjusted norms. Ann Emerg Med. 2011;58(4):S213.
Liu MC, Akinyi L, Scharf D, et al. Ubiquitin C-terminal hydrolase-L1 as a biomarker for ischemic and traumatic brain injury in rats. Eur J Neurosci. 2010;31(4):722–32.
Mondello S, Papa L, Buki A, et al. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Crit Care. 2011;15(3):R156.
Mondello S, Gabrielli A, Catani S, et al. Increased levels of serum MAP-2 at 6 months correlate with improved outcome in survivors of severe traumatic brain injury. Brain Inj. 2012;26(13-14):1629–35.
Dutta S, Chiu YC, Probert AW, et al. Selective release of calpain produced alphalI-spectrin (alpha-fodrin) breakdown products by acute neuronal cell death. Biol Chem. 2002;383(5):785–91.
Nath R, Davis M, Probert AW, et al. Processing of cdk5 activator p35 to its truncated form (p25) by calpain in acutely injured neuronal cells. Biochem Biophys Res Commun. 2000;274(1):16–21.
Conflict of interest
Drs. Gabrielli, Hannay, Heaton, Robertson, Robicsek, and Schmalfuss have no competing financial interests.
Fundings
This study was funded by NIH RO1 NS052831 “Biochemical Markers of Severe Traumatic Brain Injury”. Drs. Brophy and Papa are consultants of Banyan Biomarkers, Inc. but receive no stocks or royalties from the company and will not benefit financially from this publication. Dr. Hayes and Wang own stock, receive royalties from Banyan Biomarkers Inc., and as such may benefit financially as a result of the outcomes of this research or work reported in this publication.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
See Table 7.
Ubiquitin C-terminal Hydrolase (UCH-L1)
UCH-L1 sandwich ELISA (swELISA) was performed in accordance with previously published studies [29, 32–34, 58–60]. Both mouse monoclonal antibody (capture antibody) and rabbit polyclonal antibody (detection antibody) were made in-house at Banyan Biomarkers Inc. against recombinant human UCH-L1 full-length protein and protein A purified. Plates were coated with capture antibody in 0.05 M sodium bicarbonate, pH 9.6 overnight at 4 °C. Blocking and washing buffer was Tris buffered saline with 0.05 % Tween-20 (v/v) (TBST). Antigen standard (UCH-L1 standard curve: 0.78–200 ng/mL; unknown samples: 10 µL of CSF) were incubated with detection antibody overnight and then added to the plate for 2 h. After washing, secondary anti-rabbit-IgG HRP (GE Healthcare) was added and incubated for 1 h. Plates were developed with substrate solution Ultra-TMB ELISA (Pierce# 34,028), stopped with acidic solution and read at 450 nm with a spectrophotometer (Molecular Device SpectraMax 190). The interassay CV was 2–8 % while intraassay CV was 2–11 % within the dynamic range. The limit of detection (LOD) was 0.03 ng/mL.
αII-Spectrin Breakdown Products 150 kDa (SBDP150), 145 kDa (SBDP145), 120 kDa (SBDP120)
SBDP150, SBDP145 and SBDP120 swELISAs were constructed similarly to those described previously [29]. Briefly, a 96-well plate was coated with 100 μL/well capture antibody (5ug/ml purified goat polyclonal anti-SBDP150 [28, 61] or 10ug/ml rabbit anti-SBDP145 or 10ug/ml anti-SBDP120 [62] overnight at 4 °C. Antigen used was partially purified human brain αII-spectrin for SBDP150 or recombinant glutathione-S-transferase– αII-spectrin (including the SBDP145 cleavage site in repeat 13–18) fusion protein cleaved with either calpain-1 (1: 40 ratio for 10 min at 4C) for SBDP145 production or with caspase-3 (1 : 20 ratio for 4 h at room temperature) for SBDP120. After blocking buffer (Startingblock T20-PBS), SBDP150 calibrator (10 × dilution factor, 1.17 ng/ml–300 ng/ml), SBDP145 calibrator (10X dilution factor, 1–500 ng/ml) and SBDP120 Calibrators (3X dilution factor, 0.9–120 ng/mL) or samples were added (CSF, 10 μL for SBDP150, SBDP145; 34 uL for SBDP120) with diluent (total volume 100 uL) to the wells. After washing, plates were incubated with affinity purified detection antibody (mouse monoclonal anti-αII-spectrin antibody (Biomol FG6090 or equivalent). If amplification was needed, biotinyl-tyramide solution (Perkin Elmer Elast Amplification Kit) was added, washed and followed by Streptavidin-HRP (1:500) in PBS with 0.02 % Tween-20 and 1 % BSA. Lastly, the wells were developed with chemiluminescent substrate solution (SuperSignal ELISA Femto, Pierce) for 1 min and read by a luminescence microplate reader (GloRunner DXL Luminometer, Turner BioSystems). The interassay and intraassay CV were <3–14 % within the assay dynamic range. The LOD was 1.54 ng/mL for SBDP150, 0.98 ng/mL for SBDP145 and 0.474 ng/mL for SBDP120.
