Abstract
This paper considers how the full range of human experience may catalyze a placebo response. The placebo effect has been characterized as something to control in clinical research, something to cultivate in clinical practice and something present in all healing encounters. We examine domains in which the term ‘placebo’ is used in discourse: clinical research, clinical practice, media representations of treatment efficacy and lay interpretations of placebo—an underresearched topic. We briefly review major theoretical frameworks proposed to explain the placebo effect: classical conditioning, expectancy, the therapeutic relationship and sociocultural ‘meaning.’ As a corrective to what we see as an overemphasis on conscious cognitive approaches to understanding placebo, we reorient the discussion to argue that direct embodied experience may take precedence over meaning-making in the healing encounter. As an example, we examine the neurobiology of rehearsing or visualizing wellness as a mode of directly (performatively) producing an outcome often dismissed as a ‘placebo response.’ Given body/mind/emotional resonance, we suggest that the placebo response is an evolutionarily adaptive trait and part of healing mechanisms operating across many levels—from genetic and cellular to social and cultural.
Similar content being viewed by others
Introduction
Reasons for the use of the placebo can be indicated by summarizing, then, its common purposes: as a psychological instrument in the therapy of certain ailments arising out of mental illness, as a resource of the harassed doctor in dealing with the neurotic patient, to determine the true effect of drugs apart from suggestion in experimental work, as a device for eliminating bias not only on the part of the patient but also, when used as an unknown, of the observer, and, finally, as a tool of importance in the study of the mechanisms of drug action.
—Beecher (1955, p. 1602)
The focus has shifted from the ‘inert’ content of the placebo agent…to the concept of a simulation of an active therapy within a psychosocial context. This capacity of simulation empowers the influence of placebo.
—Price et al. (2008, p. 2.3)
Although there has been a clear maturation in the ways that scholars studying ‘placebo’ have used the term since Beecher’s landmark 1955 article, there remains a great deal of inconsistency among researchers as to how best to define the term and where to focus their analytic attention. Much of this inconsistency stems from the use of the term placebo—Latin for “I shall please”—to refer to ostensibly inert treatments in two contexts that are held in tension by their dissimilar goals. In clinical care, where the goal is to heal patients, clinicians have used placebos for centuries when nothing else is available to treat their patients’ illnesses—the intention being to give patients hope, to do something rather than nothing or, perhaps, to attempt to trigger some innate healing capacity within the patient (Harrington 2002; Kaptchuk 1998; Moerman 2002a). In medical research, where the goal is to determine the efficacy of a specific treatment, placebos have become the control by which ‘active’ treatments are judged efficacious in the ‘gold standard’ of biomedical research: the randomized controlled trial (RCT) (for an analysis of this development, see Kaptchuk 1998).
Of course, even within these narrow contexts, the definition of placebo as ‘inert’ quickly falls apart—because, as any clinician or researcher knows, some patients who receive ‘inert’ treatments do, in fact, get better. This is what has become known as the “placebo effect.”Footnote 1 In recent years, most researchers have aimed to understand the psychosocial and physiological mechanisms that underpin the placebo effect, with increasing recognition that what is studied under this rubric is applicable to all healing encounters (Brody and Waters 1980; Caspi 2003).
While we have significant concerns about the limitations of the terminology, in this paper we use the recently articulated definitions of Price et al. (2008). According to these authors, the placebo effect is “the average placebo response in a group of individuals,” and a placebo response is “the change in a symptom or condition of that individual that occurs as a result of placebo (natural history minus placebo conditions)” (pp. 2.2–2.3).
This paper employs broad anthropological lenses that encompass sociocultural and biocultural perspectives to shed new light on the placebo effect and placebo response. Rather than focusing on the influence of the conscious mind on bodily experience, we argue that direct embodied experience may be a vitally important aspect of healing. As a corrective to what we view as an overemphasis on interpretations of the placebo effect that focus on the conscious mind,Footnote 2 we suggest that what is initially embodied and sensorial may, over time, become cognitive, as narrative, explanation and meaning become attached to the experience. As an example, we examine the neurobiology of rehearsing wellness as a mode of directly (performatively) producing an outcome. Finally, we suggest that the placebo effect is part of a wider array of (self-) healing mechanisms operating across many levels.
Putting ‘Placebo’ in Context
From various vantage points, the ‘placebo effect’ has been differentially characterized as (a) something to control and minimize in clinical research because it confounds the study of treatment efficacy, (b) something of therapeutic value for the practitioner to cultivate in order to maximize patient improvement and (c) something present to differing degrees in all healing encounters despite efforts to cultivate or minimize. While these distinctions are anything but trivial, they are too frequently dismissed or collapsed into a black box containing those healing elements that are not well understood and labeled—at best—as the ‘nonspecific’ or ‘incidental’ elements of therapy (Bootzin and Caspi 2002).Footnote 3 Overall, what is clear is that the interpretation of the placebo effect is highly context specific. We briefly review four domains in which the term has important salience: clinical research, clinical practice, media representations and lay interpretations.
Clinical Trials
The concept of ‘placebo’ is vital to the function of the pharmaceutical industry—specifically in the central role the placebo plays in the clinical trial process. Beecher’s (1955) landmark article, “The Powerful Placebo,” drew attention to the high level of placebo responses in drug trials. Although a number of Beecher’s specific arguments have been invalidated over the years, his call for strictly controlled research to demonstrate pharmaceutical efficacy and mechanism has greatly influenced the way biomedicine conducts research today—that is, by privileging the placebo-controlled RCT as the ‘gold standard’ for demonstrating efficacy.Footnote 4
Beecher also laid the groundwork for biomedicine’s interpretation of placebo effects as confounders to clinical trial research—which can, nevertheless, be subtracted from an active drug arm to indicate the verum effect (or ‘true’ effect of the study drug). In this process the placebo effect became an underexamined catch-all for what could not be controlled or quantified in RCTs. In his review of the development of the RCT, Kaptchuk (1998) argues that elite medical researchers were deeply invested in the success of this new paradigm in which “medical intervention was only scientifically acceptable if it was superior to placebo. No longer was it sufficient for a therapy to work: it had to be better than placebo. For the first time in history…method became more important than outcome” (p. 1724, italics added).
From a practical perspective, there are elements specific to clinical trials that may affect the placebo response in unique ways (e.g., the consent process, increased therapeutic attention and surveillance, increased self-surveillance). For example, in a study of an experimental Parkinson’s treatment, patients’ perception of treatment group assignment was the strongest predictor of outcome (McRae et al. 2004). Indeed, analyses of ‘failed’ antidepressant trials indicate that participation in a clinical trial, alone, can have therapeutic effects (Kirsch et al. 2008; Lakoff 2007; Montgomery 1999). It must be stressed that a number of research or methodological ‘artifacts’ (such as the natural history of a disorder, regression to the mean, measurement problems, therapist or observer bias and confounding therapeutic procedures) are not ‘placebo effects’—although they may appear so in research settings (Bootzin and Caspi 2002; Kleinman et al. 2002).
Placebo researchers have identified a number of important critiques of the way the concept of ‘placebo’ has been applied to clinical research. Caspi and Bootzin (2002) argue that the dominant additive (or ‘fastidious’) model of the clinical trial—that is, the model suggesting that the total effect of treatment is the sum of the placebo effect and the verum effect—is flawed because it mistakenly equates the outcome of the placebo arm of a clinical trial with the placebo effect. Even without accounting for the synergy that may take place between the defining and the incidental elements of treatment, the additive model does not account for methodological artifacts in both active and placebo arms of the trial. In actuality, “only by comparing the total effect of the placebo intervention with a no-treatment arm, in a three-arm trial, can we estimate the true magnitude of the placebo effect” (p. 447). Even careful fastidious models (such as Kirsch and Sapirstein 1998; Walach et al. 2002) do not “include the possibility of interactions between different therapeutic ingredients” (Caspi and Bootzin 2002, p. 449)—although the literature supports these synergistic effects.Footnote 5
Along similar lines, Kaptchuk (2002) argues that the focus of the RCT is on the specific efficacy of an intervention, which is measured against a placebo arm consisting of any number of ‘nonspecific’ effects. Within this research paradigm, demonstrating the specific efficacy of an intervention is deemed superior to determining the overall effectiveness of treatment—thus therapeutic effects attributed to the placebo are generally discarded and ignored. Kaptchuk rightly argues that dismissing placebo effects “diminishes our knowledge of important dimensions of health care” (p. 817).
What about Beecher’s ‘powerful placebo’? While there can be no doubt as to the influence Beecher’s assertion has had on medical research, whether or not the placebo really is ‘powerful’ (and what this means for evaluating clinical research and practice) has been a source of continued debate in the field of medical research. In a meta-analysis comparing placebo arms to no-treatment arms in 156 RCTs (of various sizes) of 46 disparate health conditions (from depression to bacterial infections to Alzheimer’s disease), Hrobjartsson and Gotzsche found “no evidence that placebo interventions in general have large clinical effects and no reliable evidence that they have clinically useful effects” (2004, p. 98; 2001). The authors claim that this ‘evidence’ demonstrates that placebo-controlled clinical trials are an unproblematic way to determine the efficacy of pharmaceuticals and interventions.
The “power” attributed to ‘placebo’ appears to depend on the research perspective. Whereas a strong placebo performance in comparison with a complementary or alternative (CAM) therapy, such as homeopathy, acupuncture or herbal therapies, is frequently designated as ‘proof’ that the CAM therapy has no benefit (Bausell 2007; Newton et al. 2006; Shang et al. 2005; Walach et al. 2005), a strong placebo performance in comparison with a ‘known’ active drug is deemed a ‘powerful placebo’ (Kirsch and Sapirstein 1998).
For example, in an analysis of antidepressant clinical trials, Lakoff (2007) provides an excellent example of the pharmaceutical industry’s battling a ‘powerful placebo’ in its efforts to bring new antidepressant medications to market. Based on early phase studies, drug makers are convinced of the efficacy of these novel antidepressant drugs and see their task as finding “the right patients for the drug” in the process of producing positive clinical trial outcomes (Lakoff 2007, p. 57). In practice, finding the ‘right patients’ means identifying potential ‘placebo responders’ through placebo run-in periods and excluding them from the study prior to randomization.Footnote 6 On a positive note, these efforts indicate increased openness to the idea that treatments be targeted to more specific patients, rather than the population at large. Because of intense competition in the pharmaceutical marketplace, individualization (rather than a ‘one-pill-fits-all’ mindset) is becoming a trend in the pharmaceutical industry, and it will, presumably, have positive consequences for patients. In clinical practice, of course, identifying which patients are likely to do well on a particular treatment is a central tenet of good clinical practice.Footnote 7
Clinical Practice
Unlike clinical trials, where the placebo effect is thought to obscure investigation of therapeutic efficacy, in clinical practice the placebo effect is something to be cultivated through the therapeutic process in order to maximize patient healing. Brody (2000) and Caspi (2003) have been stalwart advocates of the perspective that the existence of a ‘placebo effect’ is not dependent on whether a treatment is active or inert by biomedical standards; rather, it is present or absent to varying degrees in all therapeutic encounters. Placebo effects can enhance or aggravate biologically active treatments, just as they can ‘produce’ positive or negative (nocebo) ‘effects’ in treatments understood to be biologically inert (or those with mechanisms not understood within our current biomedical paradigm). As Caspi and Bootzin (2002) note, placebo effects have been widely mislabeled as ‘nonspecific effects,’ when they are, in fact, highly specific effects that stem from what are currently nonspecific elements of treatments (i.e., relieving pain via specific pathways, alleviating depression, healing an ulcer, etc.).
Brody and Waters (1980) pioneered the notion that clinicians should actively cultivate the placebo effect in their practice, arguing that “there is placebo-effect component to virtually every physician-patient encounter.… [O]ne should use the placebo component in ways that change the meaning of the illness experience for the patient, with positive therapeutic outcomes” (p. 447, original italics). Specifically, they argue that the diagnostic process, itself, is a powerful therapeutic tool that can shape the meaning of a condition for patients by providing them with an explanatory framework that “allows the patient to make sense of his suffering” (Brody and Waters 1980, p. 448; Brody 1997, 2000; see also Illich 1975).
Integrating research from a number of sources, Caspi (2003) argues that the placebo effect is a contextual phenomenon that triggers the patient’s innate homeostatic healing response. He identifies the therapeutic relationship between clinician and patient as a key element in triggering the placebo effect. In Caspi's (2003) model of the ideal therapeutic relationship, the clinician and patient form a collaborative partnership in which “the patient regards the clinician as experienced, competent and optimistic, and…the clinician genuinely expects the treatments to help” (p. 705). Caspi also argues that the clinician can use the therapeutic encounter to positively reframe the meaning of the patient’s health status in ways that can instill hope and charge the encounter with positive expectancy, as well as provide the patient with opportunities to attribute meaning and attain mastery over skills that lead to empowerment and improved outcomes.Footnote 8 Bootzin and Caspi (2002) warn, however, that clinicians need to take care not to overextend patient hope and expectancy, lest it fail to live up to patients expectations.
While placebo researchers are interested in the mechanisms underlying the manifestation of placebo effects in clinical practice, the central question facing clinicians is (or should be) how to trigger the placebo effect in all patients in order to maximize their therapeutic outcome.
Representations in the Media
Given the central role that ‘placebo’ plays in medical research, it is not surprising to find the term widely used in health-related media reports—especially those touting (or discrediting) new and promising therapies. Within the media, the term ‘placebo’ is used in two primary contexts. First, media reports index the placebo-controlled RCT—the ‘gold standard’ of biomedical research—by citing how a study therapy (usually a pharmaceutical) is performed in contrast to a placebo, lending credibility to both the research and the report. Alternatively, the word ‘placebo’ is used as a synonym for deception in medicine. It is expressly defined as a “fake,” a “sham” or a “sugar pill”—especially in reports “debunking” or expressing skepticism in alternative (CAM) therapies (Adler 2007; BBC 2002), or in reports of unexpectedly strong placebo performances in clinical trials (Vedantam 2002). In such cases, the use of the term ‘placebo’ communicates faith in the underlying biomedical paradigm, that ‘true’ healing of real diseases only occurs in the context of a powerful external (chemical or mechanical) intervention, and indicates surprise when this paradigm is challenged. The dual headlines for an Associated Press report on a three-armed clinical trial of acupuncture, sham acupuncture and conventional care illustrate the media’s take on ‘the placebo effect.’ These headlines (produced for the same story) read: “Researchers: Even Fake Acupuncture Works” and “Acupuncture, Real or Sham, Works Better Than Standard Care for Low Back Pain” (Johnson 2007a, b).
