Abstract
Purpose
To assess the effectiveness and safety of myoinositol for patients with PCOS.
Methods
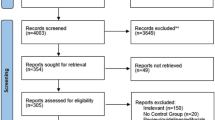
In this meta-analysis, data from randomized controlled trials are obtained to assess the effects of myoinositol vs. placebo or western medicine in women with PCOS. The study’s registration number is CRD42017064563. The primary outcomes included total testosterone, estradiol (E2) and the homeostatic model assessment (HOMA) of insulin resistance.
Result
Ten trials involving 573 patients were included. The meta-analysis results show that: compared with the control group, myoinositol may improve HOMA index (WMD −0.65; 95% CI −1.02, −0.28; P = 0. 0005) and increase the E2 level (WMD 16.16; 95% CI 2.01, 30.31; P = 0. 03); while there is no enough strong evidence that the myoinositol has an effect on the total testosterone level (WMD −16.11; 95% CI −46.08, 13.86; P = 0. 29).
Conclusion
Based on current evidence, myoinositol may be recommended for the treatment of PCOS with insulin resistance, as well as for improving symptoms caused by decreased estrogen in PCOS.




Similar content being viewed by others
References
R. Azziz, K.S. Woods, R. Reyna, T.J. Key, E.S. Knochenhauer, B.O. Yildiz, The prevalence and features of the polycystic ovary syndrome in an unselected population. J. Clin. Endocrinol. Metab. 89, 2745–2749 (2004). https://doi.org/10.1210/jc.2003-032046
Y. Meng, X. Chen, Z. Peng, X. Liu, Y. Sun, S. Dai, Association between high serum homocysteine levels and biochemical characteristics in women with polycystic ovarian syndrome: a systematic review and meta-analysis. PLoS One 11, e0157389 (2016). https://doi.org/10.1371/journal.pone.0157389
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group., consensus on diagnostic criteria and long-term healthiest related to polycystic ovary syndrome. Fertil. Steril. 81, 19–25 (2004). https://doi.org/10.1016/j.fertnstert.2003.10.004. Revised 2003
R. Azziz, E. Carmina, D. Dewailly, E. Diamanti-Kandarakis, H.F. Escobar-Morreale, W. Futterweit, O.E. Janssen, R.S. Legro, R.J. Norman, A.E. Taylor, S.F. Witchel, Task force on the phenotype of the polycystic ovary syndrome of the androgen excess PCOS society 2009: The androgen excess and PCOS society criteria for the polycystic ovary syndrome: the complete task force report. Fertil. Steril. 91, 456–488 (2009)
R. Azziz, E. Carmina, D. Dewailly, E. Diamanti-Kandarakis, H.F. Escobar-Morreale, W. Futterweit, O.E. Janssen, R.S. Legro, R.J. Norman, A.E. Taylor, S.F. Witchel, Androgen excess society 2006.:, Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J. Clin. Endocrinol. Metab. 91, 4237–4245 (2006)
L.J. Moran, M.L. Misso, R.A. Wild, R.J. Norman, Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum. Reprod. Update 16, 347–363 (2010)
J. Vague, La différentiation sexuelle. Facteur determinant des formes de l’obesité. Presse Med. 55, 339–340 (1947)
A.H. Kissebah, N. Vydelingum, R. Murray, D.J. Evans, A.J. Hartz, R.K. Kalkhoff, P.W. Adams, Relation of body fat distribution to metabolic complications of obesity. J. Clin. Endocrinol. Metab. 54, 254–260 (1982)
M.A. Kirschner, E. Samojlik, M. Drejka, E. Szmal, G. Schneider, N. Ertel, Androgen-estrogen metabolism in women with upper body versus lower body obesity. J. Clin. Endocrinol. Metab. 70, 473–479 (1990)
C.R. Kahn, J.S. Flier, R.S. Bar, J.A. Archer, P. Gorden, M.M. Martin, J. Roth, The syndromes of insulin resistance and acanthosis nigricans. Insulin-receptor disorders in man. N. Engl. J. Med. 294, 739–745 (1976)
