Abstract
The incidental diagnosis of both developmental venous anomalies (DVAs) and cavernous malformations (CMs) in the central nervous system is increasing with improved imaging techniques. While classically silent diseases, these cerebrovascular pathologies can follow an aggressive course, particularly when present in the brainstem. In the last decade, substantial research has focussed on KRIT1-mediated tight junction gene expression and their role in CM development. However, our understanding of the physiologic conditions precipitating symptomatic CM development or CM haemorrhage with and without concomitant DVAs, remains lacking. The only established risk factor for CM haemorrhage is a previous history of haemorrhage, and literature currently reports trauma as the only precipitant for symptomatic events. While plausible, this occurs in a minority, with many patients experiencing occult events. This manuscript presents a hypothesis for symptomatic CM events by first discussing the anatomical pathways for intracranial venous outflow via the internal jugular veins (IJV) and vertebral venous plexus (VVP), then exploring the role of venous flow diversion away from the IJVs under physiologic stress during dynamic postural shift. The resultant increase in intracranial venous pressure can exacerbate normal and pre-existing structural DVA pathologies, with repeated exposure causing symptomatic or CM-inducing events. This pathophysiological model is considered in the context of the role of the autonomic nervous system (ANS) in postural intracranial venous outflow diversion, and how this may increase the risk of DVA or CM events. It is hoped that this hypothesis invokes further investigation into precipitants for DVA or CM events and their sequela and, also, furthers the current knowledge on pathophysiological development of DVAs and CMs.
Similar content being viewed by others
References
Sarwar M, McCormick WF (1978) Intracerebral venous angioma: case report and review. Arch Neurol 35(5):323–325
Ene C, Kaul A, Kim L (2017) Natural history of cerebral cavernous malformations. Handb Clin Neurol 143:227–232. https://doi.org/10.1016/B978-0-444-63640-9.00021-7
Gross BA, Batjer HH, Awad IA, Bendok BR (2009) Brainstem cavernous malformations. Neurosurgery 64(5):E805–EE18
Holmlund P, Johansson E, Qvarlander S, Wåhlin A, Ambarki K, Koskinen L-OD, Malm J, Eklund A (2017) Human jugular vein collapse in the upright posture: implications for postural intracranial pressure regulation. Fluids Barriers CNS 14(1):17
Tobinick E, Vega C (2006) The cerebrospinal venous system: anatomy, physiology, and clinical implications. MedGenMed 8(1):53
Doepp F, Schreiber SJ, von Münster T, Rademacher J, Klingebiel R, Valdueza JM (2004) How does the blood leave the brain? A systematic ultrasound analysis of cerebral venous drainage patterns. Neuroradiology 46(7):565–570
Huang YP, Wolf BS, Antin SP, Okudera T (1968) The veins of the posterior fossa—anterior or petrosal draining group. Am J Roentgenol 104(1):36–56
Olufsen MS, Ottesen JT, Tran HT, Ellwein LM, Lipsitz LA, Novak V (2005) Blood pressure and blood flow variation during postural change from sitting to standing: model development and validation. J Appl Physiol 99(4):1523–1537
Cirovic S, Walsh C, Fraser WD, Gulino A (2003) The effect of posture and positive pressure breathing on the hemodynamics of the internal jugular vein. Aviat Space Environ Med 74(2):125–131
Gisolf J, Van Lieshout J, Van Heusden K, Pott F, Stok W, Karemaker J (2004) Human cerebral venous outflow pathway depends on posture and central venous pressure. J Physiol 560(1):317–327
Gisolf J (2005) Postural changes in humans: effects of gravity on the circulation
Sternberg Z (2012) Autonomic dysfunction: a unifying multiple sclerosis theory, linking chronic cerebrospinal venous insufficiency, vitamin D 3, and Epstein-Barr virus. Autoimmun Rev 12(2):250–259
Clatterbuck R, Eberhart C, Crain B, Rigamonti D (2001) Ultrastructural and immunocytochemical evidence that an incompetent blood-brain barrier is related to the pathophysiology of cavernous malformations. J Neurol Neurosurg Psychiatry 71(2):188–192
Dammann P, Wrede KH, Maderwald S, El Hindy N, Mueller O, Chen B, et al (2012) The venous angioarchitecture of sporadic cerebral cavernous malformations: a susceptibility weighted imaging study at 7 T MRI. J Neurol Neurosurg Psychiatry. jnnp-2012-302599