Nevertheless, health-care consumers depend on media reports to determine what products are safe and effective. This is especially true for products readily available without a health-care gatekeeper, such as over-the-counter medications, dietary supplements and CAM therapies (Fonnebo et al. 2007; Nichter and Thompson 2006). While reports of something being ‘good for you’ result in increased sales, reports of results showing that something performs ‘no better than placebo’ can result in major drops in sales. For example, share prices for pharmaceutical companies Schering-Plough, the makers of Vytorin (a combination pill for high cholesterol), and Merck, the maker of Zetia (a component drug of Vytorin), dropped by 40% and 25%, respectively, in the 10 weeks following media reports that Zetia may be ‘no better than placebo’ in a recent clinical trial.Footnote 9
From time to time, the media takes on the ‘placebo effect’ directly. In May 2007, the hosts of Radio Lab, from New York Public Radio, examined the placebo effect from a number of different angles.Footnote 10 While they undoubtedly simplified this complex topic for a popular—albeit educated and interested—audience, they were extraordinarily successful in presenting the vast array of factors that underlie any robust understanding of the placebo effect. For example, they spoke with neurobiologist Fabrizio Benedetti about the brain’s “internal pharmacy”—that is, how our endogenous chemical faculties explain our brains’ capacity to recognize and respond to pharmaceutical intervention.Footnote 11 The hosts of Radio Lab also explored topics of interest to social scientists, such as the social context of illness (framed in this context as “the story you tell” about pain) and the context of treatment (that is, the therapeutic power of diagnosis, the symbolic power of the doctor’s white coat and the contextual power of expectation and ‘belief’ on the part of patient and practitioner).
What is striking is the degree to which the hosts of this program recognize the seamlessness between the ‘placebo effect’ and ‘healing.’ Although they initially referred to the placebo effect as “the true healing power of lies” (a statement reflective of the overall characterization of the placebo by the media), they revise this statement as the show progresses, saying, “This show really is not about lying. It’s about healing—the healing process, which doesn’t happen in a vacuum.” The same cannot be said for most media coverage, which treats ‘the placebo effect’ with a mixture of surprise and awe (“Just thinking a medicine will make you feel better actually may—even if it’s fake” [CNN 2004]) or as the outcome of trickery and/or deception (“Even those who should know better can be fooled by personal experience” [Adler 2007]).
Lay Interpretations
Despite a great deal of media attention, the public is often unclear as to how to interpret the notion of placebo. The literature is virtually devoid of studies aimed at understanding lay interpretations of this concept. Nevertheless, lay perceptions about what a placebo can or cannot do, and/or what ‘the placebo effect’ is, may make a difference in therapeutic, as well as clinical trial, outcomes. Ader (2000) posits that patients’ hypotheses about whether they are receiving active or placebo treatment may interact with their actual placement in clinical trials such that there are actually four groups to be analyzed: (a) those who rightly believe they are receiving the active treatment (approximating “real” treatment conditions), (b) those who believe they are receiving active treatment but are receiving placebo (yielding “classic placebo effects”), (c) those who believe they are receiving placebo but are receiving active treatment (which may attenuate the performance of the active drug via negative expectancy or “nocebo response”) and (d) those who rightly believe they are receiving placebo (yielding “little to no response”).
Although we have not conducted a systematic study of lay interpretations of this concept, we have taken special note when the topic of placebo has come up in our interviews on other issues (such as dietary supplement use and menopause-related health-care decision-making). When our interviewees spontaneously mentioned the term ‘placebo’ they most often used it in reference to a treatment of questionable efficacy (in most cases, we were talking with them about dietary supplements). They used the term to indicate that a product was either (a) harmless or (b) useless. In the first instance, a number of interviewees used the term ‘placebo’ as a toss-off term when they were expressing doubt or skepticism about whether a product was efficacious, while also considering it harmless to try, especially in comparison with an active pharmaceutical known to have serious risks or side effects. For example, this “can’t hurt and might help” attitude was expressed by Natalie when she was asked (by J.J.T.) how she anticipates managing the symptoms of menopause. She responded, “I probably would start taking soy Estroven, you know, over-the-counter, harmless, placebo kind of thing.”
When interviewees used the term ‘placebo’ to reference something they deemed useless, it was often used benignly (e.g., “It is just a placebo”)—either to express skepticism and disregard a product or to characterize, in hindsight, a therapy or product they had hoped would work but proved ineffective for them over time. An interviewee told M.N. that a placebo was a treatment “you hope will work and think it does, but the effect just doesn’t last long.” In other cases, the term was used to reference what they perceived as deliberate deception on the part of health-care professionals or the pharmaceutical industry. For example, Carla told J.J.T. about seeking out treatment for excruciating menstrual pain:
I went to a doctor for medicine, and he didn’t believe me so he gave me placebo. And I kept saying, “These aren’t working, you know, these aren’t working…” When I went back to [an acquaintance], because she used to work in a medical field, she looked at it and said, “This isn’t medicine.” She said, “This is half aspirin and half placebo.”
In general, we have observed that people are not so much mistaken about the definition of ‘placebo’ as they are confused about to how to translate the concept into their own health-care decisions—which is evident from the way that they talk about it. For example, when M.N. asked Linda what it would mean if she found out that a supplement performed “no better than a placebo,” she responded, “Well, it would mean you aren’t using enough. Because supplement-makers are afraid of a law suit for side effects, they tell you to use a low dose. You have to experiment with it yourself to make it work” (Nichter and Thompson 2006; Thompson and Nichter 2007).
Other interviewees have interpreted the phrase “no better than placebo” to mean that a medicine thought to be active was, in fact, biologically inert. A number of interviewees rationalized that positive therapeutic experiences with something deemed “no better than placebo” indicated that either (a) they did not have a ‘real’ illness to begin with or (b) the illness had already “run its course” by the time they treated it. Another interviewee described the placebo effect (to M.N.) as “no better than chance,” explaining that “your chances of it working are 50/50. No better than that. Half of the time you are probably going to improve anyway, so the medicine does not increase your chances much more than taking a placebo, which is a fake medicine.” And yet another interviewee interpreted the placebo effect as psychological, explaining that when a patient with a physical illness improves with placebo, “then it is belief in the medicine that cured the person. That can happen sometimes; it’s like faith healing.” [M.N.: When someone gets healed by a preacher, is that a placebo effect?] “I guess that is what a scientist would probably call it.”
Overall, examples like these suggest that, although people have a general understanding that placebos operate in clinical trials to help establish the efficacy of products, there appears to be a great deal of confusion about how to apply these results in their own decision-making and how to reconcile them with their personal experiences with these products.
Theorizing Placebo: A Critical Review
A great number of explanations for the placebo effect have been suggested over the years. In this section, we examine four perspectives that have received the most scholarly attention: classical conditioning, expectancy, the therapeutic relationship and meaning. Although the language used in this literature may often appear all-inclusive, researchers and philosophers of these perspectives undoubtedly view them as complementary—rather than exclusive—approaches to understanding this complex phenomenon.
Classical (Pavlovian) Conditioning
Probably the best-known, and earliest, biological explanation of the placebo effect is classical conditioning. While conditioning cannot explain all placebo effects, there are well-documented examples of classically conditioned placebo effects on the immune and endocrine systems in human and animal models. Proponents of a classical conditioning argument focus on the physiological response of the body “to a substance or treatment that is not explicable on the basis of the known properties of the substance or treatment” (Siegel 2002, p. 134). According to the Pavlovian conditioning paradigm, the body responds therapeutically to a neutral conditioned stimulus (CS), the ‘placebo,’ which had been previously paired with an unconditioned stimulus (UCS). The response to the CS alone—when it mimics the response to the UCS—is called the conditioned response (CR) (Ader 1997). For example, in one study, multiple sclerosis patients ingested a ‘neutral’ anise-flavored syrup (CS) while receiving ‘active’ injections of cyclophosphamide (UCS). When patients ingested the syrup and received less than 1 percent of the active injection, 8 of 10 had an active therapeutic response (CR) (Giang et al. 1996; Goebel et al. 2002).Footnote 12 This approach to understanding the placebo response is complicated by paradoxical (‘compensatory’) responses to conditioned stimuli, in which the body responds in the opposite direction—presumably to compensate for the expected UCS. Furthermore, Siegel (2002) acknowledges that “all placebo effects cannot readily be attributable to Pavlovian conditioning” because “pharmacologic CRs often do not mimic the drug effect” and, most notably, because “people can…have placebo responses without previous drug experience” (p. 153, original emphasis).
Ader takes a more critical perspective. He argues that placebo effect in the presence of a CS “looks like” a CR (Ader 1997, p. 140, 2000); however, researchers have yet to undertake a “systematic analysis of the placebo effect within the context of conditioning” (1997, p. 142). Specifically, Ader focuses on the importance of learning in catalyzing the placebo effect, and calls for a series of conditioning trials in order to better understand—and assess the potential clinical implications of—the phenomenon. For example, Ader suggests the need for systematic investigation of partial reinforcement schedules of pharmaceuticals (rather that the all/nothing scenario of RCTs) to investigate whether the placebo response might be harnessed such that patients will be able to gain the benefits of pharmacotherapy while reducing net exposure to the pharmaceutical.
Kirsch (1997) notes that “this model of classical conditioning eliminates the need for cognitive or mentalistic concepts in explanations of learning” (p. 169). While classical conditioning does provide an important alternative to cognitive models of the placebo effect, it is a narrow example of a broader concept—direct embodied experience—that deserves further investigation. We take this topic up in detail in the next section.
Expectancy
With the exception of classical conditioning, most conventional models of the placebo effect require that the patient consciously perceive certain elements of the simulated therapeutic experience—such that the brain responds as if the patient received active treatment, thus biochemically or physiologically reproducing the effects of active treatment in/on the body.
Perhaps the most thoroughly researched model of the placebo effect has become expectancy. Simply put, expectancy is the patient’s level of expectation that he or she will be helped by the treatment. Expectancy is a fairly robust and comprehensive model, in that it recognizes the importance of the therapeutic context in supporting expectancy and triggering a placebo effect. One of the most important factors in triggering an expectancy-induced placebo response appears to be verbal instruction or suggestion. For example, in a study of expectancy and placebo analgesia (Pollo et al. 2001), patients recovering from surgery for lung cancer received buprenorphine on demand for pain management, along with a saline IV infusion. Patients were instructed in one of three ways with regard to the saline infusion: group 1 was told nothing (natural history), group 2 was told that they would receive either a powerful analgesic or placebo (simulated double-blind condition) and group 3 was told that they were receiving a powerful analgesic (deceptive condition). After three days, the authors found that patients in the double-blind condition requested less buprenorphine than those in the natural history group, and patients in the deceptive condition requested the least buprenorphine overall. Pollo et al. conclude that “different verbal instructions produced different outcomes which, in turn, led to a significant change of behavior and a significant reduction of opioid intake” (p. 82). These findings—about the power of verbal suggestion on expectancy—were replicated in a study of patients with irritable bowel syndrome, which found that “adding a verbal suggestion for pain relief can increase the magnitude of placebo analgesia to that of an active agent” (Vase et al. 2003, p. 17). Documenting the importance of media and the commercial marketplace in patient expectancy, a recent study found that subjects experienced greater pain reduction from a placebo analgesic when they were instructed that the drug cost $2.50 per pill than when they were told it “had been discounted” to $0.10 per pill (Waber et al. 2008, p. 1016).
A related concept is ‘self-efficacy’—that is, the belief “that one can successfully perform that actions required to achieve valued outcomes”—which activates a positive feedback loop to help patients feel that their illness experience is manageable (Bootzin and Caspi 2002, p. 119). Bandura argues that placebos may play an important role in boosting patients’ perceived self-efficacy in their abilities to withstand pain or to initiate and maintain positive personal change. For example, he reports on a study in which researchers measured subjects’ ability to endure pain under varying conditions of expectancy. Bandura and colleagues found that “efficacy beliefs predicted how well people managed pain. The stronger their beliefs in their ability to withstand pain, the longer they endured mounting pain” (reported in Bandura 1997, p. 271).
While most of the attention to expectancy and self-efficacy has focused on the patient, Bootzin and Caspi (2002) explicitly connect these concepts to the therapeutic relationship, arguing that the clinician plays an important role in “charg[ing] the intervention” with positive expectation by providing information, teaching skills and having confidence in the treatment (p. 120). Despite the powerful effects that can be produced through increased self-efficacy, they are “vulnerable to revision” if expectancies are not confirmed (p. 120).
Recent work suggests that desire—defined by Price et al. (2008) as “the experiential dimension of wanting something to happen or wanting to avoid something happening” (2.8)—interacts with expectancy in a synergistic way, such that the placebo effect is best potentiated when there is both desire for and expectation of an effect. The final piece of the expectancy-desire puzzle is the positive feedback loop of somatic focus (Geers et al. 2006; Lundh 1987)—“in which positive placebo suggestions for improvements in physical health lead individuals to attend selectively to signs of improvement. When they closely notice these signs, they are said to take them as evidence that the placebo treatment has been effective” (Price et al. 2008, p. 2.11).
Therapeutic Relationship
A number of clinically oriented placebo scholars have argued that the patient-practitioner relationship is the most important variable in producing a placebo response in patients (Benson and Friedman 1996; Brody 1997; Brody and Waters 1980). These authors are less concerned with understanding the mechanisms for producing placebo effects than they are interested in enhancing patients’ responses to treatment. For example, Caspi (2003) focuses on therapeutic relationship as a key element in “triggering” the “innate ability of the body to heal itself spontaneously” (p. 703). He identifies several important practitioner qualities, but argues that it is the interpersonal relationship—rather than the individual characteristics of the patientFootnote 13 or practitioner—that enables a placebo response (p. 705). On a similar note, Benson and Friedman (1996) argue that “positive beliefs and expectancies” of patients and practitioners, as well as a “good relationship” between the two, are the essential elements for producing a placebo effect. They stress that an enhanced therapeutic relationship can “maximize” the placebo effect, and “optimize” all clinical care (p. 198).
While we recognize the positive effect that a ‘good relationship’ between patient and practitioner could have on therapeutic outcomes, we must stress that the power in the therapeutic relationship may be more complex. For example, Nichter and Nordstrom (1989) argue that finding the right ‘fit’ between patient and provider among the rural Sinhalese in Sri Lanka has more to do with concordance on the levels of ‘constitution,’ ‘habit’ and ‘power of the hand’ (that is, a practitioner’s capacity to heal a particular patient) than any interpersonal dynamic between individuals. A similar notion comes into play in biomedicine when a patient’s confidence that a particular practitioner is well suited for managing a particular health concern (e.g., the calculating oncologist or surgeon who provides a clear-cut course of action, or whose reputation and/or pedigree is compelling) trumps a patient’s general desire for a ‘good relationship’ with his or her health-care provider.
For his part, Brody (1997) focuses on a “meaning model” of placebo action (cf. Moerman’s “meaning response,” below)—arguing that the practitioner plays a crucial role in ‘altering’ the meaning of the patient’s illness experience in a positive direction. This process consists of three elements on the part of the practitioner: “providing an understandable and satisfying explanation of the illness; demonstrating care and concern; and holding out an enhanced promise of mastery or control over the symptoms” (p. 79). Brody and Waters (1980) illustrate the power of the therapeutic relationship through a case study of a patient with sharp chest pains, although no signs of disease. With the guidance of his practitioner, the patient narrates an illness experience that connects the chest pains to emotional turmoil and mourning. “Armed with the awareness, he is able to pair his feelings with his symptoms. He is encouraged to mourn actively, after which he finds that the chest pains do not recur” (p. 446).