C. Wu, F. Lin, S. Qiu, Z. Jiang, The characterization of obese polycystic ovary syndrome rat model suitable for exercise intervention. PLoS One 9, e99155 (2014). https://doi.org/10.1371/journal.pone.0099155
J.E. Nestler, J.F. Strauss III, Insulin as an effector of human ovarian and adrenal steroid metabolism. Endocrinol. Metab. Clin. N. Am. 20, 807–823 (1991)
J.C. Marshall, A. Dunaif, Should all women with PCOS be treated for insulin resistance? Fertil. Steril. 97, 18–22 (2012)
J.E. Nestler, D. Stovall, N. Akhter, M.J. Iuorno, D.J. Jakubowicz, Strategies for the use of insulin-sensitizing drugs to treat infertility in women with polycystic ovary syndrome. Fertil. Steril. 77, 209–215 (2002)
V. De Leo, M.C. Musacchio, G. Morgante, P. Piomboni, F. Petraglia, Metformin treatment is effective in obese teenage girls with PCOS. Hum. Reprod. 21, 2252–2256 (2006)
E. Papaleo, V. Unfer, J.P. Baillargeon, F. Fusi, F. Occhi, L. De Santis, Myo-inositol may improve oocyte quality in intracytoplasmic sperm injection cycles: a prospective, controlled, randomized trial. Fertil. Steril. 91, 1750–1754 (2009)
D. Costantino, G. Minozzi, E. Minozzi, C. Guaraldi, Metabolic and hormonal effects of myo-inositol in women with polycystic ovary syndrome: a double-blind trial. Eur. Rev. Med. Pharmacol. Sci. 13, 105–110 (2009)
G. Donà, C. Sabbadin, C. Fiore, M. Bragadin, F.L. Giorgino, E. Ragazzi, G. Clari, L. Bordin, D. Armanini, Inositol administration reduces oxidative stress in erythrocytes of patients with polycystic ovary syndrome. Eur. J. Endocrinol. 166, 703–710 (2012). https://doi.org/10.1530/EJE-11-0840
J.J. Deeks, J.P. Higgins, D.G. Altman, in Special Topics in Statistics, ed. by J.P. Higgins, S. Green Cochrane Handbook for Systematic Reviews of Interventions, Chapter 16 (The Cochrane Collaboration, UK, 2011)
J.J. Deeks, J.P. Higgins, D.G. Altman, in Assessing Risk of Bias in Included Studies, ed. by J.P. Higgins, S. Green Cochrane Handbook or Systematic Reviews of Interventions Version 5.1.0, Chapter 8 (The Cochrane Collaboration, UK, 2011)
J.J. Deeks, J.P. Higgins, D.G. Altman, in Analyzing Data and Undertaking Meta-analyses. ed. by J.P. Higgins, S. Green Cochrane Handbook for Systematic Reviews of Interventions, Chapter 9 (The Cochrane Collaboration, UK, 2011)
E. Benelli, S. Del Ghianda, C. Di Cosmo, M. Tonacchera, A combined therapy with Myo-inositol and D-chiro-inositol improves endocrine parameters and insulin resistance in PCOS young overweight women. Int. J. Endocrinol. 2016, 3204083 (2016). https://doi.org/10.1155/2016/3204083
J. Nehra, J. Kaushal, S.R. Singhal, V.S. Gehlaut, A comparative study of myo inositol versus metformin on biochemical profile in polycystic ovarian syndrome in women. Int. J. Pharm. Sci. Res. 8(4), 1664–1670 (2017). https://doi.org/10.13040/IJPSR.0975-8232
F. Fruzzetti, D. Perini, M. Russo, F. Bucci, A. Gadducci, Comparison of two insulin sensitizers, metformin and myo-inositol, in women with polycystic ovary syndrome (PCOS). Gynecol. Endocrinol. 33, 39–42 (2017)
P.G. Artini, O.M. Di Berardino, F. Papini, A.D. Genazzani, G. Simi, M. Ruggiero, V. Cela, Endocrine and clinical effects of myo-inositol administration in polycystic ovary syndrome. A randomized study. Gynecol. Endocrinol. 29, 375–379 (2013). https://doi.org/10.3109/09513590.2012.743020