Hong YJ, Chung T-S, Suh SH, Park CH, Tomar G, Seo KD, Kim KS, Park IK (2010) The angioarchitectural factors of the cerebral developmental venous anomaly; can they be the causes of concurrent sporadic cavernous malformation? Neuroradiology 52(10):883–891
Jakimovski D, Schneider H, Frei K, Kennes LN, Bertalanffy H (2014) Bleeding propensity of cavernous malformations: impact of tight junction alterations on the occurrence of overt hematoma. J Neurosurg 121(3):613–620
Alonso-Vanegas MA, Cisneros-Franco JM, Otsuki T (2011) Surgical management of cavernous malformations presenting with drug-resistant epilepsy. Front Neurol 2
Barrow DL (2012) Cavernous malformations. World Neurosurg 78(3–4):253–254. https://doi.org/10.1016/j.wneu.2012.05.007
Yu X-G, Wu C, Zhang H, Sun Z-H, Cui Z-Q (2016) The management of symptomatic cerebral developmental venous anomalies: a clinical experience of 43 cases. Med Sci Monit 22:4198
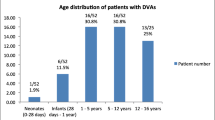
Brinjikji W, El-Masri AE-R, Wald JT, Flemming KD, Lanzino G (2017) Prevalence of cerebral cavernous malformations associated with developmental venous anomalies increases with age. Childs Nerv Syst 33(9):1539–1543
Kehrer-Sawatzki H, Wilda M, Braun VM, Richter H-P, Hameister H (2002) Mutation and expression analysis of the KRIT1 gene associated with cerebral cavernous malformations (CCM1). Acta Neuropathol 104(3):231–240
Baranoski JF, Kalani MYS, Przybylowski CJ, Zabramski JM (2016) Cerebral cavernous malformations: review of the genetic and protein–protein interactions resulting in disease pathogenesis. Front Surg3
Petersen TA, Morrison LA, Schrader RM, Hart BL (2010) Familial versus sporadic cavernous malformations: differences in developmental venous anomaly association and lesion phenotype. Am J Neuroradiol 31(2):377–382
Haseloff RF, Dithmer S, Winkler L, Wolburg H, Blasig IE, (eds) (2015) Transmembrane proteins of the tight junctions at the blood–brain barrier: structural and functional aspects. Semin Cell Dev Biol. Elsevier
Persidsky Y, Ramirez SH, Haorah J, Kanmogne GD (2006) Blood–brain barrier: structural components and function under physiologic and pathologic conditions. J NeuroImmune Pharmacol 1(3):223–236
Maeder P, Gudinchet F, Meuli R, De Tribolet N. Development of a cavernous malformation of the brain. Am J Neuroradiol 19(6):1141–1143. 1998
Dvorak HF, Brown LF, Detmar M, Dvorak AM (1995) Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol 146(5):1029–1039
Pereira VM, Geibprasert S, Krings T, Aurboonyawat T, Ozanne A, Toulgoat F, Pongpech S, Lasjaunias PL (2008) Pathomechanisms of symptomatic developmental venous anomalies. Stroke 39(12):3201–3215
Kondziolka D, Lunsford LD, Flickinger JC, Kestle JR (1995) Reduction of hemorrhage risk after stereotactic radiosurgery for cavernous malformations. J Neurosurg 83(5):825–831. https://doi.org/10.3171/jns.1995.83.5.0825
Kashefiolasl S, Bruder M, Brawanski N, Herrmann E, Seifert V, Tritt S, Konczalla J (2018) A benchmark approach to hemorrhage risk management of cavernous malformations. Neurology 90(10):e856–ee63
Ohue S, Fukushima T, Kumon Y, Ohnishi T, Friedman AH (2010) Surgical management of brainstem cavernomas: selection of approaches and microsurgical techniques. Neurosurg Rev 33(3):315–322; discussion 23–4. https://doi.org/10.1007/s10143-010-0256-7
Houtteville JP (1997) Brain cavernoma: a dynamic lesion. Surg Neurol 48(6):610–614
Gross BA, Lin N, Du R, Day AL (2011) The natural history of intracranial cavernous malformations. Neurosurg Focus 30(6):E24. https://doi.org/10.3171/2011.3.FOCUS1165
Cantu C, Murillo-Bonilla L, Arauz A, Higuera J, Padilla J, Barinagarrementeria F (2005) Predictive factors for intracerebral hemorrhage in patients with cavernous angiomas. Neurol Res 27(3):314–318. https://doi.org/10.1179/016164105X39914
Aguilar-Salinas P, Gonsales D, Brasiliense LB, Sauvageau E, Hanel RA (2017) High-energy trauma precipitating intramedullary cavernous malformation hemorrhage–a possible underreported mechanism. Cureus 9(3)
Fanous AA, Jowdy PK, Lipinski LJ, Balos LL, Li V (2016) Association between trauma and acute hemorrhage of cavernous malformations in children: report of 3 cases. J Neurosurg Pediatr 18(3):263–268
Bravi L, Rudini N, Cuttano R, Giampietro C, Maddaluno L, Ferrarini L, Adams RH, Corada M, Boulday G, Tournier-Lasserve E, Dejana E, Lampugnani MG (2015) Sulindac metabolites decrease cerebrovascular malformations in CCM3-knockout mice. Proc Natl Acad Sci 112(27):8421–8426
