Abstract
Background
Data on patients with coronavirus disease 2019 (COVID-19) who return to hospital after discharge are scarce. Characterization of these patients may inform post-hospitalization care.
Objective
To describe clinical characteristics of patients with COVID-19 who returned to the emergency department (ED) or required readmission within 14 days of discharge.
Design
Retrospective cohort study of SARS-COV-2-positive patients with index hospitalization between February 27 and April 12, 2020, with ≥ 14-day follow-up. Significance was defined as P < 0.05 after multiplying P by 125 study-wide comparisons.
Participants
Hospitalized patients with confirmed SARS-CoV-2 discharged alive from five New York City hospitals.
Main Measures
Readmission or return to ED following discharge.
Results
Of 2864 discharged patients, 103 (3.6%) returned for emergency care after a median of 4.5 days, with 56 requiring inpatient readmission. The most common reason for return was respiratory distress (50%). Compared with patients who did not return, there were higher proportions of COPD (6.8% vs 2.9%) and hypertension (36% vs 22.1%) among those who returned. Patients who returned also had a shorter median length of stay (LOS) during index hospitalization (4.5 [2.9,9.1] vs 6.7 [3.5, 11.5] days; Padjusted = 0.006), and were less likely to have required intensive care on index hospitalization (5.8% vs 19%; Padjusted = 0.001). A trend towards association between absence of in-hospital treatment-dose anticoagulation on index admission and return to hospital was also observed (20.9% vs 30.9%, Padjusted = 0.06). On readmission, rates of intensive care and death were 5.8% and 3.6%, respectively.
Conclusions
Return to hospital after admission for COVID-19 was infrequent within 14 days of discharge. The most common cause for return was respiratory distress. Patients who returned more likely had COPD and hypertension, shorter LOS on index-hospitalization, and lower rates of in-hospital treatment-dose anticoagulation. Future studies should focus on whether these comorbid conditions, longer LOS, and anticoagulation are associated with reduced readmissions.
Similar content being viewed by others
INTRODUCTION
Four months after the first cluster of cases were reported in Wuhan, China, coronavirus disease 2019 (COVID-19) persists as a major cause of morbidity and mortality worldwide.1 Many healthcare facilities remain stretched beyond capacity. Readmissions following hospitalization for COVID-19 have the potential to exacerbate this burden and may represent a missed opportunity to provide optimal care. As the evolution of COVID-19 remains uncertain, characterization of the clinical course of patients who re-present after discharge is important with potential to inform discharge planning and post-discharge care.2 In this study, we focus on early readmissions more likely related to the index COVID-19 hospitalization. We determine the overall rate of early re-presentation at multiple time points; compare demographics, hospital course, vitals, labs, and other EMR data between patients who re-present vs those who do not; and evaluate how these data changed between discharge and re-presentation.
METHODS
Study Population and Data Collection
We included patients who were at least 18 years old, had laboratory-confirmed SARS-CoV-2 infection, and were admitted and subsequently discharged alive from five MSHS hospitals until April 28, 2020. Data were collected from MSHS electronic health records (EHR). A COVID-19-related hospital admission included any inpatient encounter with detected SARS-CoV-2 from an order within the first 48 h of the encounter, including time spent in the emergency department, or within 48 h of an antecedent lab diagnosis-only visit in an outpatient setting. Patients were excluded if they were still hospitalized, discharged < 14 days prior to the data freeze on April 26th, 2020, or died during the index admission. Detailed chart review revealed return to the hospital within 12 h (N = 28) was primarily due to a lack of care coordination (e.g., primary caretaker not at home). All of these patients were also discharged the day following admission, reflecting important readmissions that highlight critical areas for quality improvement interventions. Because they had an explainable cause for readmission that was not primarily driven by a progressing medical condition, patients returning to the hospital within 12 h were excluded from downstream analyses.