Brody’s approach to understanding the placebo effect focuses on the meaning that an individual assigns to his or her illness and therapeutic encounter—often through narrative. According to this ‘meaning-centered’ framework, a healer must be attentive to the culturally situated meaning a patient assigns to illness and work to transform the meaning of illness for the patient by providing a meaningful explanation, diagnosis and therapy that ‘makes sense’ of the patient’s suffering within a sociocultural context (Brody 1997, Brody and Waters 1980; Brody et al. 2004). This transformation by which personal suffering is given socially acceptable meaning is what Obeyesekere has termed the ‘work of culture’ (Nichter 2008; Obeyesekere 1990; Throop 2003). Anthropologists have documented many examples in which determining the ‘right’ explanation for the patient’s suffering is an extensive process involving consultations with a number of providers (Harrell 1991; Nichter 1981b; Nuckolls 1992), illustrating that what constitutes an effective therapeutic relationship may be more a practitioner’s ability to provide an acceptable explanation for the patient’s suffering than a ‘good’ interpersonal relationship.Footnote 14
Bootzin and Caspi (2002) offer a well-developed and compelling ‘cognitive model for the placebo effect within the therapeutic process’ (pp. 126–128). The merits of Bootzin and Caspi’s model are the strong underlying assumptions: first, that the placebo effect is dynamic and, second, that the placebo effect interacts synergistically with other therapeutic elements. In their model, the clinician-patient relationship (a) generates the clinician’s treatment plan and (b) affects the patient’s interpretation and understanding of his or her health status. Thus, the clinician-patient relationship provides an opportunity for the clinician to “positively reframe the meaning of any medical condition” (p. 127). This ‘cognitive reframing’ can lead to (a) a placebo/nocebo effect from positive/negative expectations as well as (b) the development of coping strategies shaping the patient’s ongoing health-related behaviors (e.g., adherence/compliance to treatment and/or patient-initiated practices). Bootzin and Caspi refer to this as the ‘total package of care.’Footnote 15
Sociocultural “Meaning”
Moerman (2002a), an anthropologist, has received a great deal of attention for his reframing of the placebo response as the ‘meaning response,’ which he defines as “the physiological or psychological effects of meaning in the treatment of illness” (p. 14). In his treatment of the ‘meaning response,’ Moerman extracts a wide range of culturally shaped, ‘meaning-related’ variables from the clinical trial literature, including the meaning of surgery, adherence to treatment, physician characteristics and the formal factors of treatment such as color, number and type of pills. He reports, for example, on a study where subjects were randomized to receive one of four treatments for headaches: unbranded placebo, branded placebo, unbranded aspirin or branded aspirin. After one hour, all the subjects reported improvement. And while aspirin outperformed placebo, both branded aspirin and branded placebo outperformed their unbranded counterparts. Moerman argues that these data indicate that although “the [placebo] pills were inert, the ‘taking a pill’ wasn’t inert, and the brand name wasn’t inert” (p. 19).Footnote 16 The more recent study of the $2.50 placebo analgesia outperforming its $0.10 counterpart (Waber et al. 2008), described above, suggests that notions of the ‘value’ of treatment—whether it is located in the brand name, cost or, perhaps, availability—are implicated here.
While Moerman has been criticized for his decontextualized extraction of clinical trial data (Kirmayer 2003), he echoes Brody (1997, 2000) in stressing that meaningfulness “can make a huge difference for patients in the objective and subjective dimensions of their illness, regardless of the effectiveness of the specifics of the treatment” (Moerman 2002b, p. 103). Clearly, “meaning” is implicated in producing a placebo response, but it cannot be said to be the whole story. To quote Kirmayer (2003), “There are many ways to unpack the meaning of meanings” (p. 288), and unfortunately, Moerman uses the term ‘meaning’ uncritically as a ‘catch-all’ for everything that cannot be accounted for by the verum effect or natural history of the disease. Throughout his work on placebo, all incidental and preliminary elements of therapy are attributed to “meaning.” Only at the very end of his book does he mention that “meaning” encompasses a number of complex and varied representations and relationships—identifying the metonymic relationship (part for whole), the iconic relationship (based on resemblance) and the symbolic relationship (an arbitrary relationship between two things) (Moerman 2002a, pp. 148–149). Furthermore, Moerman ends with a truism: “Meaning affects life; life affects meaning” (p. 150).
Like the psychology-oriented scholars of the placebo effect, Moerman privileges the way patients consciously interpret the healing encounter or therapy over other ways of knowing. Although he is dealing with powerful symbolic, affective, aesthetic and performative dimensions of healing, Moerman focuses his analytic attention on what happens in the conscious mind of the individual in terms of knowledge, belief and understanding. For example, Moerman (2002a) employs Levi-Strauss’ oft-cited secondary analysis of Cuna shamanistic curing during difficult childbirth (p. 94). Following Levi-Strauss’ interpretation, Moerman argues that psychotherapy—like Cuna healing—”evokes meaning responses” by providing a coherent theoretical lens through which the patient can view his or her suffering. This interpretation, however, has been thoroughly criticized in anthropology. Both Briggs (1994) and Atkinson (1987) have critiqued Levi-Strauss’ analysis on the very grounds that it places undue emphasis on the meaning of the narrative incantation, thus neglecting the social and performative force of the ritual. Citing their field experiences, they independently argue that the curing process operates beyond the patient’s cognitive interpretation of the text—which may not even be accessible to the patient. Rather, when the social construction of the body is of central concern, healing may not be limited to the physical body of the patient. Along similar lines, Laderman (1987), looking to Malay birth incantations to critique Levi-Strauss’ textual interpretation, argues that “incantations cure by analogy, not through their specificity but by their ‘fan’ of meanings, their multi-layered nature and the ambiguity of their symbols” (p. 301). By uncritically following Levi-Strauss’ analysis, Moerman collapses the complexity of symbolic and performative healing and defaults to an overly simplistic explanation of the practitioner providing an ‘understanding’ for the patient in order to invoke his model of the ‘meaning response.’ In short, Moerman neglects many tools anthropology has to offer and falls back on what is already known about the placebo effect.
From Sociocultural to Biocultural Perspectives
Without a doubt, conscious awareness of the healing encounter plays an important role in triggering a placebo response and enhancing therapeutic effectiveness. However, as anthropologists, we must stress that the explanatory mechanisms that have been discussed from a dominantly psychological and cognitive perspective are neither solely, nor predominantly, conscious. We find that overemphasis of conscious awareness in these explanatory mechanisms has left the field experientially starved—that is, this perspective has overlooked direct sensory and embodied experience (or implicit perception). Here we reorient the discussion to consider how the full range of human experience may catalyze what is commonly characterized as a ‘placebo response.’ We refocus analytical attention on what Ots (1991) calls “the intelligent lived-body” through two alternative frameworks: embodied experience and performative efficacy. As in the previous section, the frameworks we present below are intended as complements to—not replacements for—other approaches to unpacking the black box of the placebo effect.
Embodied Experience
Scheper-Hughes and Lock (1987) argue that there was a “failure to conceptualize a ‘mindful’ causation of somatic states” in clinical biomedicine until the 20th century when psychiatry and psychosomatic medicine emerged (p. 9). In recent years, the recognition that the mind can positively affect the body has been central to many cognitively oriented studies of the placebo effect (Bandura 1997; Bootzin and Caspi 2002; Brody and Waters 1980; Caspi 2002; Moerman 2002a). However, the comprehensive study of the placebo effect must fundamentally reconceptualize the body—not as the passive site of medical intervention, but as the penultimate multisensory organ and the locus of lived experience (Merleau-Ponty 1964).
The body experiences the intersection of one’s material corpus, one’s sense of self, and the rest of the world through the senses. Sensorial experiences—in the form of sight, smell, taste, touch, hearing and bodily sensations such as dizziness and aesthetic experiences like rhythm—have the extraordinary power to evoke and trigger embodied memories of past experiences, including positive and negative healing experiences (Nichter 2008). In addition, sensations—as our mode of perceiving the world—are closely tied to emotions such as pleasure, safety and fear. Examples abound for each of us: the smell of baking apple pie makes us feel warm and secure,Footnote 17 while the sound of the dentist’s drill makes us feel fear and dread. The feelings associated with the sound of that dentist’s drill may be clearly linked to the memory of specific appointment when the Novocain wore off too early. Alternatively, the sound may just make you cringe and tense your body, without connection to any specific memory. In this case, the sensation (the sound of the drill) and the emotion (fear and dread) leapfrog conscious cognition (memory or meaning) and language (narrative) to trigger a direct reaction at the site of the body.
Direct experiences (sensation, sensory experience, emotion) may be filtered through consciousness and be stored as memory and/or narrative, or they may bypass language and conscious cognition and be etched directly into/onto the body itself “in its sinews and on its surface” (Casey 1987). The point is that the body (as the penultimate multisensory organ) is the site of interface with the physical, social and cultural world, and thus our experience in and of the world is perceived, first and foremost, by and in the body (Merleau-Ponty 1962). The experience of being-in-the-world is primarily ‘embodied,’ and only secondarily translated into conscious meaning. Csordas (1993) cites embodiment as the existential condition—that is, the ‘lived body’ is a “methodological starting point rather than …an object of study” (p. 136). However, embodiment, while ‘preobjective’ is not ‘precultural’; “the body is in the world from the beginning” (p. 9). Thus, approaching the placebo effect from a phenomenological paradigm of embodiment inverts the paradigm of conscious cognition that takes the objectified body for granted. Applying a phenomenological paradigm of embodiment demands analytical attention toward the ways in which placebo effects are manifestations of somatic modes of attention—that is, “the culturally elaborated ways of attending to and with one’s body” (p. 138).
In the last decade, the concept of embodiment as the way we “literally incorporate, biologically, the material and social world in which we live, from in utero to death” (Krieger 2005, p. 352, Table 1) has gained momentum in some corners of biomedical research (psychoneuroimmunology and psychoneuroendocrinology) and ecosocial epidemiology and life course biology. While it is reassuring that biomedicine and public health have begun to pay attention to the interconnections and feedback loops between physiology and direct sociocultural experience in the world, what are primarily considered are the negative impacts of embodiment—that is, in the profound effects of stress (Godbout and Glaser 2006; Kemeny and Schedlowski 2007), trauma (Hinton et al. 2001, 2006) and/or social inequalities (Krieger and Smith 2004) on the body. Just as negative experiences, like exposure to stress, violence and trauma, can cut deep grooves into the body such that negative health effects can become that body’s path of least resistance,Footnote 18 so, too, can healthful experiences carve positively embodied pathways to facilitate substantive positive health effects. Nevertheless, with the exception of work on the notions of resilience in social epidemiology and positive psychology (Haglund et al. 2007; Southwick et al. 2005; Taber et al. 2007), little attention has been paid to the positive effects of embodiment. Rather, it appears that many of the positive and resilient aspects of embodiment have been generally dismissed as ‘placebo effects.’
As an example of the positively embodied effects of direct sensorial experience, take the case of musician and musicologist Clive Wearing, whose amnesia following a brain infection of herpes encephalitis has rendered him unable to maintain his memory for more than a few seconds at a time (RadioLab 2007; Sacks 2007a, b; Wearing 2005). This condition has persisted for over 20 years, with Wearing awakening from what he characterizes as ‘death’ every few minutes. Despite this near-complete loss of conscious memory, Wearing’s musical skill and his abiding love for his wife continue to resonate with his very being. In a narrative analysis of Wearing’s case, Oliver Sacks makes it clear that these connections are not the result of conscious, cognitive memories. Rather, they are deeply embodied and sensorial:
Clive and Deborah were newly married at the time of his encephalitis, and deeply in love for a few years before that. His passionate relationship with her, a relationship that began before his encephalitis, and one that centers in part on their shared love for music has engraved in him—in areas of his brain unaffected by the encephalitis—so deeply that his amnesia, the most severe amnesia ever recorded, cannot eradicate it.
Nonetheless, for many years he failed to recognize Deborah if she chanced to walk past, and even now he cannot say what she looks like unless he is actually looking at her. Her appearance, her voice, her scent, the way they behave with each other, and the intensity of their emotions and interactions—all confirm her identity, and his own. (Sacks 2007a, b)
As this example makes clear, re-experiencing healthful sensations, sensory experiences or emotions that have been inscribed directly into the body can bypass conscious awareness and ‘meaning’ and prompt what Frenkel (2008), following Dreyfus, might refer to as a “skillful and unreflective” response at the site of the body.Footnote 19
Richardson (1982) observes that lived experience is also channeled into objects, thus transforming them into powerful symbols that themselves catalyze, stimulate or trigger powerful, evocative multisensorial experience. Spaces and places are also invested with and transformed by lived experience (Basso 1996; Cartwright 2007; Low 2003). Although they are often dismissed as ‘placebo effects,’ responses that enhance healing can be directly (unconsciously) triggered by objects (e.g., a Band-Aid or a pill in conventional medicine) or places (e.g., the sterile doctor’s office or the warm décor of the Western acupuncturist’s office). Within biomedicine, this effect is illustrated by the emerging literature on optimal healing environments (Dijkstra et al. 2006; Malenbaum et al. 2008; Schweitzer et al. 2004; Ulrich 1984).
The characterization of placebo as meaning, expectation or even desire is phenomenologically and evocatively dry. Just as illness etched into the body and into symbols and spaces can make us feel or be ill, healing and positive affect can be etched into the body and into symbols and spaces to genuinely make us well. The point is that the body can directly respond to sensory or affective stimuli and it does not require meaning in any consciously cognitive sense to catalyze a placebo response.
So how does this all relate to the placebo effect? From a physical reductionist perspective, the symbolic significance of, or emotional or aesthetic reaction to, any given treatment should not have an effect on its outcome. But it clearly does. Our point here is that these symbolic, emotional and aesthetic elements cannot be boiled down to expectation, desire or meaning, per se. These elements may be registered directly at the site of the body—bypassing conscious awareness and etching themselves “in its sinews and on its surface” (Casey 1987). Yes, there are multiple things held in tension here: conscious awareness versus direct embodied experience; cultural versus personal symbols (as well as associated meaning and knowledge); past experience etched on the body versus emergent experience that is shaped and constrained, but not dictated by the past; rational versus sensory or emotional responsiveness. However these facets of lived experience are not dichotomies as much as they are nodes in the complex web of what it means to be-in-the-world.
Performative Efficacy
A performance approach lends insight into understanding the embodied and directly experienced facets of the placebo effect. Key to this approach is the extension of Austin’s (1962) concept of performative efficacy from the realm of language to the body itself. Austin argues that, in the case of performative utterances, “saying make[s] it so” (e.g., “I quit” or “I now pronounce you husband and wife”), and Tambiah (1979) has fruitfully applied the concept of performativity to ritual. We further extend this notion to suggest that therapeutic performances (both social and internal) may exert perlocutionary force on the body. That is, doing makes it so.Footnote 20 In other words, we suggest that healthful outcomes often dismissed as placebo effects by mainstream medicine may be productively analyzed through a performative lens.