Microtubule Associated Protein 2 (MAP-2)
MAP-2 sandwich ELISA was performed using 10 uL CSF for quantitative determination. Mouse MAb anti-MAP2A/2B (clone M13, Zymed #13-1,500) was used as capture antibody (5 ug/well) to coat the plate. Biofluid samples (10 uL CSF, or recombinant antigen as GST-fusion protein with residue 1,078–1,551 of MAP-2 at 0.10–6.67 ng/mL) were added with diluent (100 uL total) to microtiter plate wells. After 2 h incubation and washing, HRP-labeled mouse monoclonal anti-MAP-2 (clone AP20; BD Bioscience; #552,320) antibody was added. After washing, plates were developed with substrate solution Ultra-TMB ELISA (Pierce# 34,028), stopped with acidic solution and read at 450 nm with a spectrophotometer (Molecular Device SpectraMax 190). The interassay and intraassay CV were <15 % within the assay dynamic range. Limit of detection (LOD) was determined to be 0.054 ng/mL.
S100B
S100B sandwich ELISA was performed using 5–10 uL CSF for quantitative determination. Mouse monoclonal anti-S100b was used as capture antibody (3ug/well) to coat the plate. After blocking buffer, biofluid samples (5–10 uL CSF) or standard protein (S100beta, human brain protein, Fitzgerald, at 0.0039 ng/ml–0.5 ng/ml) were added. After 30 min incubation and washing, detection polyclonal antibody was used and incubated for 1 h (1 ug/ml and 100 ul/well), followed by HRP-conjugated anti-rabbit-HRP (Jacksonville ImmunoResearch lab) for 30 min. After washing, plates were developed with substrate solution Ultra-TMB ELISA (Pierce# 34,028), stopped with acidic solution, and read at 450 nm with a microplate spectrophotometer (Molecular Device SpectraMax 190). The interassay and intraassay CV were <10 % within the assay dynamic range with a limit of detection (LOD).
Myelin Basic Protein (MBP)
MBP assay was based on commercial MBP ELISA for CSF (iPOC) according to manufacturer’s instructions. Briefly, 50 uL of calibrator (0.13–36 ng/mL) or 4 uL CSF samples with diluent (to 50 uL) was used and incubated with plate with capture antibody (goat polyclonal anti-MBP) for 2 h. After washing, 50 uL detection mouse monoclonal antibody to MBP was added (50 uL) and incubated for 30 min, followed by HRP-enzyme-conjugated secondary donkey anti- mouse IgG antibody. After washing, 50 uL of chromogenic TMB substrate was used for 15 min. 100 uL stop solution was added and absorbance at 450 nm was measured with a spectrophotometer (Molecular Device Spectramax 190). The interassay and intraassay CV were <10 % within the assay dynamic range. The limit of detection was determined to be 0.13 ng/ml.
Rights and permissions
About this article
Cite this article
Papa, L., Robertson, C.S., Wang, K.K.W. et al. Biomarkers Improve Clinical Outcome Predictors of Mortality Following Non-Penetrating Severe Traumatic Brain Injury. Neurocrit Care 22, 52–64 (2015). https://doi.org/10.1007/s12028-014-0028-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0028-2