Variables from the EHR were chosen for this analysis based on a combination of their prevalence per patient across the dataset, relevance to COVID-19 based on previous literature and empirical evidence, and the goals of this study. These features included demographics, key vitals, and laboratory measurements on time of discharge from index hospitalization and readmission, disease diagnoses, comorbidities, procedures during hospitalization (including intubation and non-invasive O2 oxygen support), ICU course, and outcomes (death or hospital discharge). Selection, culling, and cleanup of these variables were performed through exhaustive manual inspection by two physicians (AL and GN) and two residents (internal medicine, anesthesiology). Comorbidities were extracted using International Classification of Disease (ICD) 9/10 billing codes for atrial fibrillation (AF), asthma, coronary artery disease (CAD), cancer, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), diabetes (DM), heart failure (HF), and hypertension (HTN). In-hospital anticoagulants included treatment-dose oral anticoagulation (warfarin, dabigatran, rivaroxaban, apixaban, edoxaban), treatment dose low molecular weight heparin (bemiparin, certoparin, dalteparin, enoxaparin, nadroparin, parnaparin, reviparin, tinzaparin), and intravenous heparin. While body mass index (BMI) may be bucketed into categorical representations (e.g., low, normal, high), we kept BMI as a continuous variable because such a reduction in its representation may inject bias into statistical inference and lower the confidence of interpreting its resulting trends. Due to discrepancies in how labs were named in different hospitals, a comprehensive and statistical review of all labs by field name was conducted by the aforementioned team of clinicians to ensure that there was a direct mapping between all sites. Additionally, many labs represented a single component (e.g., sodium), but were acquired from either an arterial blood gas (ABG), venous blood gas (VBG), or basic metabolic panel (BMP). Based on the utility of these lab values in clinical practice and the similarity between their statistical distributions, labs derived from a VBG or BMP were collapsed into a single category (i.e., “SODIUM”), and arterial labs were not incorporated as features in these analyses. The lab closest to discharge, by time of result, in the set of all lab order names that were combined into a single lab category, was chosen as the representative lab value for that category. Finally, lab data below the 0.5th and above the 99.5th percentiles were removed to avoid inclusion of outliers that could represent incorrect documentation or measurement error. Labs with > 80% missing data were subsequently excluded, resulting in an a priori set of 125 variables for comparison of the primary endpoint. Of these 125 variables, all of which are accounted through multiple hypothesis testing, 66 are shown in Tables 1 and 2, and Supplemental Table 1 to highlight pertinent positive and negative findings most salient for physicians, as judiciously determined by our interdisciplinary team of clinicians. The Mount Sinai Institutional Review Board approved this research under a broad research protocol for patient-level data analysis.
Statistical Analysis
In this retrospective cohort study, the primary comparator was patients re-presenting to the hospital within 14 days (cases) vs those who did not (controls). Medians and interquartile ranges were used for continuous data. Univariate statistical significance was identified with the non-parametric Kruskal-Wallis one-way ANOVA or chi-squared tests at Bonferroni-adjusted P < 0.05 (multiplying P by 125 study-wide tests and setting adjusted P values greater than 1 to 1). Due to variable correlations, Bonferroni correction ensured a conservative interpretation of any potential statistical differences. P values were adjusted separately within subgroups (i.e., discharged from the emergency department or readmitted) because they were considered distinct hypothesis spaces. Wilcoxon signed-rank tests compared pairwise differences in labs between discharge and return (Supplemental Table 2). The time to return to hospital by ultimate visit type (ED vs readmission) was compared with cumulative density function plots. Analyses were performed using R (R Foundation) and Python (Python Software Foundation).
RESULTS
Patient and Index Hospitalization Associations with Return to Hospital
Of 2864 patients discharged alive following hospitalization for COVID-19, 103 (3.6%) returned to one of five hospitals within 14 days, with 56 (54.4%) readmitted and the remaining 47 (45.6%) discharged or left from the emergency department (ED) (Table 1). There were no between-group differences in age, sex, or race/ethnicity. Patients who returned to the hospital had lower BMI (26.1 vs 28.0 kg/m2, Padjusted < 0.001) in the absence of a bimodal distribution (i.e., very low or high) of BMI patients (Supplemental Figure 1). Chronic obstructive pulmonary disease (COPD) (6.8% vs 2.9%, Padjusted = 0.035) and hypertension (36% vs 22.1%, Padjusted = 0.003) were more common in those who returned, though other comorbidities such as chronic kidney disease, asthma, coronary artery disease, and diabetes mellitus were not. Though not statistically significant, there was a clinically significant lower frequency of therapeutic anticoagulation use in the index hospitalization among patients who re-presented to the hospital when compared with those who did not re-present to the hospital (20.9 vs 30.9%, Padjusted = 0.06).