Social Performativity
Performance is not merely representative, but constitutive of social and cultural life. Goffman (1959) and Butler (1990) argue that sustained performances enact social reality. Butler goes beyond Goffman’s discussion of the performance of social roles by stressing that repeated social performances enact identity at the site of the body. To what degree do practitioners, patients and others in fact catalyze the placebo effect via mutually reinforcing performances of social roles? Kaptchuk (2002) makes the argument that alternative medicine (CAM) may be well poised to enhance placebo responses by “administering an especially large dose of…performative efficacy” (p. 817). Importantly, Kaptchuk argues that a consideration of performative efficacy in healing (whether in biomedicine or CAM) draws much-needed attention to the importance of clinical significance of treatment (that is, a patient’s improvement from his or her own baseline versus the relative improvement of this intervention vis-à-vis an alternative intervention).
One clear example of performative force in healing is the power of diagnoses and prognoses to affect and mobilize resources and social support. Bandura (1997) has found that “prognostic judgments activate psychosocial processes that can influence health outcomes rather than simply serving as nonreactive forecasts of things to come.” Brown (2003) takes this a step farther to argue that expectation, itself, is constitutive and performative. Simply put, expectation performatively “mobilizes the future into the present.” Furthermore, “within communities of promise, expectations structure and organize a whole network of mutually binding obligations” (p. 6).Footnote 21 Traditional explanations of expectancy stress that expectation stimulates conscious desire and motivation to do more for oneself, which can lead to improved health outcome. A social performative interpretation points out that expectation is itself constitutive and performative (Brown 2003), in that it affects change on a level that can bypass conscious cognition and operate directly on the body and on social structure.
Performativity, itself, fundamentally reorganizes social relationships, or reorients the self in the world. For example, Nordstrom (1998) describes a ceremony held for a woman who “was physically sick and emotionally traumatized” by war in Mozambique (Nordstrom 1998, p. 114). During the ceremony, “women picked up the patient, and carefully gave her a complete bath, which was said to cleanse her soul as well as her body” (p. 114). After being fed and dressed in new clothing, the patient is carried into the hut, where women tend to her physical and emotional wounds. They hold her, rock her and speak of “rebirth in a healthy place among people who cared for her.” Finally, the women carry the patient outside “where the community welcomed her as a part of it” (pp. 114–115).
As this moving example illustrates, social performance is not merely representative of social life; it has the power to be constitutive of physical and social well-being by mobilizing the support and resources that set healing in motion and see it through to completion. While these types of healing rituals—to reintegrate soldiers and victims of war—exist across cultures, what is significant is that they are local, creative and adaptive responses to the need for healing, on an individual and social level.
Within biomedicine, the power of social performativity to catalyze something of a placebo response may be best illustrated by examples of sham-controlled surgical trials in which patients who undergo sham surgery have outcomes as good as those of patients who undergo the real thing (Birch 2006; Freed et al. 2001; Moseley et al. 2002). In the majority of these surgical trial scenarios, both sham and real groups receive the same surgical incision and postoperative care by medical staff, who are blinded to group assignment. In fact, this example begs the question: What is the ‘active’ element of surgery? A number of theories have been posited to explain the strong performance of sham surgery, including the therapeutic benefit of bloodletting and the self-healing mechanisms triggered by the incision itself (Birch 2006). We suggest, however, that social performativity may also be part of the equation. Assembling a full surgical and rehabilitation team that is committed to “playing their parts” in the surgical performance may potentiate a scenario in which patient expectation is performatively transformed into therapeutic effect.
Perhaps the simplest example of a performative placebo effect may be seen in the effectiveness of a mother’s kiss on a toddler’s skinned knee. As any parent knows, this act has the power to eliminate pain and stop the flow of tears almost instantly—far better than a hug and an ‘I love you.’ One would be hard-pressed to argue that the effect these actions have on the experience of pain in a very young child are ‘consciously cognitive’ or based solely in ‘meaning.’ The kiss is directly sensorial, embodied and clearly performative: doing it makes it so.
Internal Performativity
Anyone who has played a musical instrument or played on a sports team knows that practice, or rehearsal, plays a key role in skilled performance. In fact, proficiency in these fields requires that the fundamental skills become fully integrated in the body such that they become what Bourdieu (1977) characterizes as habitus: those bodily and social ‘dispositions’ that have become internalized and historicized to the degree that they operate within a given field as second nature.
Recent neuroimaging studies of musicians confirm the extraordinarily plasticity of the brain in response to training demands (Munte et al. 2002; Pascual-Leone 2001; Schlaug 2001), and there is a substantial body of evidence that musicians and athletes benefit from “mental practice” (that is, imagined or visualized rehearsal) as well as from physical practice (Denis 1985; Mendoza and Wichman 1978; Pascual-Leone 2001; Schonberg 1987, 1988). Recently, for example, Smith and Holmes (2004) found that golfers who listened or watched internal-perspective recordings of themselves putting performed significantly better at putting tasks over six weeks than those who read golf literature for an equivalent amount of time.
We suggest that the efficacy of mental practice resides in its performativity—that is, doing (even in the mind’s eye) makes it so. This framework may provide an avenue for considering some placebo effects as the manifestation of internal performativity, in which the practice of rehearsing and/or imaging a particular state of health may itself have perlocutionary force in the body. Although there has been little research on the efficacy of internal performativity in health-care settings, there is increasing interest in applying sports science to therapeutic and rehabilitation settings. Recent evidence suggests that these internally performative methods (including mirror therapy) may be of therapeutic value in the rehabilitation of stroke victims (de Vries and Mulder 2007; Yavuzer et al. 2008).
The discovery of mirror neurons, which appear to play an important role in understanding the goals, intentions and emotions of others, and perhaps in complex cognitive processes such as language acquisition (Rizzolatti et al. 2006; Rizzolatti and Craighero 2004), may suggest a physiological pathway by which internal performativity is effective.Footnote 22 De Vries and Mulder (2007) review the evidence indicating that ‘offline actions’ such as imagining and observing movements trigger the firing of mirror neurons that may be able to activate neural reorganization. It may follow that internal performativity focused on healing (whether it be through mirror therapy, direct observation, audio stimulation, guided imagery, etc.) may alter neural networks in ways that inscribe healing action in the brain and body.
Neurobiological Mechanisms
The vast majority of research into the physiology of placebo effects has been undertaken by Benedetti et al. (2005), who see the placebo effect as a “psychobiological phenomenon” (p. 10390). These researchers argue that “the placebo effect appears to be a very good model to understand how a complex mental activity, such as expectancy, interacts with different neuronal systems” (p. 10390). Here, we briefly consider two domains in which neurobiologists are working to unravel the complex neurobiology underlying the placebo effect: placebo analgesia and depression.
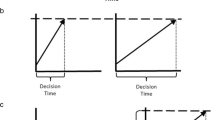
Placebo analgesia can be induced by both expectancy and conditioning. Expectancy-induced placebo analgesia results in an endogenous opioid response (indicated by reversal by naloxone),Footnote 23 whereas conditioning results in either an endogenous opioid response or a nonopioid response, depending on the US (Price and Sorensen 2002). In an effort to better understand which bodily systems are implicated in expectancy versus conditioning-induced placebo effects, Benedetti et al. (2005) found that expectancy could antagonize conditioned placebo analgesia and motor performance, and they found no changes in hormone secretion based on expectancy. These findings have important implications for understanding the translation of psychosocial triggers into the neurobiological processes.
Placebo researchers from diverse fields agree that depression and the high rates of placebo response in clinical trials of pharmaceutical and psychosocial antidepressant therapies provide fertile ground for investigating the placebo effect (Benedetti et al. 2005; Kirsch 2002; Kirsch and Sapirstein 1998; Lakoff 2007).Footnote 24 The changes observed in the brain images of placebo responders in depression treatment studies appear to track those changes observed in active treatment responders; however, the patterns of these changes vary according to active treatment, “refuting the hypothesis that placebo response is mediated by changes in a common antidepressant response pathway. These findings additionally suggest that placebo response is also not the result of uncontrolled, unspecific psychological treatment effects” (Benedetti et al. 2005, p. 10398).
While researchers of the physiology of the placebo effect are primarily interested in basic science underlying the way “psychosocial context” (very narrowly defined as expectancy and conditioning) is translated into the brain and body, they identify a number of practical implications—which harkens back to Caspi's (2003) clinically oriented message: To optimize care for patients, health-care providers must learn to catalyze the placebo response in active treatments.
Based on the neurobiological evidence provided by Benedetti et al. (2005), it is becoming increasingly clear that the placebo effect cannot be characterized as a singular phenomenon. Rather, placebo effects may be triggered by any number of stimuli, including conditioning, expectancy, therapeutic relationship and sociocultural meaning. Furthermore, stimuli may act through any number of biological pathways (some identified and others still unknown) including endogenous opioid, immune and hormonal pathways, among others. By illustrating that placebo responses are yoked to the intervention at the brain level, Benedetti et al. (2005) demonstrate that placebo responses are not limited to a few neurobiological mechanisms. It may be that every part of the brain can participate in the placebo response.
Healing in an Evolutionary Context
It is becoming ever more apparent that ‘the placebo effect’ is polymorphic in both its trigger and its expression, and that the mechanisms for placebo responses within the body are diverse. It is also clear that in all societies, healing modalities have developed to maximize the placebo response in an attempt to overcome assaults to well-being. This raises the question whether the placebo response, like other self-healing mechanisms, may be an evolutionary adaptation.
While it is beyond the scope of this paper to review the evolutionary evidence for self-healing in detail, we would like to describe briefly what we see as a multilevel, cells-to-society approach that supports this evolutionary contention. Let us begin at the most basic level by providing three examples of self-healing—at the cellular, organismal and psychosocial levels—to illustrate the selective pressures that underpin wellness.
At the most basic, cellular, level, there are multiple mechanisms to repair (“heal”) DNA that has been damaged during cell function or replication. Among these are DNA damage response reactions that can: (1) remove DNA damage and restore the functioning double helix; (2) stop the process of mitosis to allow for repair and prevent the transmission of mutated DNA; (3) alter the portions of DNA that can be transcribed, to protect the cell from damage; and (4) initiate programmed cell death (apoptosis), which safely eliminates severely damaged cells (Sancar et al. 2004). Cancer appears to be a consequence of these processes being inactivated or overwhelmed (Mahoney 2007). In light of the high incidence of DNA errors, the relatively low frequency of cancer occurrence is a testimony to the effectiveness of this system.
A second example of self-healing at the cellular level involves mechanisms to protect cellular structures and processes from damage that would be caused by oxidative stress. In the course of normal cellular function, a variety of reactive oxygen species (ROS) is produced inside cells. In addition, many cells are exposed to oxidation from exogenous sources, such as sunlight or the bloodstream. A large number of mechanismsFootnote 25 quench reactive oxygen species, repair proteins that have been damaged and move compounds into safe places inside the cell in preparation for excretion (auf dem Keller et al. 2006; Thorpe et al. 2004). Considering that much of the basic research on mechanisms for protecting against or healing the damage of oxidative stress has been done on yeast, it is clear that certain ‘self-healing’ properties, such as antioxidation mechanisms and DNA repair systems, are evolutionarily ancient (Thorpe et al. 2004).
Wound healing and the immune response are the most obvious mechanisms for protection and self-healing at the level of the organism, and they share underlying mechanisms. While we all have biopsychocosocial experiences of wound healing (i.e., a mother’s kiss, also see Detillion et al. 2004), the full range of overlapping physiological and biochemical mechanisms that make up and modulate processes of inflammation, proliferation of new cells and remodeling of tissue to accomplish this wound healing are extraordinarily complex and not yet fully understood (Schafer and Werner 2007; Shilo et al. 2007). Wound healing includes the recovery from broken bones as well, and the mechanisms behind the control of each component of the cellular processes involved are similarly not understood (Dimitriou et al. 2005).
Also at the level of the organism, the immune system is made up of components that provide protection from and healing of invasions by undesirable organisms, from single-celled (bacteria, etc.) to complex parasitic organisms. The innate immune response, which is genetically encoded to recognize and protect against specific structures foreign to cells, is evolutionarily ancient, and even bacteria exhibit this response against viruses (Barton 2008; Medzhitov 2007). The acquired immune response, which results in what we usually think of as ‘immunity’ due to the creation of new specific antibodies to foreign antigens, is a characteristic of all land vertebrates (Fietta 2007; Girardi 2007; Medzhitov 2007). What we experience as the illness of infection is often the organismal response to invasion. Inflammation, fever, fatigue, even body aches are the result of cytokines and chemokines released by cells all over the body (local and distant to the site [Murphy 2007]) to help defeat invading organisms (Libby 2007). Healing from an infection requires both that the invading organism be essentially eradicated and that the immune response be reduced to a normal level. Chronic infection, chronic inflammation and autoimmune diseases are all examples of a hyperactive immune response (Maggini et al. 2007; Netea et al. 2008).
A third, less visible, set of mechanisms at the level of the organism are those that remove toxins from the body, irrespective of whether those toxins are exogenous assaults or endogenous by-products of normal cellular function or inflammatory immune response. For example, the activities of cytochrome P450 (cyp450) enzymes are so specific in removing environmental toxins that the human excretion of metabolites can provide information on environmental exposures to chemicals such as PCB and DDT (Lampe and Chang 2007; Yi et al. 2007).Footnote 26 While these mechanisms protect the organism from harm, they also heal by removing toxins created in the inflammatory responses, thus enhancing the return of health following infection.
Thus, from an evolutionary perspective, biological mechanisms that provide protection from harm and enhance healing are central components of organismal survival. Certainly, the capacity to recover from insults would enhance individual fitness, and any genetically encoded biological traits that enhanced fitness in this way would be under positive selective pressure.
On a psychosocial level, the complex interrelationships between brain function and self-healing mechanisms are being studied within the fields of psychoneuroimmunology and psychoneuroendocrinology (DeVries et al. 2003). For example, psychosocial stress, especially within social interactions, and negative emotional states, such as depression, can alter hormonal factors and hinder fertility (Novack et al. 2007). These psychosocial conditions can also hinder wound healing and the function of the immune system. As an example, caregivers (often adult children) of Alzheimer’s patients show greater susceptibility to infection, slower immune responses and slower wound healing (Christian et al. 2006; Damjanovic et al. 2007; Detillion et al. 2004; Mills et al. 2004). Further, it appears that physical states such as chronic infection can precipitate or worsen psychological conditions, including depression, demonstrating that these are truly interrelationships rather than unidirectional causal pathways (Irwin and Miller 2007). What is clear is that the body-mind is highly integrated, and insults in any location can affect the organism as a whole. The concept that the body and mind are somehow distinct—encoded in language such that there is no scientific word to effectively connote full integration between the two—is clearly an inadequate picture of the human organism.
