Abstract
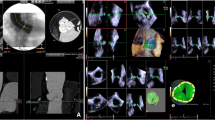
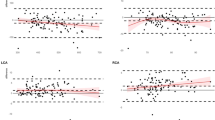
To compare a semi-automatic software tool for the measurement of aortic annulus dimensions with manual measurements by expert readers and to analyze whether and to what extent interchangeability exists between semi-automatic and manual measurements. We retrospectively included 374 consecutive patients with high-grade aortic stenosis who had undergone CT-angiography of the heart prior to trans-catheter aortic valve replacement (TAVR). In independent analyses, two expert readers manually measured aortic annulus dimensions (long axis, short axis, circumference, area) as well as the distance of the coronary ostia from the annulus plane. A third independent reader performed annulus evaluation using a software tool for semi-automatic detection and measurement of the annulus plane. Intraclass correlation coefficients (ICC) and Bland–Altman analysis was used to compare both manual measurements as well as manual and semi-automatic measurements of annulus parameters. Using the respective measurements we simulated size selection for a Sapien XT transcatheter heart valve (THV). Interchangeability of methods was addressed by calculation of the estimated individual equivalence index γ. There was excellent agreement between both expert observers in manual measurements of the annulus with ICC’s in the range 0.89–0.94 for all anatomic parameters. Similar high agreements were observed between semi-automatic and manual measurements, with ICC’s in the range of 0.89–0.95. THV size recommendation based on manual versus semiautomatic measurements agreed in 80.7% of cases while agreement between both expert readers concerning THV size recommendation was 80.6%. Semi-automatic measurements of anatomic parameters of the aortic root show high agreement and interchangeability with manual measurements in CT-angiography prior to TAVR.





Similar content being viewed by others
References
Carabello BA (2002) Aortic stenosis. N Engl J Med 346:677–682. https://doi.org/10.1056/NEJMcp010846
Mack MJ, Leon MB, Smith CR et al (2015) 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385:2477–2484. https://doi.org/10.1016/S0140-6736(15)60308-7
Kapadia SR, Leon MB, Makkar RR et al (2015) 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385:2485–2491. https://doi.org/10.1016/S0140-6736(15)60290-2
Adams DH, Popma JJ, Reardon MJ et al (2014) Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 370:1790–1798. https://doi.org/10.1056/NEJMoa1400590
Haussig S, Schuler G, Linke A (2014) Worldwide TAVI registries: what have we learned? Clin Res Cardiol 103:603–612. https://doi.org/10.1007/s00392-014-0698-y
Leon MB, Smith CR, Mack MJ et al (2016) Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 374:1609–1620. https://doi.org/10.1056/NEJMoa1514616
Achenbach S, Delgado V, Hausleiter J et al (2012) SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr 6:366–380. https://doi.org/10.1016/j.jcct.2012.11.002
Binder RK, Webb JG, Willson AB et al (2013) The impact of integration of a multidetector computed tomography annulus area sizing algorithm on outcomes of transcatheter aortic valve replacement. J Am Coll Cardiol 62:431–438. https://doi.org/10.1016/j.jacc.2013.04.036