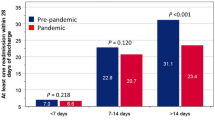
Across the entire subset of individuals that re-presented to the hospital, the median time to return was 4.5 days (Fig. 1). Among patients who returned to the hospital, we observed a shorter median index hospitalization LOS (4.7 days; 95% confidence interval (CI) 2.9–9.1), compared with patients who did not return (6.7 days, CI 3.5–11.5, Padjusted = 0.006) (Table 1). This trend was consistent in subgroups restricted to patients who were intubated (Padjusted = 0.006) or admitted to the ICU (Padjusted = 0.003) during index admission.
Time to return to hospital since discharge for COVID-19-related hospitalization. Cumulative density function of time to return to the ED or readmission illustrates the proportion of patients (N = 103) from each return visit type contributing to the total. For every time point, the proportion of readmitted patients (N = 56) is higher than those who are only seen in the ED and then discharged (N = 47).
Certain index hospitalization laboratory values on discharge differed among patients who returned vs those who did not (Table 2). These included minor but statistically significant differences in basic metabolic panel components, including sodium, potassium, and glucose. Lower white blood cell (WBC) counts, platelets, and LDH, as well as higher albumin, were observed on discharge among patients who returned. However, no major differences were found in other recorded inflammatory markers, including C-reactive protein, erythrocyte sedimentation rate (ESR), fibrinogen, ferritin, procalcitonin, or troponin.
Reasons for and Outcomes on Return
The most common reason for return to hospital was respiratory distress (50%). Other reasons included chest pain (6%), other pain (6%), altered mental status (5%), falls (5%), and skin/soft-tissue infections (5%) (Fig. 2). The frequency of these return reasons was consistent in two subgroups of re-presenting patients: those who were readmitted for a subsequent hospitalization and those who re-presented to the hospital but were discharged from the Emergency Department. In comparison with vitals taken at discharge from the index hospitalization, pulse (96 vs 82 bpm) and respiratory rate (19 vs 18 breaths/min) were higher on return to hospital. Returning patients similarly had higher WBC counts (9.2 × 103 vs 7.0 × 103 cells) and lower lymphocyte percentages (12.1% vs 14.8%) compared at discharge (Supplemental Table 2). On readmission, six (10.7%) patients required ICU-level care. Among all patients that were readmitted upon return, 51 were (91.1%) successfully discharged, three (5.4%) died, and two (3.6%) remained hospitalized.
Reasons for return to hospital in 103 patients. Among patients who returned to hospital within the 14-day event horizon (N = 103), the majority presented with respiratory distress as the primary reason. SSTI, skin/soft-tissue infections; AMS, altered mental status; Resp Distress, respiratory distress.
DISCUSSION
To the best of our knowledge, this is the first report characterizing early return to hospital following discharge in COVID-19 patients across multiple hospital centers. Though the percentage of patients returning to hospital within 14 days was small, we made several important observations. First, patients who returned generally presented within 5 days of discharge, with only half of these requiring hospital readmission. Age, sex, and race/ethnicity were not different in patients returning to the hospital compared with those patients who did not return within 14 days; however, there was a higher prevalence of hypertension and COPD. Second, respiratory distress, accounting for half of all symptoms on return, was the most common cause for returning to the hospital. Finally, returning patients had a shorter LOS, had lower frequencies of ICU care, and were less likely to have been on therapeutic anticoagulation on index hospitalization compared with patients that did not return to the hospital. These findings may offer implications for the post-discharge care of patients hospitalized with COVID-19, and if verified, could inform resource allocation.3,4
Notably, patients returned to hospital relatively early at a median of 4.5 days after discharge from their index hospitalization. While the lack of association between age and return to hospital was surprising, the finding that COPD was more common among returning patients was consistent with the observation that respiratory distress was the most common cause for return. Though lower BMI could serve as a marker for and has been associated with worse health outcomes in other disease states, the distributions of BMI between those returning to the hospital and those who did not were relatively similar (Supplementary Figure 1) with a low difference in means; therefore, further work is needed to unravel the association between BMI and outcomes in COVID-19.
