Abstract
Roux-en-Y gastric bypass (RYGB) surgery is a popular and extremely effective procedure for sustained weight loss in the morbidly obese. However, hyperoxaluria and oxalate kidney stones frequently develop after RYGB and steatorrhea has been speculated to play a role. We examined the effects of RYGB and the role of dietary fat in an obese rat model by measuring fecal fat content and transmural oxalate fluxes across the distal colon compared to sham-operated controls (SHAM). Direct measurements of fecal fat content confirmed that RYGB on a 10 % fat diet excreted 40-fold more fecal fat than SHAM and, on a 40 % fat diet, RYGB excreted sevenfold more fecal fat than SHAM fed similarly. Results from the transport studies revealed a clear effect of high dietary fat (40 %) on colonic oxalate permeability and tissue conductance (G T) with comparable oxalate fluxes in RYGB and in SHAM. Administering a diet containing 10 % fat to both groups distinguished differences between RYGB and SHAM, revealing a 40 % increase in G T in RYGB and a reversal in the direction of net oxalate flux from absorption in SHAM to secretion in RYGB. These changes in colonic oxalate permeability were associated with a fourfold increase in urinary oxalate excretion in RYGB compared to SHAM. Therefore, oxalate solubility and permeability in the RYGB model are promoted by steatorrhea and result in enhanced passive oxalate absorption and hyperoxaluria. To our knowledge, these are the first measurements of intestinal oxalate transport in rats with RYGB.





Similar content being viewed by others
References
Ammon HV, Phillips SF (1973) Inhibition of colonic water and electrolyte absorption by fatty acids in man. Gastroenterology 65:744–749
Ammon HV, Phillips SF (1974) Inhibition of ileal water absorption by intraluminal fatty acids. Influence of chain length, hydroxylation, and conjugation of fatty acids. J Clin Investig 53:205–210
Ammon HV, Thomas PJ, Phillips SF (1974) Effects of oleic and ricinoleic acids on net jejunal water and electrolyte movement. Perfusion studies in man. J Clin Investig 53:374–379
Andersson H, Bosaeus I (1981) Hyperoxaluria in malabsorptive states. Urol Int 36:1–9
Bright-Asare P, Binder HJ (1973) Stimulation of colonic secretion of water and electrolytes by hydroxy fatty acids. Gastroenterology 64:81–88
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Canales BK, Ellen J, Khan SR, Hatch M (2013) Steatorrhea and hyperoxaluria occur after gastric bypass surgery in obese rats regardless of dietary fat or oxalate. J Urol 190:1102–1109
Canales BK, Hatch M (2014) Kidney stone incidence and metabolic urinary changes after modern bariatric surgery: review of clinical studies, experimental models, and prevention strategies. Surg Obes Related Diseases 10:734–742
Canales BK, Reyes L, Reinhard MK, Khan SR, Goncalves CG, Meguid MM (2012) Renal glomerular and tubular injury after gastric bypass in obese rats. Nutrition 28:76–80
Carlsson LM, Peltonen M, Ahlin S, Anveden A, Bouchard C, Carlsson B, Jacobson P, Lonroth H, Maglio C, Naslund I, Pirazzi C, Romeo S, Sjoholm K, Sjostrom E, Wedel H, Svensson PA, Sjostrom L (2012) Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med 367:695–704
Cryer PE, Garber AJ, Hoffsten P, Lucas B, Wise L (1975) Renal failure after small intestinal bypass for obesity. Arch Intern Med 135:1610–1612
Dobbins JW, Binder HJ (1976) Effect of bile salts and fatty acids on the colonic absorption of oxalate. Gastroenterology 70:1096–1100
Dobbins JW, Binder HJ (1977) Importance of the colon in enteric hyperoxaluria. N Engl J Med 296:298–301
Duffey BG, Alanee S, Pedro RN, Hinck B, Kriedberg C, Ikramuddin S, Kellogg T, Stressman M, Moeding A, Monga M (2010) Hyperoxaluria is a long-term consequence of Roux-en-Y gastric bypass: a 2-year prospective longitudinal study. J Am Coll Surg 211:8–15
Durrani O, Morrisroe S, Jackman S, Averch T (2006) Analysis of stone disease in morbidly obese patients undergoing gastric bypass surgery. J Endourol/Endourol Soc 20:749–752
Earnest DL (1987) Enteric hyperoxaluria. Adv Intern Med 24:407–427
Earnest DL, Johnson G, Williams HE, Admirand WH (1974) Hyperoxaluria in patients with ileal resection: an abnormality in dietary oxalate absorption. Gastroenterology 66:1114–1122
Earnest DL, Williams HE, Admirand WH (1975) A physicochemical basis for treatment of enteric hyperoxaluria. Trans Assoc Am Phys 88:224–234
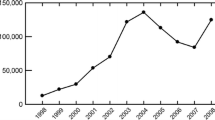
Encinosa WE, Bernard DM, Chen CC, Steiner CA (2006) Healthcare utilization and outcomes after bariatric surgery. Med Care 44:706–712
Freel RW, Hatch M, Earnest DL, Goldner AM (1980) Oxalate transport across the isolated rat colon. A re-examination. Biochim Biophys Acta 600:838–843
Frizzell RA, Koch MJ, Schultz SG (1976) Ion transport by rabbit colon. I. Active and passive components. J Membrane Biol 27:297–316
Gaginella TS, Lewis JC, Phillips SF (1976) Ricinoleic acid effects on rabbit intestine: an ultrastructural study. Mayo Clin Proc 51:569–573