On the basis of this evolutionary evidence, we argue that the neurobiological mechanisms of healing discussed above can link direct embodied experience—including performative and sensory experience—to changes in immunologic, endocrinologic and pain responses. These responses would be under positive selective pressure throughout mammalian and human evolution. Given the varieties of human experience (with variation in physical environments, population size, family and social structure and sociocultural experiences across the life course), local biocultural feedback loops are likely to exert selective pressure on a range of self-healing responses. Further, as the substrate for selection is random variation, the variants available for selection will differ among populations. For both of these reasons, it seems highly plausible that there would be a wide variety of mechanisms that link the body-mind to local biocultural conditions and, hence, provide populations with a broad range of sites for interventions with the potential to enhance health. Given the genetic and psychosocial variability among individuals and between populations, the likelihood that a single mechanism will enhance healing in all individuals in all situations is highly unlikely. Assuming that the ‘placebo response’ is a highly polymorphic trait in human populations that has been under local selective pressure for thousands of years, it is reasonable to expect that pluralistic healing modalities would emerge that trigger a ‘placebo response’ in multifarious ways.Footnote 27
Thus we suggest here that what has been disparagingly called the placebo effect, and has been relegated to the category of a nuisanceFootnote 28 in RCTs, is in fact an evolutionarily adaptive trait. It is adaptive (for the individual and the social group) to be well, and the mindful body will use every tool at its disposal (material, social, psychological and symbolic) to maintain or restore well-being. The ability of an organism to respond to resonant (rather than precise) therapeutic triggers would be under positive selective pressure. For the individual organism, responding to a ‘placebo’ may enhance the probability of wellness and the survival of offspring and, thus, may be a precursor to biological adaptation that produces an enduring and reproducible therapeutic effect. In addition, any social mechanism that would support or trigger a placebo response (such as ritual, empathy, altruism, positive social relations, etc.), and would enhance the resilience of the organism to return to wellness, would be under positive selective pressure on a social level.
Conclusion
In principle, all resonating systems have this peculiarity that all parts of the system will be changed when any part is changed. So that to sense organs which can register the change, all parts of the system carry information about the change. In other words, there is a redundancy between all parts of such a system. In principle, all resonating systems have hologramic characteristics.
—Bateson (1975, p. 135)
In our conclusion, let us summarize our case for how placebo might be better conceptualized, note why exploring the concept of placebo is vitally important to anthropological and ‘whole systems’ studies of the healing processFootnote 29 and identify some directions for future research.
Within biomedicine, the ‘placebo effect’ has been characterized in multiple ways: as something to control in clinical research, something to cultivate in clinical practice and something present in all healing encounters. Just as the language of atoms became obsolete for discussing the intricacies of interactions at the subatomic level, we argue that the field of placebo research has grown in richness and sophistication to the point where the language of ‘placebo’ restricts our ability to think about complex healing.Footnote 30 Researchers increasingly require more subtle ways to examine and describe the variety of catalysts involved in self-healing. In this paper, we have considered how the full range of human experience may catalyze a ‘placebo response.’ As a corrective to what we view as an overemphasis on conscious cognitive approaches to understanding placebo, we shifted analytical focus and argued that direct embodied experience may take precedence over meaning-making in the healing encounter. As an example, we examined the neurobiology of rehearsing or visualizing wellness as a mode of directly (performatively) producing an outcome often dismissed as “placebo.” Given body/mind/emotional resonance, we further suggest that the placebo response is an evolutionarily adaptive trait and part of healing mechanisms operating across many levels—from genetic and cellular to social and cultural.
This paper makes a contribution to the emerging field of evolutionary medicine. Evolutionary medicine has been considered from several perspectives over the last few decades. For example, in an early review of the field, Williams and Nesse (1991) urge biomedicine to pay more attention to the evolutionary underpinnings of disease. They suggest that the role of natural selection plays out in four disease-related arenas: (i) infection, (ii) physical injury, (iii) genetic disease and susceptibility to disease and (iv) diseases of “civilization.” Biological anthropologists have long called attention to human plasticity and the role that older evolutionary adaptations may play in modern disease trajectories and health sequelae (Eaton et al. 1988; Krogman 1951; Lasker 1969; Livingstone 1958; Trevathan 2007; Washburn 1951). Recently, Trevathan et al. (2008) presented us with an edited volume of case studies illustrating how a wide range of contemporary ills (including nutritional deficiencies, reproductive concerns, psychological disorders and chronic diseases) may be the result of “mismatches” between the contemporary human physical, social and psychological context and the environment in which our species evolved (Trevathan 2007).
Life-course epidemiologists have further drawn our attention to the long-term negative health effects of physical and social ‘exposures,’ beginning in gestation and continuing throughout life (Ben-Shlomo and Kuh 2002; Kuh et al. 2003). Ecosocial epidemiologists have critically examined the cumulative impact of sociopolitical context on disease and illness (Berkman and Kawachi 2000; Krieger 2000, 2001, 2003; Krieger and Smith 2004; McKinlay and Marceau 2000; McLaren and Hawe 2005). What is clear from these studies is that humans do not statically react to life experience; our local biology adapts in response to stressors and assaults in the physical and sociopolitical environment (Hertzman 1999; Krieger 2005) such that what is embodied over the life course is patterns of biosocial response with long-term impact. Abundant examples exist in the literature to illustrate that short-term coping responses may have harmful consequences over the longer term.Footnote 31
At the level of sociocultural responses to illness, Fabrega (1997a, b)Footnote 32 has employed an evolutionary medicine lens to examine the emergence and “evolution” of sickness and healing as a response to social and cultural selective pressures, specifically changes in social organization. What we would add to an evolutionary medicine agenda is the study of ‘placebo response’ as a core biosocial dimension of the ‘resilient’ side of the evolutionary equation. In this paper we argue that the human capacity to develop and respond to resonant, rather than precise, healing triggers (‘the placebo response’) is adaptive and catalyzed in a multitude of ways by pluralistic healing systems.
Let us end by suggesting four important directions for future studies of the placebo response.
Placebo effects are local biopsychosocial phenomena and, as such, can only be understood in terms of local biologies. Lock introduces this term to describe the “ongoing dialectic between biology and culture” (1993b, p. xxi) such that “both…are subject to transformation in evolutionary, historical, and life cycle time bytes and to movement through space” (1993a, p. 146). This concept is central to understanding both biological responses to sociocultural triggers of ‘placebo response’ and the sociocultural evolution of healing systems that potentiate placebo responses.
Second is the issue of temporality. Although there is evidence that placebo effects for Parkinson’s patients can endure (McRae et al. 2004; Price et al. 2008), clinical studies of depression suggest that placebo antidepressant effects fall off after a certain length of time, while pharmaceutical effects are sustained (Benedetti et al. 2005). Future studies of the placebo response need not only to investigate who experiences a placebo response, and under what conditions, but also to ask How is the placebo response sustained? How is it recharged? and What conditions undo a placebo response?
This brings us to the third important line of investigation: the sociality of the placebo response. Nichter (1981a, 2008) suggests that the effectiveness of idioms of distress and concern resides in their initiation of feedback loops of positive social support for the individual. Similarly, a placebo response may be mediated by a sociocultural environment that provides positive or negative feedback regarding treatment. While support and encouragement from friends and family may help to boost placebo responses to treatment, placebo responses can be undone by naysayers. This concept highlights the need to investigate features such as collective efficacy and social support elements at work in initiating and maintaining a placebo response/effect.
Finally, studies of healing mechanisms, including the placebo response, may be productively approached from a complex systems perspective. In a follow-up paper, our working group will investigate in greater detail how healing responses are triggered by diverse biosocial stimuli from local and novel sources. We will use research on patient experiences of CAM therapies as an opportunity to explore diverse dimensions of healing that are underprivileged—if not overlooked—in biomedical research. While CAM and whole-systems research offer fertile sites for the exploration of these issues on both theoretical and methodological grounds, it is our contention that these lines of inquiry are vital to the future of biomedicine as well (IOM 2005a, b).
Notes
The flip side of the ‘placebo effect’ has been referred to as the ‘nocebo effect.’ This term has been used in a number of ways to indicate the negative effects associated with ostensibly ‘inert’ treatments in practice and research (Barsky et al. 2002; Benedetti et al. 2007; Bootzin and Bailey 2005; Caspi 2002; Hahn 1999; Helman 2001). Bootzin and Bailey (2005) observe that “the fact that placebos and nocebos elicit a pattern of reactions in symptom relief and side effects that is similar to that produced by the medication or intervention to which they are being compared means that mechanisms of action for either specific or nonspecific effects must be able to account for the complex patterning of results” (p. 873). Clearly, understanding nocebo effects may be at least as complicated as understanding placebo effects. While it is beyond the scope of this paper to examine nocebo effects, we view this as an important future direction for research.
Although there is a well-developed literature on the cognitive unconscious—including implicit perception, learning and thought (Kihlstrom 1987, 1996)—the vast majority of the literature on the placebo effect (with the exception of work on a conditioned placebo response) privileges a state of conscious awareness on the part of the patient in its explanations of the placebo effect.
Bootzin and Caspi (2002) offer another useful way of framing this issue. Specifically, their definition of ‘placebo response’—a patient’s positive (placebo) or negative (nocebo) response to treatment (broadly construed) stemming from the ‘incidental’ or ‘preliminary’ therapeutic elements—vis-à-vis those treatment responses specifically attributable to ‘defining or characteristic elements’ intended to be “causally responsible for the outcome” (see also Caspi 2003).
This schema suggests the need to deconstruct the notion of healing intent. Most simply put, one practitioner’s placebo may be another’s ‘active’ treatment. Within biomedicine, take the example of diagnosis itself. While the healing intent underlying physicians’ diagnosis has not been systematically studied, Brody and Waters (1980) argue that the diagnostic process itself is a powerful therapeutic tool—especially for behavioral problems for which diagnosis provides an explanatory system that gives meaning to otherwise unexplainable suffering and symptoms. Further research is needed on what elements practitioners (biomedical, as well as complementary and alternative) consider ‘active’ vs. incidental. While randomized controlled trials (RCTs) narrowly define the ‘active’ treatment according to the biomedical paradigm of disease (and treatment) specificity—thus relegating everything else to the category of ‘nonspecific’ or ‘incidental’—it is not clear whether practitioners themselves would agree with this distinction.
While the notion of a placebo-controlled clinical trial was created to help health-care providers decide between pharmaceutical treatments, it has become an increasingly thorny and politicized issue. The U.S. Food and Drug Administration (FDA), which regulates and approves pharmaceuticals for the lucrative U.S. drug market, privileges evidence from placebo-controlled clinical trials. There is increasing pressure from the World Medical Association’s Declaration of Helsinki for pharmaceutical companies to use active controls (often the current standard of care) whenever a condition has a ‘proven therapy’ (http://www.wma.net/e/policy/b3.htm). To cut costs, more rapidly recruit naïve subjects and avoid having to offer subjects expensive, gold-standard therapies during or following trials, pharmaceutical companies seek out patient populations (frequently Third World, underprivileged and underserved patient populations) that are willing to submit to placebo-controlled clinical trials because they do not have access to standard-of-care treatments. Pharmaceutical companies have thus found it more cost-effective to run clinical trials overseas (Shah 2006). Critics argue that placebo-controlled trials are examples of the pharmaceutical companies’ “stacking the deck” in their favor: “Why risk trying to be better than something…when all you need to show is that you are better than nothing?” (p. 33).
With respect to complementary and alternative medicine (CAM) therapies and procedures, the National Institutes of Health (NIH) frequently demands that clinical trials of all kinds of therapies be placebo-controlled. Conflicts between researchers and funding/regulating agencies arise as to what, precisely, is the active element of a CAM therapy and how to design a study with an appropriate placebo arm. Bootzin (personal communication) argues that the concept of placebo—as it is used in clinical trials—is limited to testing a specific mechanism of action and tells us little about the overall therapeutic effectiveness of a given intervention. In fact, some critics argue that the FDA and NIH have become more concerned with mechanism than with outcome (Kaptchuk 1998).
Ader (2000) similarly observes that the notion that “real” drug effects can be parsed out in clinical trials is a gross oversimplification. “Drug effects can only be evaluated in vivo… There are no ‘real’ drug effects outside of those observed in a behaving organism.” He argues that “we have no a priori right to assume that placebo effects and drug effects are additive. It may be more reasonable to hypothesize that they interact in complex ways that have not been studied in any systematic manner.”
A recent meta-analysis of all clinical trials on four ‘new-generation’ antidepressants, which used data obtained from the FDA through the Freedom of Information Act, found that these drugs provide only slight, if any, statistical benefit (and did not reach clinical significance) over placebo in mild to moderate depression (Kirsch et al. 2008; Mayor 2008). Furthermore, while these antidepressants appear to provide somewhat more benefit to those with the most severe depression, this is due more to a decrease in the placebo response among the most severely depressed than to an increase in the drug response.
According to some researchers, CAMs, which operate within novel paradigms that are responsive to patient individuality on the level of diagnosis and treatment, may be particularly well positioned for activating the placebo effect in clinical practice (Kaptchuk 2002). This has created a conundrum in which the efficacy of CAM therapies may be rendered ‘just’ placebo effects (Bausell 2007; Beyerstein 2001; Shang et al. 2005). Bootzin and Caspi (2002) argue that this ‘placebo problem’ in CAM is not insignificant:
If indeed the incidental elements of CAM are those that account for its effectiveness, then health care providers need not necessarily be skilled in any of the CAM techniques but rather should be trained to activate the placebo effect/healing system pathways. However, if the therapeutic relationship enhances rather than substitutes for the treatment…then all practitioners need to be trained to activate healing pathways. (p. 125)
To be fair, the ENHANCE study was not a placebo-controlled clinical trial, but a study of the combination drug (Zetia and Zocor) versus Zocor alone (Kastelein John et al. 2008). Nevertheless, the idea persists that Zetia was just “an expensive placebo” circulated in the media, especially on Internet blogs (http://www.forbes.com/2008/04/04/schering-merck-vytorin-biz-healthcare-cx_mh_0404floor.html?boxes=custom). Another example is the dramatic drop in sales of Quaker Oats following the media attention to a flawed study indicating that oat bran had no cholesterol-lowering effect (Bausell 1990; Lehman 1990; Swain et al. 1990).
This broadcast came out while we were working on the early drafts of this paper. We authors were pleased to find this broadcast a remarkably robust media treatment of this topic, which touched on many of the issues we cover here. It can be found online at: http://www.wnyc.org/shows/radiolab/episodes/2007/05/18.
Unfortunately, says Benedetti (2008), our internal pharmacy “sometimes does not work”—that is, while the placebo effect (in this case, the stimulation of our endogenous production of a therapeutic substance) is “incredibly powerful, it’s rarely consistent. It’s hard to predict who’s going to get a placebo effect under what circumstances.”
Inadvertently conditioned ‘nocebo’ effects are also well documented. A well-known example is that of conditioned nausea among chemotherapy patients, in which up to one-third of patients “become profoundly nauseated when encountering a previously neutral stimulus that has now become associated with the chemotherapy, such as meeting the infusion nurse outside the hospital or entering a room painted the same color as the infusion room” (Barsky et al. 2002, p. 624).
The concept of “placebo” is a biomedical construction. When we use nonbiomedical or cross-cultural examples in this paper, readers may wonder whether we are implying that these are examples of ‘sham’ healing. Of course, we are not. We use these examples to illustrate oft-overlooked aspects of healing, a number of which have been disparagingly referred to as ‘placebo effects’ in biomedical literature.
Elsewhere, Bootzin and Caspi (2002) have identified other “preliminary elements of treatment”—such as the decision to seek treatment in the first place, as well as the diagnostic process (including testing and diagnosis)—that may also set in motion certain expectations on the part of the patient and that may, in turn, trigger a shift in patient practice and/or the body’s homeostatic healing response. These elements may be located prior to the clinician-patient relationship on this same ‘cognitive’ trajectory.