Interestingly we note that patients who returned to the hospital had lower LOS on index hospitalization. Despite administrative prioritization to reduce LOS and readmissions, studies across a variety of disease states have suggested these two outcomes may be inversely related.5,6,7 Reducing LOS during the COVID-19 pandemic has also been emphasized for the purposes of preserving resources and limiting exposure. Further, we observed returning patients were less likely to have required ICU stay during the index hospitalization. ICU stay serves as a marker of illness severity and thereby may caution practitioners to ensure clinical stability prior to discharge.8 Whether continued in-hospital observation translates into longer LOS for improvement in respiratory status impacts readmission status and exposure risk warrants further study.9,10 These patients also had trends of higher heart rate, respiration rate, elevated WBCs, and higher platelet counts when returning to the hospital as compared with discharge, which may be consistent with signs of the continuation of the underlying inflammatory process that may not have subsided fully prior to discharge.
We also observed a trend towards the association between treatment-dose anticoagulation use and return to hospital. There is increasing speculation that COVID-19 is a pro-thrombotic disease11,12 and as such, the impact of treatment-dose anticoagulation on readmission and other outcomes is of special interest. However, this trend may be confounded by the institution of systemic anticoagulation policies at our institution for SARS-COV-2-positive patients mid-way throughout the time period of this study, which suggests the need for a more rigorous clinical trial design to validate this observed trend.
Finally, though comparative data on COVID-19 return to hospital does not yet exist, readmissions for other diseases provide context for our observed re-presentation rate (3.6%). The largest study to date assessing 15-day readmissions following an index hospitalization for pneumonia found that 11.5% of patients were readmitted to the hospital.13 Another study on influenza observed 5.2 readmissions per 100 index hospitalizations within 10 days and 8.6 within 20 days.14 Our readmission rates were lower, which could reflect regional differences before the pandemic, hesitancy to return to the hospital during the pandemic, a preponderance of healthier individuals among those hospitalized for COVID-19, or less likely, re-presentation to hospitals outside the Mount Sinai Health System. Teasing apart these contributions will require further work dissecting geo-demographic, temporal, and historical trends in both our hospital system and others.
Several limitations of this study warrant mention. First, small sample sizes and missing data restricted statistical power and prevented multivariable analysis to adequately control for non-normal distributions and feature collinearities.15 Larger sample sizes may allow the development of such multivariable models to address potentially confounding factors and are actively being pursued.16 The lack of multivariate adjustment was mitigated in our comparison of discharge and re-presentation data, because patients served as their own controls for these hypothesis tests. Another limitation is that height was occasionally recorded from previous hospital encounters in patient charts, so height and BMI were missing in 11% of patients from the database implementation for the index COVID+ hospitalizations. To maintain proper data hygiene, we avoided looking beyond this initial patient encounter to recover these heights. Missing information was also encountered for a subset of anticoagulation medication data, which were obtained with an alternate procurement procedure that resulted in data harmonization issues for 14% of patients. Second, although the MSHS reflects a large and diverse cohort, clinical management varies across hospitals and continues to evolve. Additionally, many of these discharges were in the earlier period of the COVID-19 pandemic when hospital capacity was strained. Thus, generalizability may be limited due to a possible temporal bias, necessitating extension of current studies to longer time periods. Third, readmission over a 30-day horizon may permit comparative analyses with readmission rates for other diseases to inform impact on systems-level operations. The number of readmissions may have been underreported given the retrospective design of this study due to presentation to hospitals outside of the Mount Sinai Health system that could not be tracked via EHR and at-home patient deaths that prevented a return to the hospital.17
In summary, among patients discharged following admission for COVID-19, the rate of early return to hospital was relatively low (3.6%), with only half requiring readmission. The most common cause for return to hospital was respiratory distress. Returning patients were more likely to have a history of COPD and hypertension and have had shorter length of stay and lower frequency of therapeutic anticoagulation use during their index hospitalization. When larger sample sizes become available, the conceptual framework and preliminary trends in this study can help guide future research in understanding determinants of safe discharge and appropriate in-hospital treatment for preventing readmission and death following a COVID-19 hospitalization.