Watanabe Y, Morice MC, Bouvier E et al (2013) Automated 3-dimensional aortic annular assessment by multidetector computed tomography in transcatheter aortic valve implantation. JACC Cardiovasc Interv 6:955–964. https://doi.org/10.1016/j.jcin.2013.05.008
Delgado V, Ng ACT, Schuijf JD et al (2011) Automated assessment of the aortic root dimensions with multidetector row computed tomography. Ann Thorac Surg 91:716–723. https://doi.org/10.1016/j.athoracsur.2010.09.060
Foldyna B, Jungert C, Luecke C et al (2015) CT evaluation prior to transapical aortic valve replacement: semi-automatic versus manual image segmentation. Int J Cardiovasc Imaging 31:1233–1242. https://doi.org/10.1007/s10554-015-0662-6
Van Linden A, Kempfert J, Blumenstein J et al (2014) Manual versus automatic detection of aortic annulus plane in a computed tomography scan for transcatheter aortic valve implantation screening. Eur J Cardio-thorac Surg 46:207–212. https://doi.org/10.1093/ejcts/ezt600
Queirós S, Dubois C, Morais P et al (2017) Automatic 3D aortic annulus sizing by computed tomography in the planning of transcatheter aortic valve implantation. J Cardiovasc Comput Tomogr 11:25–32. https://doi.org/10.1016/j.jcct.2016.12.004
Schwarz F, Lange P, Zinsser D et al (2014) CT-angiography-based evaluation of the aortic annulus for prosthesis sizing in transcatheter aortic valve implantation (TAVI)-predictive value and optimal thresholds for major anatomic parameters. PLoS ONE 9:e103481. https://doi.org/10.1371/journal.pone.0103481
Obuchowski NA, Subhas N, Schoenhagen P (2014) Testing for interchangeability of imaging tests. Acad Radiol 21:1483–1489. https://doi.org/10.1016/j.acra.2014.07.004
Obuchowski NA (2001) Can electronic medical images replace hard-copy film? Defining and testing the equivalence of diagnostic tests. Stat Med 20:2845–2863
Lou J, Obuchowski NA, Krishnaswamy A et al (2015) Manual, semiautomated, and fully automated measurement of the aortic annulus for planning of transcatheter aortic valve replacement (TAVR/TAVI): analysis of interchangeability. J Cardiovasc Comput Tomogr 9:42–49. https://doi.org/10.1016/j.jcct.2014.11.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Konstantin Nikolaou, Fabian Bamberg and Florian Schwarz have received speaker honoraria from Siemens Healthineers. Konstantin Nikolaou has received speaker honoraria from Bracco Imaging Deutschland GmbH. Fabian Bamberg has received an unrestricted research grant from Bayer Healthcare AG. All other authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. This article does not contain any studies with animals performed by any of the authors.
Informed consent
All patients gave informed consent for MDCT. Due to the retrospective nature of this study, the local IRB waived the necessity to obtain informed consent beyond these routine clinical requirements.
Appendices
Appendix 1
Agreement between manual measurements of the aortic root by reader 1 and reader 2 reported as intraclass correlation coefficient and Bland–Altman-analysis parameters in image quality subgroups.
Diameter long axis | Diameter short axis | Annulus circumference | Annulus area | Distance of left coronary ostium | Distance of right coronary ostium | |
|---|---|---|---|---|---|---|
Sub-group IQ 4 or 5 (n = 258) | ||||||