Ruiz D, Ha Y, Gailloud P (2009) Cerebral developmental venous anomalies: current concepts. Ann Neurol 66(3):271–283
Cakirer S (2003) De novo formation of a cavernous malformation of the brain in the presence of a developmental venous anomaly. Clin Radiol 58(3):251–256
Rammos SK, Maina R, Lanzino G (2009) Developmental venous anomalies: current concepts and implications for management. Neurosurgery 65(1):20–30
Brinjikji W, El-Masri AE-R, Wald JT, Lanzino G (2017) Prevalence of developmental venous anomalies increases with age. Stroke 116:016145
Abe T, Singer RJ, Marks MP, Norbash AM, Crowley RS, Steinberg GK (1998) Coexistence of occult vascular malformations and developmental venous anomalies in the central nervous system: MR evaluation. Am J Neuroradiol 19(1):51–57
Ozturk AK, Pricola KL (2005) Cerebral venous malformations have distinct genetic origin from cerebral cavernous malformations. Stroke
Vikkula M, Boon LM, Mulliken JB (2001) Molecular genetics of vascular malformations. Matrix Biol 20(5–6):327–335
Eerola I, Plate KH, Spiegel R, Boon LM, Mulliken JB, Vikkula M (2000) KRIT1 is mutated in hyperkeratotic cutaneous capillary–venous malformation associated with cerebral capillary malformation. Hum Mol Genet 9(9):1351–1355
Toll A, Parera E, Giménez-Arnau AM, Pou A, Lloreta J, Limaye N et al (2009) Cutaneous venous malformations in familial cerebral cavernomatosis caused by KRIT1 gene mutations. Dermatology 218(4):307–313
Tomlinson FH, Houser OW, Scheithauer BW, Sundt Jr TM, Okazaki H, Parisi JE. Angiographically occult vascular malformations: a correlative study of features on magnetic resonance imaging and histological examination. Neurosurgery 34(5):792–800. 1994
Farina M, Novelli E, Pagani R (2013) Cross-sectional area variations of internal jugular veins during supine head rotation in multiple sclerosis patients with chronic cerebrospinal venous insufficiency: a prospective diagnostic controlled study with duplex ultrasound investigation. BMC Neurol 13(1):162
Lucini D, Norbiato G, Clerici M, Pagani M (2002) Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension 39(1):184–188
Clutter WE, Bier DM, Shah SD, Cryer PE (1980) Epinephrine plasma metabolic clearance rates and physiologic thresholds for metabolic and hemodynamic actions in man. J Clin Invest 66(1):94–101
Mills PJ, Berry CC, Dimsdale JE, Nelesen RA, Ziegler MG (1993) Temporal stability of task-induced cardiovascular, adrenergic, and psychological responses: the effects of race and hypertension. Psychophysiology 30(2):197–204
Su I-C, Li C-H, Wang K-C, Lai D-M, Huang S-J, Shieh J-S, Tu YK (2009) Prediction of early secondary complications in patients with spontaneous subarachnoid hemorrhage based on accelerated sympathovagal ratios. Acta Neurochir 151(12):1631–1637
Fulton GJ, Davies MG, Hagen P-O (1997) Preservation of the endothelium in venous bypass grafts: relevance for graft patency. Asia Pac Heart J 6(2):98–106
Messerli FH (2011) Definition of hypertension. Clinician’s manual: treatment of hypertension. Springer, p. 1–2
Carter JB, Banister EW, Blaber AP (2003) Effect of endurance exercise on autonomic control of heart rate. Sports Med 33(1):33–46
Anderson JM, Van Itallie CM (2009) Physiology and function of the tight junction. Cold Spring Harb Perspect Biol 1(2):a002584
Ruíz DSM, Delavelle J, Yilmaz H, Gailloud P, Piovan E, Bertramello A et al (2007) Parenchymal abnormalities associated with developmental venous anomalies. Neuroradiology 49(12):987–995
Marasco R, Spagnoli M, Leonardi M (2009) Association between developmental venous anomalies and cavernous angiomas: a retrospective MR study. Neuroradiol J 22(2):179–185
Kostecki J, Zaniewski M, Ziaja K, Urbanek T, Kuczmik W, Krzystanek E, Ziaja D, Korzeniowski T, Majewski E, Hartel M, Swiat M, Sioma-Markowska U (2011) An endovascular treatment of chronic cerebro-spinal venous insufficiency in multiple sclerosis patients-6 month follow-up results. Neuro Endocrinol Lett 32(4):557–562
Zamboni P, Tesio L, Galimberti S, Massacesi L, Salvi F, D’alessandro R et al (2018) Efficacy and safety of extracranial vein angioplasty in multiple sclerosis: a randomized clinical trial. JAMA Neurol 75(1):35–43
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maish, W. Developmental venous anomalies and brainstem cavernous malformations: a proposed physiological mechanism for haemorrhage. Neurosurg Rev 42, 663–670 (2019). https://doi.org/10.1007/s10143-018-1039-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-1039-9