References
Khachfe HH, Chahrour M, Sammouri J, Salhab H, Makki BE, Fares M. An Epidemiological Study on COVID-19: A Rapidly Spreading Disease. Cureus 2020;12(3):e7313.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020. https://doi.org/10.1001/jama.2020.6775
Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA 2010;303(21):2141-2147.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360(14):1418-1428.
Eapen ZJ, Reed SD, Li Y, et al. Do countries or hospitals with longer hospital stays for acute heart failure have lower readmission rates?: Findings from ASCEND-HF. Circ Heart Fail 2013;6(4):727-732.
Damrauer SM, Gaffey AC, DeBord Smith A, Fairman RM, Nguyen LL. Comparison of risk factors for length of stay and readmission following lower extremity bypass surgery. J Vasc Surg. 2015;62(5):1192-200.e1.
Sud M, Yu B, Wijeysundera HC, et al. Associations Between Short or Long Length of Stay and 30-Day Readmission and Mortality in Hospitalized Patients With Heart Failure. JACC Heart Fail 2017;5(8):578-588. https://doi.org/10.1016/j.jchf.2017.03.012
Chalmers JD. ICU admission and severity assessment in community-acquired pneumonia. Crit Care 2009;13(3):156.
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;46(5):846-848. https://doi.org/10.1007/s00134-020-05991-x
Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034.
Paranjpe I, Fuster V, Lala A, et al. Association of Treatment Dose Anticoagulation with In-Hospital Survival Among Hospitalized Patients with COVID-19. J Am Coll Cardiol 2020. https://doi.org/10.1016/j.jacc.2020.05.001
Wichmann D, Sperhake J-P, Lütgehetmann M, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19. Ann Intern Med 2020. https://doi.org/10.7326/M20-2003
Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013;309(4):355-363.
Yandrapalli S, Aronow WS, Frishman WH. Readmissions in adult patients following hospitalization for influenza: a nationwide cohort study. Ann Transl Med 2018;6(16):318.
Song Y, Morency L-P, Davis R. Distribution-sensitive learning for imbalanced datasets. In: 2013 10th IEEE International Conference and Workshops on Automatic Face and Gesture Recognition (FG). IEEE; 2013. https://doi.org/10.1109/fg.2013.6553715
Biau DJ, Kernéis S, Porcher R. Statistics in brief: the importance of sample size in the planning and interpretation of medical research. Clin Orthop Relat Res 2008;466(9):2282-2288.
Weber-Jahnke J, Peyton L, Topaloglou T. eHealth system interoperability. Inf Syst Front 2012;14(1):1-3.
Funding
This work was Supported by UL1 TR001433-05, National Center for Advancing Translational Sciences, National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
The Mount Sinai Institutional Review Board approved this research under a broad research protocol for patient-level data analysis.
Conflict of Interest
GNN is a scientific co-founder of Renalytix AI and Pensieve Health. GNN receives financial compensation as a consultant and advisory board member for RenalytixAI and owns equity in RenalytixAI and Pensieve Health. In the past 3 years GNN has also received consulting fees from AstraZeneca, Reata, GLG Consulting, BioVie and grant support from Goldfinch Bio.
SS is a scientific co-founder of and owns equity in Monogram Orthopedics.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shan Zhao, Benjamin S Glicksberg, Anuradha Lala, and Girish N Nadkarni jointly directed this project.
Electronic supplementary material
ESM 1
(DOCX 50 kb)
Rights and permissions
About this article
Cite this article
Somani, S.S., Richter, F., Fuster, V. et al. Characterization of Patients Who Return to Hospital Following Discharge from Hospitalization for COVID-19. J GEN INTERN MED 35, 2838–2844 (2020). https://doi.org/10.1007/s11606-020-06120-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-06120-6