ICC (95% CI) | 0.90 (0.87; 0.92) | 0.89 (0.86; 0.91) | 0.94 (0.92; 0.95) | 0.94 (0.93; 0.96) | 0.79 (0.74; 0.83) | 0.78 (0.72; 0.82) |
Mean difference | 0.00 cm | 0.01 cm | 0.05 cm | 0.03 cm2 | 0.02 cm | 0.06 cm |
SD of differences | 0.12 cm | 0.11 cm | 0.23 cm | 0.26 cm2 | 0.18 cm | 0.24 cm |
Sub-group IQ 2 or 3 (n = 97) | ||||||
ICC (95% CI) | 0.88 (0.83; 0.92) | 0.89 (0.84; 0.93) | 0.93 (0.90; 0.95) | 0.95 (0.92; 0.96) | 0.74 (0.64; 0.82) | 0.65 (0.52; 0.75) |
Mean difference | 0.00 cm | 0.00 cm | 0.11 cm | 0.07 cm2 | 0.01 cm | 0.04 cm |
SD of differences | 0.14 cm | 0.12 cm | 0.26 cm | 0.29 cm2 | 0.19 cm | 0.25 cm |
p for difference in ICC’s | 0.42 | 1.0 | 0.51 | 0.44 | 0.32 | 0.03 |
Appendix 2
Agreement between manual and semiautomatic measurements in various subgroups:
Signal-to-noise ratio (SNR)
Diameter long axis | Diameter short axis | Annulus circum-ference | Annulus area | Distance of left coronary ostium | Distance of right coronary ostium | |
|---|---|---|---|---|---|---|
SNR > SNRmedian (n = 167) | ||||||
ICC (95% CI) | 0.89 (0.86; 0.92) | 0.86 (0.81; 0.89) | 0.95 (0.93; 0.96) | 0.95 (0.94; 0.96) | 0.69 (0.62; 0.76) | 0.75 (0.68; 0.81) |
Mean difference | 0.03 cm | 0.01 cm | 0.01 cm | 0.08 cm2 | 0.01 cm | 0.04 cm |
SD of differences | 0.13 cm | 0.13 cm | 0.22 cm | 0.26 cm2 | 0.23 cm | 0.26 cm |
SNR < SNR25th percentile (n = 87) | ||||||
ICC (95% CI) | 0.88 (0.82; 0.92) | 0.88 (0.82; 0.92) | 0.92 (0.88; 0.95) | 0.93 (0.90; 0.95) | 0.75 (0.64; 0.83) | 0.74 (0.64; 0.82) |
Mean difference | 0.01 cm | 0.03 cm | 0.02 cm | 0.04 cm2 | 0.03 cm | 0.03 cm |
SD of differences | 0.12 cm | 0.12 cm | 0.29 cm | 0.31 cm | 0.23 cm | 0.26 cm |
p value for difference of ICC’s | 0.73 | 0.54 | 0.07 | 0.20 | 0.35 | 0.87 |
Degree of calcification
Diameter long axis | Diameter short axis | Annulus circum-ference | Annulus area | Distance of left coronary ostium | Distance of right coronary ostium | |
|---|---|---|---|---|---|---|
Calcifications = 1 (n = 97) | ||||||
ICC (95% CI) | 0.88 (0.82; 0.92) | 0.86 (0.80; 0.90) | 0.92 (0.89; 0.95) | 0.93 (0.90; 0.95) | 0.63 (0.49; 0.73) | 0.79 (0.71; 0.85) |
Mean difference | 0.02 cm | 0.02 cm | 0.01 cm | 0.10 cm | 0.00 cm | 0.06 cm |
SD of differences | 0.12 cm | 0.12 cm | 0.25 cm | 0.27 cm | 0.24 cm | 0.24 cm |
Calcifications = 2 (n = 205) | ||||||
ICC (95% CI) | 0.89 (0.86; 0.92) | 0.86 (0.82; 0.89) | 0.95 (0.94; 0.96) | 0.95 (0.94; 0.96) | 0.71 (0.64; 0.76) | 0.71 (0.63; 0.77) |
Mean difference | 0.02 cm | 0.05 cm | 0.01 cm | 0.05 cm | 0.00 cm | 0.04 cm |
SD of differences | 0.13 cm | 0.27 cm | 0.22 cm | 0.27 cm | 0.23 cm | 0.26 cm |
Calcifications = 3 (n = 53) | ||||||
ICC (95% CI) | 0.90 (0.84; 0.94) | 0.85 (0.76; 0.91) | 0.94 (0.90; 0.97) | 0.95 (0.92; 0.97) | 0.76 (0.61; 0.85) | 0.81 (0.69; 0.88) |
Mean difference | 0.03 cm | 0.03 cm | 0.02 cm | 0.08 cm2 | 0.04 cm | 0.02 cm |
SD of differences | 0.12 cm | 0.11 cm | 0.24 cm | 0.26 cm2 | 0.22 cm | 0.23 cm |
Rights and permissions
About this article
Cite this article
Zinsser, D., Baumann, A.B., Winter, K.S. et al. Semi-automatic CT-angiography based evaluation of the aortic annulus in patients prior to TAVR: interchangeability with manual measurements. Int J Cardiovasc Imaging 34, 1657–1667 (2018). https://doi.org/10.1007/s10554-018-1377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1377-2