Moerman (2002a, p. 121) argues that each time a patient takes a pill, he or she “recalls” the entire medical experience. We must stress that the connection goes beyond the patient’s cognitive connection with a past medical experience. In fact, the pill is a metonym (part representing the whole) for all of biomedical technology. Each time the patient takes the pill, he or she indexes the technological and symbolic power of biomedicine.
The feelings associated with apple pie may able be associated with the mammalian attraction to safe and sweet foods.
Examples include culturally specific manifestations such as ‘sore neck syndrome’ among Khmer refugees (Hinton et al. 2001), as well as biomedicalized manifestations such as PTSD and anxiety attacks.
We thank the reviewers for bringing our attention to Frenkel’s (2008) recently published phenomenological account of the placebo effect. Although we disagree with Frenkel’s wholesale disregard of expectancy theory and his contention that placebo responses are better referred to as “meaning responses,” we appreciate his application of Merleau-Ponty’s (1962) notion of ‘motor intentionality’ to this topic. Bringing in Dreyfus’s (1999) work on ‘absorbed coping’ and his own concept of ‘affordances of healing,’ Frenkel (2008) constructs a compelling argument for the “sentient body, capable of responding to the world without having to invoke any reflexive activity” (p. 70).
Like ‘classical conditioning’ models, both Frankel (2008) and Ader’s (1997, 2000) frameworks suggest that the body ‘learns’ from past experience. However, an embodiment paradigm differs from conditioning in that it operates on multiple senses engaged in the world rather than relying on the direct pairing (and later withdrawal) of an unconditioned stimulus with a conditioned stimulus to stimulate the desired therapeutic effect.
Strictly speaking, we are operating outside the domain of the placebo effect, as the perlocutionary force of performance—which, by definition does something—cannot be considered ‘inert.’
In contexts of collective intervention, such as surgery and ritual, collective efficacy, that is, “a group's shared belief in its conjoint capabilities to organize and execute the courses of action required to produce given levels of attainments,” may also catalyze a positive feedback loop to maximize both the performance of team members and the patient’s placebo response, thus enhancing the overall therapeutic effect (Bandura 1997, p. 477).
When an individual observes an action of another, the mirror neuron system (discovered in macaque monkeys and indirectly proven to exist in humans) activates as if the individual were performing the action him- or herself. The mirror neuron system can also be triggered—although to a lesser degree—by audio stimulation (that is, hearing a sound that represents a particular action such as the ripping of a sheet of paper) or by observing a ‘goal’ of which the action is implicit (for example, seeing a basketball go through a hoop). In a study of the translation of verbal stimulus into neural networks, for example, Pulvermuller (2001) found topographic differences in the brain activity between subjects who listened to action verbs related to leg-related activities (such as “walking,” which stimulated cortical leg areas of the brain) and subjects who listened to face-related action verbs (such as “talking,” which stimulated cortical areas related to the motor representation of the face and mouth).
The mirror neuron system appears to come into play in interpersonal emotions such as empathy, as well. For example, when an individual observes another person in pain or disgust, mirror neurons track that emotional experience in the observer’s brain. Rizzolatti et al. (2006) suggest that this process bypasses consciousness and provides a “direct mapping of sensory information onto motor structures that would produce the experience of that emotion in the observer.” What these studies indicate is that audio and visual stimuli can influence the body’s neural networks, affecting physical performance as well as emotional experience.
Mirror neurons (or some structure similar to them) may have implications for anthropology that have yet to be explored. For instance, internalization of cultural knowledge may be the work of mirror neurons constructing neurological pathways based on the observation, sensation, emotion and practice of cultural schemas. It may be that habitus and the internalization of culture are the result of mirror neurons building up neural pathways from childhood. Furthermore, mirror neurons may help us better understand biocultural feedback loops, including the way that the external world shapes our internal world (by building up neural pathways based on observation, sensory input, emotion and practice) and, conversely, the way our internal world (given structure and coherence by a lifetime of neural pathways) affects our external world (manifesting these pathways externally through action).
Although there is strong evidence that expectancy-induced placebo analgesia is the result of endogenous opioid production, Benedetti et al. (2005) posit that positive expectations may also affect other body systems that can help individuals better tolerate pain by decreasing anxiety, increasing positive emotions and activating reward systems.
Lakoff (2007) cites studies indicating that depression trials result in placebo response rates of 15 to 70 percent, with verum (or study drug) response rates of 30 to 70 percent, although Benedetti et al. (2005) stress that “significant short-term placebo response rates are in contrast to continuation studies that demonstrate a significant advantage of maintenance medication over continued placebo treatment in preventing relapse and recurrence” (p. 10396). Given the complexity of the phenomenon labeled ‘depression’ and the many confounds of clinical studies of depression therapies, including that research subjects are often veterans of depression, depression treatments and drug trials, Benedetti and colleagues argue that there is a “complex interaction between mechanisms mediating expectation and conditioning effects for a given antidepressant and the heterogeneity of the depressed patient population under study” (p. 10396).
The best-known mechanisms are those that involve the antioxidant nutrients (vitamins C and E, glutathione) and enzymes such as the superoxide dismutases, which require copper, manganese or selenium as cofactor (Maggini et al. 2007). These are just a few of the many mechanisms that essentially “heal” cells damaged by ROS.
A pluralistic health-care environment provides individuals (and those caring for them) with therapeutic options (with regard to diagnoses that ‘make sense,’ reduce stigma or accomplish social goals, as well as with treatment options), a sense of agency in the therapeutic process and opportunities for holding out hope (Frank 1973; Good et al. 1990; Nichter and Quintero 1996). Through the proliferation of pluralistic medicine, opportunities for catalyzing a placebo response by triggers to the mind, body and senses are multiplied. Further, in the current Western context, patients are choosing to use multiple health-care systems interactively.
Although placebos and placebo arms are tools at the foundation of clinical research, a number of prominent scholars of this topic have noted that the placebo effect has been treated as a “nuisance factor”—that is, something to be controlled, minimized or, at the very least, tolerated—in clinical research (Ader 2000; Benedetti 2008; Enck et al. 2008; Kaptchuk 2002; Walach and Jonas 2004).
Whole-systems research (WSR) aims to investigate the efficacy of complex health-care systems (such as homeopathy, naturopathy or traditional Chinese medicine and, ultimately, biomedicine) in a way that is consistent with their philosophical underpinnings and real-world practice (including diagnosis, therapeutic intervention and outcome assessment). WSR looks beyond the specific efficacy of an intervention to consider the contribution of indirect (‘placebo’) effects and larger ‘whole-person’ shifts on overall well-being. A key issue central to carrying out WSR is the need for research designs that are tailored to best understanding the intact system (Ritenbaugh et al. 2003; Verhoef et al. 2005).
We acknowledge that the term ‘placebo’ has specific utility in pharmaceutical trials, in order to establish the safety and specific efficacy of pharmaceutical therapies. There, the term plays a functional design role, helping to account for other sources of variance in outcome, including the natural course of the disease and random variation. While we concede that the term placebo continue to be used within this narrow focus, we reiterate the call for further research and critique into the problematic nature of placebo-controlled clinical trials (see Shah 2006). One informant in India told M.N., when he asked whether she was concerned that the medication she received in a clinical trial would not work (was a placebo), “Of course it works! It must work! No one would spend this kind of money [to outfit and run the clinic housing the study] if it didn’t work!”
For example, Fabrega (1997b) argues that the earliest forms of sickness (that is, “the behavioral expressions of disease and injury” [p. ix]), emerging in family-level foragers, were short-term and generally acute; healing was fairly unelaborated, as sick persons were self-treated or treated by family members, with the goal being a quick return to productivity or death. In contrast to the contemporary industry of sickness and healing, Fabrega (1997a) stresses that evolutionarily early healing “did not prolong dependence or sickness, nor could it be said to have caused conditions of sickness and dependence” (p. 43).
References
Ader, Robert 1997 The Role of Conditioning in Pharmacotherapy. In The Placebo Effect: An Interdisciplinary Exploration. Anne Harrington, ed. Cambridge, MA: Harvard University Press.
Ader, Robert (2000)The Placebo Effect: If It’s All in Your Head, Does That Mean You Only Think You Feel Better? Advances in Mind-Body Medicine 16(1):7.
Adler, Jerry 2007 A Big Dose of Skepticism: Those ‘Amazing New Treatments’ Usually Aren’t So Amazing. In Newsweek. Available at: http://www.newsweek.com/id/73283. Accessed December 6, 2007.
Atkinson, Jane Monnig 1987 The Effectiveness of Shamans in an Indonesian Ritual. American Anthropologist 342–355.
auf dem Keller, Ulrich, Angelika Kumin, Susanne Braun, and Sabine Werner 2006 Reactive Oxygen Species and Their Detoxification in Healing Skin Wounds. Journal of Investigative Dermatology Symposium Proceedings 11(1): 106–111.
Austin, J. L. 1962 How to Do Things with Words. Cambridge, MA: Harvard University Press.
Bandura, Albert 1997 Self-Efficacy: The Exercise of Control. New York: Cambridge University Press.
Barker, David J. P. 1998 Mothers, Babies and Health in Later Life. Edinburgh: Churchill Livingstone.
Barsky, Arthur J., Ralph Saintfort, Malcolm P. Rogers, and Jonathan F. Borus 2002 Nonspecific Medication Side Effects and the Nocebo Phenomenon. Journal of the American Medical Association 287(5):622–627.
Barton, Gregory M. (2008) A Calculated Response: Control of Inflammation by the Innate Immune System. Journal of Clinical Investigation 118(2):413–420.
Basso, Keith H. (1996) Wisdom Sits in Places: Landscape and Language among the Western Apache. Albuquerque: University of New Mexico Press.
Bateson, Gregory (1975)“Reality” and Redundancy. The Co-Evolution Quarterly 6:132–135.
Bausell, R. Barker 1990 On the Formal Induction of the Press into the Scientific Process. Evaluation & the Health Professions 13(3):267–282.
Bausell, R. Barker 2007 Snake Oil Science: The Truth about Complementary and Alternative Medicine. New York: Oxford University Press.
BBC 2002 Homeopathy: The Test. In Horizons. Available at: http://www.bbc.co.uk/science/horizon/2002/homeopathy.shtml.
Beecher, Henry K. (1955) The Powerful Placebo. Journal of the American Medical Association 159(17):1602–1606.
Bell, Iris R., Daniel A. Lewis, 2nd, Audrey J. Brooks, Gary E. Schwartz, Sabrina E. Lewis, Opher Caspi, Victoria Cunningham, and Carol M. Baldwin 2004 Individual Differences in Response to Randomly Assigned Active Individualized Homeopathic and Placebo Treatment in Fibromyalgia: Implications of a Double-Blinded Optional Crossover Design. Journal of Alternative and Complementary Medicine 10(2):269–283.
Benedetti, F.(2008)Mechanisms of Placebo and Placebo-Related Effects across Diseases and Treatments. Annual Review of Pharmacology and Toxicology 48:33–60.
Benedetti, Fabrizio, Helen S. Mayberg, Tor D. Wager, Christian S. Stohler, Jon-Kar Zubieta (2005) Neurobiological Mechanisms of the Placebo Effect. Journal of Neuroscience 25(45):10390–10402.
Benedetti Fabrizio, M. Lanotte, L. Lopiano, L. Colloca (2007) When Words Are Painful: Unraveling the Mechanisms of the Nocebo Effect. Neuroscience 147(2):260.
Ben-Shlomo Yoav, Diana Kuh (2002) A Lifecourse Approach to Chronic Disease Epidemiology: Conceptual Models, Empirical Challenges and Interdisciplinary Perspectives. International Journal of Epidemiology 31:285–293.
Benson Herbert, Richard Friedman (1996) Harnessing the Power of the Placebo Effect and Renaming It ‘‘Remembered Wellness’’ Annual Review of Medicine 47:193–199.
Berkman, Lisa F., and Ichiro Kawachi 2000 A Historical Framework for Social Epidemiology. In Social Epidemiology. Lisa F. Berkman and Ichiro Kawachi, eds., Chap. 1. Oxford: Oxford University Press.
Beyerstein, B. L. (2001) Alternative Medicine and Common Errors of Reasoning. Academic Medicine 76(3):230–237.
Birch Stephen (2006) A Review and Analysis of Placebo Treatments, Placebo Effects, and Placebo Controls in Trials of Medical Procedures When Sham Is Not Inert. Journal of Alternative and Complementary Medicine 12(3):303–310.
Bootzin Richard R, Elaine T. Bailey (2005)Understand Placebo, Nocebo, and Iatrogenic Treatment Effects. Journal of Clinical Psychology 61(7):871–880.
Bootzin, Richard R, Opher Caspi (2002) Explanatory Mechanisms for Placebo Effects: Cognition, Personality and Social Learning. In: The Science of Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, Arthur Kleinman, John W. Kusek, and Linda W. Engel, eds. Pp. 108–132. London: BMJ Books.
Bourdieu Pierre (1977)Outline of a Theory of Practice. Cambridge: Cambridge University Press.
Briggs Charles L. (1994) The Sting of the Ray: Bodies, Agency, and Grammar in Warao Curing. Journal of American Folklore 107(423):139–166.
Brody Howard (1997)The Doctor as Therapeutic Agent. In The Placebo Effect: An Interdisciplinary Exploration. Anne Harrington, ed. Pp. 77–92. Cambridge, MA: Harvard University Press.
Brody Howard (2000) The Placebo Response—Recent Research and Implications for Family Medicine. Journal of Family Practice 49(7):649–654.
Brody Howard, David B. Waters (1980) Diagnosis Is Treatment. Journal of Family Practice 10(3):445–449.
Brody Howard, Cardinal J. L., Foglio J. P (2004) Addressing Spiritual Concerns in Family Medicine: A Team Approach. Journal of the American Board of Family Practice 17(3):201–206.
Brown, Nik (2003) Hope against Hype—Accountability in Biopasts, Presents and Futures. Science Studies 16(2):3–21.
Butler Judith (1990) Gender Trouble: Feminism and the Subversion of Identity. New York: Routledge.
Cartwright Elizabeth (2007) Bodily Remembering: Memory, Place, and Understanding Latino Folk Illnesses among the Amuzgos Indians of Oaxaca, Mexico. Culture, Medicine and Psychiatry 31:527–545.
Casey Edward S. (1987) Body Memory. In Remembering: A Phenomenological Study. Pp. 146–165. Bloomington: Indiana University Press.
Caspi, Opher 2002 When Are Medication Side Effects Due to the Nocebo Phenomenon? Journal of the American Medical Association 287(19):2502.
Caspi, Opher 2003 Activating the Healing Response. In Integrative Medicine. David Rakel, ed., pp. 703–710. Philadelphia: Saunders.
Caspi O., Bootzin R. R.(2002) Evaluating How Placebos Produce Change—Logical and Causal Traps and Understanding Cognitive Explanatory Mechanisms. Evaluation & The Health Professions 25(4):436–464.
Caspi, Opher, and Iris R. Bell 2004a One Size Does Not Fit All: Aptitude Chi Treatment Interaction (ATI) as a Conceptual Framework for Complementary and Alternative Medicine Outcome Research. Part II. Research Designs and Their Applications. Journal of Alternative and Complementary Medicine 10(4): 698–705.