A.D. Genazzani, C. Lanzoni, F. Ricchieri, V.M. Jasonni, Myo-inositol administration positively affects hyperinsulinemia and hormonal parameters in overweight patients with polycystic ovary syndrome. Gynecol. Endocrinol. 24, 139–144 (2008). https://doi.org/10.1080/09513590801893232
L. Pkhaladze, L. Barbakadze, N. Kvashilava, Myo-Inositol in the treatment of teenagers affected by PCOS. Int. J. Endocrinol. 2016, 1473612 (2016). https://doi.org/10.1155/2016/1473612
S. Gerli, E. Papaleo, A. Ferrari, G.C. Di Renzo, Randomized, double blind placebo-controlled trial: effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur. Rev. Med. Pharmacol. Sci. 11, 347–354 (2007)
S. Gerli, M. Mignosa, G.C. Di Renzo, Effects of inositol on ovarian function and metabolic factors in women with PCOS: a randomized double blind placebo-controlled trial. Eur. Rev. Med. Pharmacol. Sci. 7, 151–159 (2003)
Y. Loke, D. Price, A. Herxheimer, in Adverse Effects. ed. by J.P. Higgins, S. Green Cochrane Handbook for Systematic Reviews of Interventions. Chapter 14. (Wiley, Chichester, UK, 2008)
J.P.A. Ioannidis, S.J.W. Evans, P.C. Gøtzsche et al. Better reporting of harms in randomized trials: an extension of the Consort statement. Ann. Intern. Med. 141, 781–788 (2004)
A. Mansour, S. Hosseini, B. Larijani, M.R. Mohajeri-Tehrani, Nutrients as novel therapeutic approaches for metabolic disturbances in polycystic ovary syndrome. EXCLI J. 15, 551–564 (2016). https://doi.org/10.17179/excli2016-422. eCollection 2016
T.T. Chiu, M.S. Rogers, C. Briton-Jones, C. Haines, Effects of myo-inositol on the in-vitro maturation and subsequent development of mouse oocytes. Hum. Reprod. 18, 408–416 (2003)
V. Unfer, G. Carlomagno, E. Papaleo, S. Vailati, M. Candiani, J.P. Baillargeon, Hyperinsulinemia alters myoinositol to d-chiroinositol ratio in the follicular fluid of patients with PCOS. Reprod. Sci. 21, 854–858 (2014)
M.J. Iuorno, D.J. Jakubowicz, J.P. Baillargeon et al. Effects of D-chiro-inositol in lean women with the polycystic ovary syndrome. Endocr. Pract. 8, 417–423 (2002)
J.E. Nestler, D.J. Jakubowicz, P. Reamer, R.D. Gunn, G. Allan, Ovulatory and metabolic effects of D-chiro-inositol in the polycystic ovary syndrome. N. Engl. J. Med. 340, 1314–1320 (1999)
J.P. Baillargeon, M.J. Iuorno, T. Apridonidze, J.E. Nestler, Uncoupling between insulin and release of a D-chiro-inositol-containing inositolphosphoglycan mediator of insulin action in obese women With polycystic ovary syndrome. Metab. Syndr. Relat. Disord. 8, 127–136 (2010). https://doi.org/10.1089/met.2009.0052
V. Unfer, J.E. Nestler, Z.A. Kamenov, N. Prapas, F. Facchinetti, Effects of inositol(s) in women with PCOS: A systematic review of randomized controlled trials. Int. J. Endocrinol. 2016, 1849162 (2016)
V. Unfer, G. Carlomagno, G. Dante, F. Facchinetti, Effects of myo-inositol in women with PCOS: a systematic review of randomized controlled trials. Gynecol. Endocrinol. 28, 509–515 (2012). https://doi.org/10.3109/09513590.2011.650660
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
K.Y. and L.Z. contributed equally to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Liuting Zeng and Kailin Yang are joint first author.
Rights and permissions
About this article
Cite this article
Zeng, L., Yang, K. Effectiveness of myoinositol for polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine 59, 30–38 (2018). https://doi.org/10.1007/s12020-017-1442-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1442-y