Green ML, Hatch M, Freel RW (2005) Ethylene glycol induces hyperoxaluria without metabolic acidosis in rats. Am J Physiol Renal Physiol 289:F536–F543
Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW (2006) Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int 69:691–698
Hatch M, Freel RW (2003) Renal and intestinal handling of oxalate following oxalate loading in rats. Am J Nephrol 23:18–26
Hatch M, Freel RW (2008) The roles and mechanisms of intestinal oxalate transport in oxalate homeostasis. Seminars Nephrol 28:143–151
Hatch M, Freel RW, Goldner AM, Earnest DL (1981) Effect of bile salt on active oxalate transport in the colon. In: Kasper H, Goebell H (eds) Colon and nutrition. MTP Press Limited, Lancaster, Boston, The Hague
Hatch M, Freel RW, Goldner AM, Earnest DL (1983) Comparison of effects of low concentrations of ricinoleic and taurochenodeoxycholate on colonic oxalate and chloride absorption. Gastroenterology 84:1181
Hatch M, Freel RW, Vaziri ND (1994) Intestinal excretion of oxalate in chronic renal failure. J Am Soc Nephrol 5:1339–1343
Hofmann AF, Laker MF, Dharmsathaphorn K, Sherr HP, Lorenzo D (1983) Complex pathogenesis of hyperoxaluria after jejunoileal bypass surgery. Oxalogenic substances in diet contribute to urinary oxalate. Gastroenterology 84:293–300
Jandacek RJ, Heubi JE, Tso P (2004) A novel, noninvasive method for the measurement of intestinal fat absorption. Gastroenterology 127:139–144
Kathpalia SC, Favus MJ, Coe FL (1984) Evidence for size and charge permselectivity of rat ascending colon. Effects of ricinoleate and bile salts on oxalic acid and neutral sugar transport. J Clin Investig 74:805–811
Knauf F, Ko N, Jiang Z, Robertson WG, Van Itallie CM, Anderson JM, Aronson PS (2011) Net intestinal transport of oxalate reflects passive absorption and SLC26A6-mediated secretion. J Am Soc Nephrol 22:2247–2255
Kumar R, Lieske JC, Collazo-Clavell ML, Sarr MG, Olson ER, Vrtiska TJ, Bergstralh EJ, Li X (2011) Fat malabsorption and increased intestinal oxalate absorption are common after Roux-en-Y gastric bypass surgery. Surgery 149:654–661
Lieske JC, Mehta RA, Milliner DS, Rule AD, Bergstralh EJ, Sarr MG (2014) Kidney stones are common after bariatric surgery Kidney international
Matlaga BR, Shore AD, Magnuson T, Clark JM, Johns R, Makary MA (2009) Effect of gastric bypass surgery on kidney stone disease. J Urol 181:2573–2577
Nelson WK, Houghton SG, Milliner DS, Lieske JC, Sarr MG (2005) Enteric hyperoxaluria, nephrolithiasis, and oxalate nephropathy: potentially serious and unappreciated complications of Roux-en-Y gastric bypass. Surg Obesity Related Diseases 1:481–485
Racusen LC, Binder HJ (1979) Ricinoleic acid stimulation of active anion secretion in colonic mucosa of the rat. J Clin Investig 63:743–749
Siener R, Glatz S, Nicolay C, Hesse A (2004) The role of overweight and obesity in calcium oxalate stone formation. Obes Res 12:106–113
Sinha MK, Collazo-Clavell ML, Rule A, Milliner DS, Nelson W, Sarr MG, Kumar R, Lieske JC (2007) Hyperoxaluric nephrolithiasis is a complication of Roux-en-Y gastric bypass surgery. Kidney Int 72:100–107
Sjostrom L, Peltonen M, Jacobson P, Sjostrom CD, Karason K, Wedel H, Ahlin S, Anveden A, Bengtsson C, Bergmark G, Bouchard C, Carlsson B, Dahlgren S, Karlsson J, Lindroos AK, Lonroth H, Narbro K, Naslund I, Olbers T, Svensson PA, Carlsson LM (2012) Bariatric surgery and long-term cardiovascular events. JAMA 307:56–65
Spak E, Bjorklund P, Helander HF, Vieth M, Olbers T, Casselbrant A, Lonroth H, Fandriks L (2010) Changes in the mucosa of the Roux-limb after gastric bypass surgery. Histopathology 57:680–688
Stauffer JQ (1977) Hyperoxaluria and intestinal disease. The role of steatorrhea and dietary calcium in regulating intestinal oxalate absorption. Am J Digestive Diseases 22:921–928
Taylor EN, Curhan GC (2006) Body size and 24-hour urine composition. Am J Kidney Diseases 48:905–915
Acknowledgments
The authors thank Bryce Bergeron, Zachary Marmetschke, Shannon Moore, and Shreya Mishra for excellent technical assistance and animal husbandry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by NIH grants DK088892 (M. Hatch) and DK089000 (B.K. Canales), an AUA Foundation Rising Star in Urology Research Award in conjunction with Astellas Global Development, Inc. (B.K. Canales), and a materials grant from Ethicon Endo-Surgery (B.K. Canales).
Conflict of interest
The first author, M. Hatch, declares no conflict of interest and the second author, B.K. Canales, declares no conflict of interest.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals in this study were followed. This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Hatch, M., Canales, B.K. The mechanistic basis of hyperoxaluria following gastric bypass in obese rats. Urolithiasis 44, 221–230 (2016). https://doi.org/10.1007/s00240-015-0836-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-015-0836-7