Caspi, Opher, and Iris R. Bell 2004b One Size Does Not Fit All: Aptitude × Treatment Interaction (ATI) as a Conceptual Framework for Complementary and Alternative Medicine Outcome Research. Part I. What Is ATI Research? Journal of Alternative and Complementary Medicine 10(3): 580–586.
Christian Lisa M., Jennifer E. Graham, David A. Padgett, Ronald Glaser, Janice K. Kiecolt-Glaser (2006) Stress and Wound Healing. Neuroimmunomodulation 13(5–6):337–346.
CNN 2004 Power of the Placebo: Simply Expecting Relief from Pain Can Help, Study Shows. Available at www.CNN.com. Accessed December 7, 2007.
Csordas Thomas J. (1990) Embodiment as a Paradigm for Anthropology. Ethos 18(1):5–47.
Csordas Thomas J 1993 Somatic Modes of Attention. Cultural Anthropology 8(2):135–156.
Damjanovic Amanda K., Yinhua Yang, Ronald Glaser, Janice K. Kiecolt-Glaser, Huy Nguyen, Bryon Laskowski, Yixiao Zou, David Q. Beversdorf, Nan-ping Weng (2007) Accelerated Telomere Erosion Is Associated with a Declining Immune Function of Caregivers of Alzheimer’s Disease Patients. Journal of Immunology 179(6):4249–4254.
Denis M. (1985) Visual Imagery and the Use of Mental Practice in the Development of Motor Skills. Canadian Journal of Applied Sport Sciences 10(4):4S–16S.
Detillion C. E., Craft T. K., Glasper E. R., Prendergast B. J., DeVries A. C. (2004) Social Facilitation of Wound Healing. Psychoneuroendocrinology 29(8):1004– 1011.
DeVries A. C., Glasper E. R., Detillion C. E (2003) Social Modulation of Stress Responses. Physiology & Behavior 79(3):399–407.
de Vries S., Mulder T (2007) Motor Imagery and Stroke Rehabilitation: A Critical Discussion. Journal of Rehabilitation Medicine 39(1):5–13.
Dijkstra K., Pieterse M., Pruyn A (2006) Physical Environmental Stimuli That Turn Healthcare Facilities into Healing Environments through Psychologically Mediated Effects: Systematic Review. Journal of Advancd Nursing 56(2):166–181.
Dimitriou R., Tsiridis E., Giannoudis P. V.(2005) Current Concepts of Molecular Aspects of Bone Healing. Injury 36(12):1392– 1404.
Dreyfus Herbert L. 1999 The Primacy of Phenomenology over Logical Analysis. Philosophical Topics 27:3–24.
Eaton S. B., Konner M, Shostak M (1988) Stone Agers in the Fast Lane: Chronic Degenerative Diseases in Evolutionary Perspective. American Journal of Medicine 84:739–749.
Enck P., Benedetti F., Schedlowski M.(2008) New Insights into the Placebo and Nocebo Responses. Neuron 59(2):195–206.
Fabrega, Horacio 1997a Earliest Phases in the Evolution of Sickness and Healing. Medical Anthropology Quarterly 11(1): 26–55.
Fabrega, Horacio 1997b Evolution of Sickness and Healing. Berkeley: University of California Press.
Fietta P. (2007) Life-or-Death Fate in the Adaptive Immune System. Rivista di Biologia 100(2):267–283.
Fonnebo Vinjar, Sameline Grimsgaard, Harald Walach, Cheryl Ritenbaugh, Arne Norheim, Hugh MacPherson, George Lewith, Laila Launso, Mary Koithan, Torkel Falkenberg, Heather Boon, Mikel Aickin (2007) Researching Complementary and Alternative Treatments—The Gatekeepers Are Not at Home. BMC Medical Research Methodology 7(1):7.
Frank J. D. (1973) Persuasion and Healing: A Comparative Study of Psychotherapy. Baltimore: Johns Hopkins University Press.
Freed C. R., Greene P. E., Breeze R. E., Tsai W. Y., DuMouchel W., Kao R., Dillon S., Winfield H., Culver S., Trojanowski J. Q., Eidelberg D., Fahn S. (2001) Transplantation of Embryonic Dopamine Neurons for Severe Parkinson’s Disease. New England Journal of Medicine 344(10):710–719.
Frenkel Oron (2008) A Phenomenology of the ‘Placebo Effect’: Taking Meaning from the Mind to the Body. Journal of Medicine and Philosophy 33(1):58–79.
Geers A. L., Helfer S. G., Weiland P. E, Kosbab K. (2006) Expectations and Placebo Response: A Laboratory Investigation into the Role of Somatic Focus. Journal of Behavioral Medicine 29(2):171–178.
Giang D. W., Goodman A. D, Schiffer R. B, Mattson D. H, Petrie M., Cohen N., Ader R. (1996) Conditioning of Cyclophosphamide-Induced Leukopenia in Humans. Journal of Neuropsychiatry and Clinical Neurosciences 8(2):194–201.
Girardi M. (2007) Cutaneous Perspectives on Adaptive Immunity. Clinical Reviews in Allergy Immunology 33(1–2):4–14.
Godbout J. P., Glaser R. (2006) Stress-Induced Immune Dysregulation: Implications for Wound Healing, Infectious Disease and Cancer. Journal of Neuroimmune Pharmacology 1(4):421– 427.
Goebel M. U., Trebst A. E., Steiner J., Xie Y. F., Exton M. S., Frede S., Canbay A. E., Michel M. C., Heemann U., Schedlowski M. (2002) Behavioral Conditioning of Immunosuppression Is Possible in Humans. FASEB Journal 16(14):1869–1873.
Goffman Erving (1959) The Presentation of Self in Everyday Life. New York: Anchor Books.
Good M. J. D., Good B. J., Schaffer C., Lind S. E. (1990) American Oncology and the Discourse on Hope. Culture Medicine and Psychiatry 14(1):59–79.
Haglund M. E., Nestadt P. S, Cooper N. S, Southwick S. M., Charney D. S. (2007) Psychobiological Mechanisms of Resilience: Relevance to Prevention and Treatment of Stress-Related Psychopathology. Developmental Psychopathology 19(3):889–920.
Hahn Robert 1999 Expectations of Sickness: Concept and Evidence of the Nocebo Phenomenon. In How Expectancies Shape Experience. I. Kirsch, ed. Pp. 333–356. Washington, DC: American Psychological Association.
Harrell S. (1991) Pluralism Performance and Meaning in Taiwanese Healing: A Case Study. Culture Medicine and Psychiatry 15(1):45–68.
Harrington Anne (2002) “Seeing” the Placebo Effect: Historical Legacies and Present Opportunities. In The Science of the Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, Arthur Kleinman, John W. Kusek, and Linda W. Engel, eds. Pp. 35–52. London: BMJ Books.
Helman Cecil G. (2001) Placebos and Nocebos: The Cultural Construction of Belief. In Understanding the Placebo Effect in Complementary Medicine: Theory, Practice and Research. David Peters, ed. Pp. 3–16. Edinburgh: Churchill Livingstone.
Hertzman C. (1999) The Biological Embedding of Early Experience and Its Effects on Health in Adulthood. Annals of the New York Academy of Science 896:85–95.
Hinton Devon, Khin Um, Phalnarith Ba (2001) A Unique Panic-Disorder Presentation among Khmer Refugees: The Sore-Neck Syndrome. Culture Medicine and Psychiatry 25(3):297.
Hinton Devon E., Chhean D., Pich V., Hofmann S. G., Barlow D. H. (2006) Tinnitus among Cambodian Refugees: Relationship to PTSD Severity. Journal of Traumatic Stress 19(4):541–546.
Hrobjartsson A., Gotzsche P. C (2001) Is the Placebo Powerless? An Analysis of Clinical Trials Comparing Placebo with No Treatment. New England Journal of Medicine 344(21):1594–1602.
Hrobjartsson A., Gotzsche P. C 2004 Is the Placebo Powerless? Update of a Systematic Review with 52 New Randomized Trials Comparing Placebo with No Treatment. Journal of Internal Medicine 256(2):91–100.
Illich, Ivan 1975 Medical Nemesis: The Exploration of Health. London: Calder & Boyars.
IOM 2005a Complementary and Alternative Medicine (CAM) in the United States. Washington DC: National Academies Press.
IOM 2005b Institute of Medicine Report on Complementary and Alternative Medicine in the United States. Seminars in Integrative Medicine 3(1): 4.
Irwin M. R., Miller A. H. (2007) Depressive Disorders and Immunity: 20 Years of Progress and Discovery. Brain Behavior and Immunity 21(4):374–383.
Johnson, Carla K. 2007a Acupuncture, Real or Sham, Works Better Than Standard Care for Low Back Pain. Associated Press Online, September 24, 2007. Available at: http://www.ap.org.
Johnson, Carla K. 2007b Researchers: Even Fake Acupuncture Works. Associated Press Online, September 24, 2007. Available at: http://www.ap.org.
Kaptchuk T. J. (1998) Powerful Placebo: The Dark Side of the Randomised Controlled Trial. Lancet 351(9117):1722–1725.
Kaptchuk T. J (2002) The Placebo Effect in Alternative Medicine: Can the Performance of a Healing Ritual Have Clinical Significance? Annals of Internal Medicine 136(11):817–825.
Kastelein, John J.P., Fatima Akdim, Erik S.G. Stroes, Aeilko H. Zwinderman, Michiel L. Bots, Anton F.H. Stalenhoef, Frank L.J. Visseren, Eric J.G. Sijbrands, Mieke D. Trip, Evan A. Stein, Daniel Gaudet, Raphael Duivenvoorden, Enrico P. Veltri, A. David Marais, Eric de Groot, and the ENHANCE Investigators 2008 Simvastatin With or Without Ezetimibe in Familial Hypercholesterolemia. New England Journal of Medicine 358(14): 1431–1443.
Kemeny M. E., Schedlowski M. (2007) Understanding the Interaction between Psychosocial Stress and Immune-Related Diseases: A Stepwise Progression. Brain Behavior and Immunology 21(8):1009–1018.
Kihlstrom John F. (1987) The Cognitive Unconscious. Science 237:1445–1452.
Kihlstrom John F (1996) Perception without Awareness of What Is Perceived, Learning without Awareness of What Is Learned. In The Science of Consciousness: Psychological, Neuropsychological, and Clinical Reviews. M. Velmans, ed. Pp. 23–46. London: Routledge.
Kirmayer Laurence (2003) Reflections on Embodiment. In Social and Cultural Lives of Immune Systems. James M. Wilce, Jr., ed. Pp. 282–302. London: Routledge.
Kirsch Irving (1997) Specifying Nonspecifics: Psychological Mechanisms of Placebo Effects. In The Placebo Effect: An Interdisciplinary Exploration. Anne Harrington, ed. Pp. 166– 186. Cambridge, MA: Harvard University Press.
Kirsch Irving 2002 Yes, There Is a Placebo Effect, but Is There a Powerful Antidepressant Drug Effect? Prevention & Treatment 5(22).
Kirsch Irving, Guy Sapirstein (1998) Listening to Prozac but Hearing Placebo: A Meta-analysis of Antidepressant Medication. Prevention & Treatment 1:2a.
Kirsch Irving, Deacon B. J., Huedo-Medina T. B., Scoboria A., Moore T. J., Johnson B. T (2008) Initial Severity and Antidepressant Benefits: A Meta-analysis of Data Submitted to the Food and Drug Administration. PLoS Med 5(2):e45.
Kleinman Arthur, Harry A. Guess, Joan S. Wilentz (2002) An Overview. In The Science of the Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, Arthur Kleinman, John W. Kusek, and Linda W. Engel, eds. Pp. 1–32. London: BMJ Books.
Krieger, Nancy (2000) Discrimination and Health. Oxford: Oxford University Press.
Krieger Nancy (2001) Theories for Social Epidemiology in the 21st Century: An Ecosocial Perspective. International Journal of Epidemiology 30:668–677.
Krieger Nancy (2003) Does Racism Harm Health? Did Child Abuse Exist Before 1962? On Explicit Questions, Critical Science, and Current Controversies: An Ecosocial Perspective. American Journal of Public Health 93(2):194–199.
Krieger Nancy (2005) Embodiment: A Conceptual Glossary for Epidemiology. Journal of Epidemiology and Community Health 59(5):350–355.
Krieger Nancy, Smith G. D. (2004) “Bodies Count,” and Body Counts: Social Epidemiology and Embodying Inequality. Epidemiologic Reviews 26:92–103.
Krogman W. M. (1951) The Scars of Human Evolution. Scientific American 185:54–57.
Kuh D., Yoav Ben-Shlomo, Lynch J., Hallqvist J., Power C.(2003) Life Course Epidemiology. Journal of Epidemiology and Community Health 57:778–783.
Laderman Carol (1987) The Ambiguity of Symbols in the Structure of Healing. Social Science Medicine 24(4):293–301.
Lakoff Andrew (2007) The Right Patients for the Drug: Managing the Placebo Effect in Antidepressant Trials. BioSocieties 2:57–71.
Lampe J. W., Chang J. L (2007) Interindividual Differences in Phytochemical Metabolism and Disposition. Seminars in Cancer Biology 17(5):347–353.
Lasker G. W. (1969) Human Biological Adaptability. The Ecological Approach in Physical Anthropology. Science 166(3912):1480–1486.
Lehman, Betsy 1990 Two Studies Raise Doubts on Oats Fad. The Boston Globe, January 18, p. 1.
Libby P. (2007) Inflammatory Mechanisms: The Molecular Basis of Inflammation and Disease. Nutrition Reviews 65(12; Pt 2):S140–S146.
Livingstone F. (1958) Anthropological Implications of Sickle Cell Gene Distribution in West Africa. American Anthropologist 60:533–562.
Lock, Margaret 1993a Cultivating the Body—Anthropology and Epistemologies of Bodily Practice and Knowledge. Annual Review of Anthropology 22: 133–155.
Lock, Margaret 1993b Encounters with Aging: Mythologies of Menopause in Japan and North America. Berkeley: University of California Press.
Low Setha M. (2003) Embodied Space(s): Anthropological Theories of Body, Space, and Culture. Space and Culture 6(1):9–18.
Lundh L. G. (1987) Placebo, Belief, and Health. A Cognitive-Emotional Model. Scandinavian Journal of Psychology 28(2):128–143.
Maggini S., Wintergerst E. S, Beveridge S., Hornig D. H (2007) Selected Vitamins and Trace Elements Support Immune Function by Strengthening Epithelial Barriers and Cellular and Humoral Immune Responses. British Journal of Nutrition 98 (Suppl 1):S29–S35.
Mahoney M. C. (2007) Genetic Polymorphisms and Disease Prevention. Pediatric Blood Cancer 48(7):742–747.
Malenbaum Sara, Francis J. Keefe, Amanda C. de C. Williams, Roger Ulrich, Tamara J. Somers (2008) Pain in Its Environmental Context: Implications for Designing Environments to Enhance Pain Control. Pain 134(3):241.
Mayor Susan (2008) Study Shows Difference between Antidepressants and Placebo Is Significant Only in Severe Depression. British Medical Journal 336:466.
McKinlay J. B., Marceau L. D (2000) Public Health Matters: To Boldly Go. American Journal of Public Health 89(3):295–298.
