Abstract
Purpose
Acute stroke treatment requires simple, quick and accurate detection of early ischemic changes to facilitate treatment decisions guided by published selection criteria. The aim of this study was to determine the accuracy and reliability of multiphase computed tomography angiography (mCTA) perfusion hypoattenuation for detecting early severe ischemia.
Methods
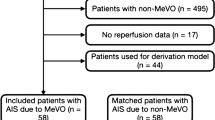
Non-contrast CT (NCCT), mCTA for regional leptomeningeal score (mCTA-rLMC), and mCTA perfusion lesion visibility (mCTA-arterial and mCTA-venous) were assessed blinded to clinical information in patients treated with endovascular therapy (EVT). The extent of early ischemia defined by regions of hypoattenuation was evaluated by the Alberta Stroke Program Early CT Score (ASPECTS). The ASPECTS scores were dichotomized based on the American Heart Association (AHA) guidelines for EVT selection, ASPECTS ≥6 vs. <6. The diagnostic accuracy was calculated by comparison to 24-h magnetic resonance imaging (MRI) or CT ASPECTS. Inter-observer reliability of NCCT and mCTA ASPECTS was evaluated. Machine learning models were used to predict the clinical follow-up outcome, e.g. National Institutes of Health Stroke scale (NIHSS) and modified Rankin scale (mRS) from baseline imaging data and patient information.
Results
A total of 89 acute stroke patients (68 ± 15 years of age) were analyzed (33 TICI-0, 56 TICI-2b or 3). Median baseline NIHSS was 17. The mCTA-venous had a large effect on accurately identifying early ischemia when dichotomized for ASPECTS ≥6 vs <6 (likelihood ratio [LR+] > 10 vs. [LR−] < 0.29) compared to the moderate effect of NCCT ([LR+] = 6.7; [LR−] = 0.56) and mCTA-rLMC [(LR+ = 8.0; (LR–) = 0.83)]. The inter-observer reliability in mCTA-venous was almost perfect for all ASPECTS regions except the internal capsule. The machine learning support factor regression model identified mCTA-venous as the most important imaging covariate for predicting 24-h NIHSS and 90-day mRS.
Conclusion
The assessment of mCTA-venous permits a more accurate detection of early ischemia than NCCT and mCTA-rLMC score and is predictive of clinical outcome. We would recommend the inclusion of mCTA perfusion lesion in future endovascular trials aiming at extending current AHA guidelines for EVT in stroke patients with low ASPECTS.


Similar content being viewed by others
Change history
03 June 2019
<Emphasis Type="Bold">Correction to:</Emphasis>
<Emphasis Type="Bold">Clin Neuroradiol 2018</Emphasis>
<ExternalRef><RefSource>https://doi.org/10.1007/s00062-018-0717-x</RefSource><RefTarget Address="10.1007/s00062-018-0717-x" TargetType="DOI"/></ExternalRef>
Unfortunately, the author list of the original version of this article contains a mistake. The middle name of the author “Rani Gupta Sah” was erroneously tagged as part of the surname in the article’s metadata.
This mistake
References
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–95.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355:1670–4.
Gupta AC, Schaefer PW, Chaudhry ZA, Leslie-Mazwi TM, Chandra RV, González RG et al. Interobserver reliability of baseline noncontrast ct alberta stroke program early ct score for intra-arterial stroke treatment selection. AJNR Am J Neuroradiol. 2012;33:1046–9.
Coutts SB, Hill MD, Demchuk AM, Barber PA, Pexman JH, Buchan AM. ASPECTS reading requires training and experience. Stroke. 2003;34:e179; author reply e179.
Brozici M, van der Zwan A, Hillen B. Anatomy and functionality of leptomeningeal anastomoses: A review. Stroke. 2003;34:2750–62.
Liebeskind DS. Stroke: the currency of collateral circulation in acute ischemic stroke. Nat Rev Neurol. 2009;5:645–6.
Finlayson O, John V, Yeung R, Dowlatshahi D, Howard P, Zhang L et al. Interobserver agreement of aspect score distribution for noncontrast CT, CT angiography, and CT perfusion in acute stroke. Stroke. 2013;44:234–6.
Coutts SB, Lev MH, Eliasziw M, Roccatagliata L, Hill MD, Schwamm LH et al. ASPECTS on CTA source images versus unenhanced CT: added value in predicting final infarct extent and clinical outcome. Stroke. 2004;35:2472–6.
Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM et al. Multiphase ct angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015;275:510–20.
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–35.
Pexman JH, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. 2001;22:1534–42.
Rodriguez-Luna D, Dowlatshahi D, Aviv RI, Molina CA, Silva Y, Dzialowski I et al. Venous phase of computed tomography angiography increases spot sign detection, but intracerebral hemorrhage expansion is greater in spot signs detected in arterial phase. Stroke. 2014;45:734–9.
Menon BK, Smith EE, Modi J, Patel SK, Bhatia R, Watson TW et al. Regional leptomeningeal score on CT angiography predicts clinical and imaging outcomes in patients with acute anterior circulation occlusions. AJNR Am J Neuroradiol. 2011;32:1640–5.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Kononenko I, Robnik-Šikonja M. An adaptation of relief for attribute estimation in regression. In: Proceedings of the Fourteenth International Conference on Machine Learning (ICML ’97). 1997. pp. 296–304.
Chang CC, Lin CJ. LIBSVM: a library for support vector machines. ACM Trans Intell Syst Technol. 2011;2:27:1–27:27.
Robnik-Šikonja M, Kononenko I. Theoretical and empirical analysis of ReliefF and RReliefF. Mach Learn 2003;53:23–69.
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–18.
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21.
Acknowledgements
We acknowledge the Calgary Stroke Program and the Seaman MR Center for their support. Supported by a Canadian Institute of Health Research Operating Grant and bridge funding from the Faculty of Medicine, University of Calgary.
Funding
Supported by a Canadian Institute of Health Research Operating Grant and bridge funding from the Faculty of Medicine, University of Calgary.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Goyal has a patent and licensing agreement with GE Healthcare re: systems of stroke diagnosis. In addition, he has a consulting agreement with Medtronic, Stryker, Microvention, Cenernovus. Medtronic has provided an unrestricted research grant to the University of Calgary for the HERMES collaboration. M. Goyal is the Chair of this collaboration. M. Reid, A.O. Famuyide, N.D. Forkert, A. Sahand Talai, J.W. Evans, A. Sitaram, M. Hafeez, M. Najm, B.K. Menon, A. Demchuk, R. Gupta Sah, C.D. d’Esterre and P. Barber declare that they have no competing interests.
Ethical standards
The local ethics boards approved the study. All participants gave informed consent prior to their inclusion in this study. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Caption Electronic Supplementary Material
62_2018_717_MOESM1_ESM.docx
The positive predictive values, negative predictive values, positive likelihood ratios (LR+) and negative likelihood ratios (LR-) of ASPECTS scoring on NCCT, mCTA-arterial, mCTA-venous and mCTA-rLMC compared to CT/MRI infarction at 24-hours dichotimized by TICI score and by onset to CT time (0–3 or >3 hours).
Rights and permissions
About this article
Cite this article
Reid, M., Famuyide, A.O., Forkert, N.D. et al. Accuracy and Reliability of Multiphase CTA Perfusion for Identifying Ischemic Core. Clin Neuroradiol 29, 543–552 (2019). https://doi.org/10.1007/s00062-018-0717-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-018-0717-x