McLaren L., Hawe P. (2005) Ecological Perspectives in Health Research. Journal of Epidemiology and Community Health 59(1):6–14.
McRae C., Cherin E., Yamazaki T. G, Diem G., Vo A. H., Russell D., Ellgring J. H., Fahn S., Greene P., Dillon S., Winfield H., Bjugstad K. B., Freed C. R (2004) Effects of Perceived Treatment on Quality of Life and Medical Outcomes in a Double-Blind Placebo Surgery Trial. Archives of General Psychiatry 61(4):412– 420.
Medzhitov R. (2007) Recognition of Microorganisms and Activation of the Immune Response. Nature 449(7164):819–826.
Mendoza DW, Wichman H (1978) ‘Inner’ Darts: Effects of Mental Practice on Performance of Dart Throwing. Perceptual & Motor Skills 47:1195–1199.
Merleau-Ponty M. (1962) Phenomenology of Perception. London: Routledge & Kegan Paul.
Merleau-Ponty M. (1964) The Primacy of Perception. Boston: Northwestern University Press.
Mills P. J., Adler K. A., Dimsdale J. E, Perez C. J, Ziegler M. G, Ancoli-Israel S., Patterson T. L, Grant I. (2004) Vulnerable Caregivers of Alzheimer Disease Patients Have a Deficit in Beta 2-Adrenergic Receptor Sensitivity and Density. American Journal of Geriatric Psychiatry 12(3):281–286.
Moerman, Daniel E. 2002a Meaning, Medicine, and the ‘Placebo Effect.’ New York: Cambridge University Press.
Moerman, Daniel E. 2002b Explanatory Mechanisms for Placebo Effects: Cultural Influences and Meaning Responses. In The Science of the Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, A. Kleinman, John W. Kusek, and Linda W. Engel, eds., pp. 77–107. London: BMJ Books.
Montgomery S. A. (1999) The Failure of Placebo-Controlled Studies. European Neuropsychopharmacology 9(3):271–276.
Moseley J. B., O’Malley K., Petersen N. J., Menke T. J, Brody B. A., Kuykendall D. H., Hollingsworth J. C., Ashton C. M., Wray N. P. (2002) A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee. New England Journal of Medicine 347(2):81–88.
Munte Thomas F., Eckart Altenmuller, Lutz Jancke (2002) The Musician’s Brain as a Model of Neuroplasticity. Nature Reviews. Neuroscience 3:473–478.
Murphy, Kenneth 2007 Janeway’s Immunobiology. 7th ed. New York: Garland Science.
Netea, M. G., G. D. Brown, B. J. Kullberg, and N. A. Gow 2008 An Integrated Model of the Recognition of Candida albicans by the Innate Immune System. Nature Reviews Microbiology 6(1):67–78.
Newton, K. M., S. D. Reed, A. Z. LaCroix, L. C. Grothaus, K. Ehrlich, and J. Guiltinan 2006 Treatment of Vasomotor Symptoms of Menopause with Black Cohosh, Multibotanicals, Soy, Hormone Therapy, or Placebo: A Randomized Trial. Annals of Internal Medicine 145(12):869–879.
Nichter, Mark 1981a Idioms of Distress: Alternatives in the Expression of Psychosocial Distress: A Case Study from South India. Culture, Medicine and Psychiatry 5: 379–408.
Nichter, Mark 1981b Negotiation of the Illness Experience: Ayurvedic Therapy and the Psychosocial Dimension of Illness. Culture, Medicine and Psychiatry 5: 5–24.
Nichter, Mark 2008 Coming to Our Senses: Appreciating the Sensorial in Medical Anthropology. Transcultural Psychiatry 45(2):163–197.
Nichter, Mark, and Carol Nordstrom 1989 A Question of Medicine Answering—Health Commodification and the Social-Relations of Healing in Sri-Lanka. Culture Medicine and Psychiatry 13(4):367–390.
Nichter, Mark, and Gilbert Quintero 1996 Pluralistic Therapy Systems: Why Do They Co-exist and How Are They Used? In Encyclopedia of Cultural Anthropology. D. Levinson and M. Ember, eds. Pp. 1– 17. New York: Henry Holt.
Nichter, Mark, and Jennifer Jo Thompson 2006 For My Wellness, Not Just My Illness: North Americans’ Use of Dietary Supplements. Culture, Medicine and Psychiatry 30(2):175–222.
Nordstrom, Carol 1998 Terror Warfare and the Medicine of Peace. Medical Anthropology Quarterly 12(1):103–121.
Novack, D. H., O. Cameron, E. Epel, R. Ader, S. R. Waldstein, S. Levenstein, M. H. Antoni, and A. R. Wainer 2007 Psychosomatic Medicine: The Scientific Foundation of the Biopsychosocial Model. Academy of Psychiatry 31(5):388–401.
Nuckolls, Charles W. 1992 Deciding How to Decide: Possession-Mediumship in Jalari Divination. In Anthropological Approaches to the Study of Ethnomedicine. Mark Nichter, ed. Pp. 75–100. Philadelphia: Gordon and Breach Science.
Obeyesekere, Gananath 1990 The Work of Culture. Chicago: University of Chicago Press.
Ots, Thomas 1991 Phenomenology of the Body: The Subject-Object Problem in Psychosomatic Medicine and the Role of Traditional Medical Systems Herein. Anthropologies of Medicine 7:43–58.
Pascual-Leone, Alvaro 2001 The Brain That Plays Music and Is Changed by It. Annals of the New York Academy of Sciences 930:315–329.
Pike, Ivy L. 2001 The Evolutionary and Ecological Context of Human Pregnancy. In Reproductive Ecology and Human Evolution. Peter T. Ellison, ed. Pp. 39–58. New York: Aldine de Gruyter.
Pollo, A., M. Amanzio, A. Arslanian, C. Casadio, G. Maggi, and F. Benedetti 2001 Response Expectancies in Placebo Analgesia and Their Clinical Relevance. Pain 93(1):77–84.
Price, Donald, and Lene Vase Sorensen 2002 Endogenous Opioid and Non-opioid Pathways as Mediators of Placebo Analgesia. In The Science of the Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, Arthur Kleinman, John W. Kusek, and Linda W. Engel, eds. Pp. 183–206. London: BMJ Books.
Price, Donald D., Damien G. Finniss, and Fabrizio Benedetti 2008 A Comprehensive Review of the Placebo Effect: Recent Advances and Current Thought. Annual Review of Psychology 59:21–226.
Pulvermuller, F. 2001 Brain Reflections of Words and Their Meaning. Trends in Cognitive Sciences 5(12):517–524.
RadioLab 2007 Memory and Forgetting. Available at: http://www.wnyc.org/shows/radiolab/episodes/2007/06/08.
Richardson, M. 1982 Being-in-the-Plaza versus Being-in-the-Market: Material Culture and the Construction of Social Reality. American Ethnologist 9:421–436.
Ritenbaugh, Cheryl 1999 Evolutionary Perspectives on Diet and Cancer. Anthropology and Medicine 6(3):323–336.
Ritenbaugh, Cheryl, M. Verhoef, S. Fleishman, H. Boon, and A. Leis 2003 Whole Systems Research: A Discipline for Studying Complementary and Alternative Medicine. Alternative Therapies in Health and Medicine 9(4):32–36.
Rizzolatti, G., and L. Craighero 2004 The Mirror-Neuron System. Annual Review of Neuroscience 27:169–192.
Rizzolatti, G., L. Fogassi, and V. Gallese 2006 Mirrors of the Mind. Scientific American 295(5):54–61.
Sacks, Oliver 2007a The Abyss: Music and Amnesia. The New Yorker, September 24. Available at: http://www.newyorker.com/reporting/2007/09/24/070924fa_fact_sacks. Accessed January 29, 2008.
Sacks, Oliver 2007b Musicophilia: Tales of Music and the Brain. New York: Knopf.
Sancar, A., L. A. Lindsey-Boltz, K. Unsal-Kacmaz, and S. Linn 2004 Molecular Mechanisms of Mammalian DNA Repair and the DNA Damage Checkpoints. Annual Review of Biochemistry 73:39–85.
Schafer, M., and S. Werner 2007 Transcriptional Control of Wound Repair. Annual Review of Cell and Developmental Biology 23:69–92.
Scheper-Hughes, Nancy, and Margaret Lock 1987 The Mindful Body: A Prolegomenon to Future Work in Medical Anthropology. Medical Anthropology Quarterly 1(1):6–41.
Schlaug, G. 2001 The Brain of Musicians. A Model for Functional and Structural Adaptation. Annals of the New York Academy of Sciences 930:281–299.
Schonberg, H 1987 Great Pianists. St. Louis, MO: Fireside Books.
Schonberg, H 1988 The Virtuosi. New York: Vintage-Random House.
Schweitzer, Marc, Laura Gilpin, and Susan Frampton 2004 Healing Spaces: Elements of Environmental Design That Make an Impact on Health. Journal of Alternative & Complementary Medicine 10:S-71.
Shah, Sonia 2006 The Body Hunters: Testing New Drugs on the World’s Poorest Patients. New York: New Press.
Shang, A., K. Huwiler-Muntener, L. Nartey, P. Juni, S. Dorig, J. A. Sterne, D. Pewsner, and M. Egger 2005 Are the Clinical Effects of Homoeopathy Placebo Effects? Comparative Study of Placebo-Controlled Trials of Homoeopathy and Allopathy. Lancet 366(9487):726–732.
Shilo, S., S. Roy, S. Khanna, and C. K. Sen 2007 MicroRNA in Cutaneous Wound Healing: A New Paradigm. DNA and Cell Biology 26(4):227–237.
Siegel, Shepard 2002 Explanatory Mechanisms for Placebo Effects: Pavlovian Conditioning. In The Science of the Placebo: Toward an Interdisciplinary Research Agenda. Harry A. Guess, Arthur Kleinman, John W. Kusek, and Linda W. Engel, eds. Pp. 133–157. London: BMJ Books.
Smith, D., and P. Holmes 2004 The Effect of Imagery Modality on Golf Putting Performance. Journal of Sport & Exercise Psychology 26(3):385–395.
Southwick, S. M., M. Vythilingam, and D. S. Charney 2005 The Psychobiology of Depression and Resilience to Stress: Implications for Prevention and Treatment. Annual Review of Clinical Psychology 1:255–291.
Swain, J. F., I. L. Rouse, C. B. Curley, and F. M. Sacks 1990 Comparison of the Effects of Oat Bran and Low-Fiber Wheat on Serum Lipoprotein Levels and Blood Pressure. New England Journal of Medicine 322(3):147–152.
Taber, K. H., M. Redden, and R. A. Hurley 2007 Functional Anatomy of Humor: Positive Affect and Chronic Mental Illness. Journal of Neuropsychiatry and Clinical Neurosciences 19(4):358–362.
Tambiah, S. J. 1979 A Performative Approach to Ritual. Vol. LXV. London: Oxford University Press.
Thompson, Jennifer Jo, and Mark Nichter 2007 The Compliance Paradox: What We Need to Know about “Real World” Dietary Supplement Use in the United States. Alternative Therapies in Health and Medicine 13(2):48–55.
Thorpe, G. W., C. S. Fong, N. Alic, V. J. Higgins, and I. W. Dawes 2004 Cells Have Distinct Mechanisms to Maintain Protection against Different Reactive Oxygen Species: Oxidative-Stress-Response Genes. Proceedings of the National Academy of Sciences of the United States of America 101(17):6564– 6569.
Throop, C. Jason 2003 On Crafting a Cultural Mind: A Comparative Assessment of Some Recent Theories of `Internalization’ in Psychological Anthropology. Transcultural Psychiatry 40(1):109–139.
Trevathan, Wenda R. 2007 Evolutionary Medicine. Annual Review of Anthropology 36:139–154.
Trevathan, Wenda, Euclid O. Smith, and James McKenna 2008 Evolutionary Medicine and Health: New Perspectives. New York: Oxford University Press.
Ulrich, R. S. 1984 View through a Window May Influence Recovery from Surgery. Science 224(4647):420–421.
Vase, L., M. E. Robinson, G. N. Verne, and D. D. Price 2003 The Contributions of Suggestion, Desire, and Expectation to Placebo Effects in Irritable Bowel Syndrome Patients—An Empirical Investigation. Pain 105(1–2):17–25.
Vedantam, Shankar 2002 Against Depression, a Sugar Pill Is Hard to Beat; Placebos Improve Mood, Change Brain Chemistry in Majority of Trials of Antidepressants. The Washington Post, May 7, p. A01.
Verhoef, M. J., G. Lewith, C. Ritenbaugh, H. Boon, S. Fleishman, and A. Leis 2005 Complementary and Alternative Medicine Whole Systems Research: Beyond Identification of Inadequacies of the RCT. Complementary Therapies in Medicine 13(3):206–212.
Waber, Rebecca L., Baba Shiv, Ziv Carmon, and Dan Ariely 2008 Commercial Features of Placebo and Therapeutic Efficacy. Journal of the American Medical Association 299(9):1016–1017.
Walach, H., and W. B. Jonas 2004 Placebo Research: The Evidence Base for Harnessing Self-Healing Capacities. Journal of Alternative & Complementary Medicine 10 (Suppl 1):S103–S112.
Walach, Harald, Wayne B. Jonas, and George Lewith 2002 The Role of Outcomes Research in Evaluating Complementary and Alternative Medicine. In Clinical Research in Complementary Therapies. H. Walach, W. B. Jonas, and G. Lewith, eds. Pp. 29–45. Edinburgh: Churchill Livingstone.
Walach, Harald, Wayne B. Jonas, and George Lewith 2005 Are the Clinical Effects of Homoeopathy Placebo Effects? Lancet 366(9503): 2081; author reply 2083–2086.
Washburn, S. 1951 The New Physical Anthropology. New York Academy of Sciences, Series III 13:298–304.
Wearing, Deborah 2005 Forever Today. New York: Doubleday.
Williams, George C., and Randolph M. Nesse 1991 The Dawn of Darwinian Medicine. Quarterly Review of Biology 66(1):1–22.
Yavuzer, G., R. Selles, N. Sezer, S. Sutbeyaz, J. B. Bussmann, F. Koseoglu, M. B. Atay, and H. J. Stam 2008 Mirror Therapy Improves Hand Function in Subacute Stroke: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation 89(3):393– 398.
Yi, B., J. Y. Yang, and M. Yang 2007 Past and Future Applications of CYP450-Genetic Polymorphisms for Biomonitoring of Environmental Toxicants. Journal of Environmental Science and Health Part C Environmental Carcinogenesis & Ecotoxicology Reviews 25(4):353–377.
Acknowledgments
The writing of this paper was partially supported by NIH/NCCAM Grant T32AT001287-06. J.J.T. is a predoctoral fellow; M.N. and C.R. are faculty. Some of the research cited in this paper was supported by NSF Grant DDIG 0718313, received by M.N. and J.J.T.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thompson, J.J., Ritenbaugh, C. & Nichter, M. Reconsidering the Placebo Response from a Broad Anthropological Perspective. Cult Med Psychiatry 33, 112–152 (2009). https://doi.org/10.1007/s11013-008-9122-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11013-008-9122-2