Abstract
The current study shows the usefulness of dengue-3- and dengue-4-specific phage-displayed antibody fragments as tools for viral detection and serotyping in sera from infected individuals. C6/36 HT cells were inoculated with acute-phase sera from patients, and supernatants were collected daily and analyzed by ELISA using phage-displayed antibody fragments as serotype-specific detector reagents. Serotyping of most samples was possible as early as two to three days postinoculation. Results were comparable with those obtained by indirect immunofluorescence assay but were obtained in a shorter period of time (<1 week). Phage-displayed antibody fragments were better tools for diagnosis and serotyping than their soluble counterparts. Our approach combines the advantages of viral isolation and ELISA techniques. These results could be the basis for the development of a high-throughput method for identifying dengue virus serotypes, which is crucial for the management and control of the disease.
Similar content being viewed by others
Introduction
Dengue is currently the most important mosquito-borne viral disease of humans worldwide [6]. Four viruses (dengue virus 1–4) belonging to the family Flaviviridae, genus Flavivirus, are responsible for this disease, which can range from asymptomatic infections, undifferentiated fever and classical dengue fever to severe forms of the disease: dengue haemorrhagic fever (DHF) and dengue shock syndrome [10]. Viral, host and epidemiological factors are involved in the severe outcome of the illness [13]. Secondary infection by a different serotype is considered the most important host risk factor for DHF [13]. Additionally, the specific serotype combination in sequential infections has also been identified as an important associated factor [3]. Due to the expanding geographic distribution of both the mosquito vector and the four dengue virus serotypes, the frequency of epidemics is increasing in many countries. Co-circulation of at least two serotypes during the same outbreak is usual [13]. Therefore, people are constantly at risk of having a secondary contact with a different serotype, and concurrent infections definitely occur [21]. Thus, rapid diagnosis of the disease and early and accurate serotype identification during the acute phase of illness are essential for disease control and could significantly reduce morbidity and mortality [25]. In addition, detection of the circulating serotypes is useful for epidemiological and pathological studies.
Virus isolation and subsequent identification via indirect immunofluorescence assay (IFA) [14] or PCR [20] allow the detection and serotyping of dengue virus during the acute phase of the illness. Due to the long time (usually more than seven days) required for virus identification by IFA [35] and to the need for specialized laboratory equipment for PCR techniques, immunoenzymatic methods have received attention. Detection of circulating dengue nonstructural protein 1 (NS1) in the serum of infected patients has been reported [39]. Despite the high sensitivity of these assays, specificity remains a problem. Preferential recognition of a given serotype and some cross-reactivity with the remaining ones have been shown [1]. Recently, a panel of highly specific monoclonal antibodies (Mabs) against NS1 protein was obtained through hybridoma technology [16] and used to detect dengue virus 1 (Den-1) [38].
Antibody phage display technology is an additional alternative for isolating antibodies against important viral pathogens [37] useful for viral diagnosis [9, 32]. We had previously obtained a panel of antibody fragments specifically recognizing viral particles of Den-3 and Den-4 serotypes using this technology [5]. The objective of the current work is to evaluate the usefulness of such phage-displayed antibody fragments in a serotyping method that combines the advantages of virus isolation and ELISA techniques. The suitability of phage-displayed antibody fragments as tools for an early detection and serotyping of dengue virus is shown.
Materials and methods
Dengue viruses and cell culture
Den-1 Angola strain (kindly donated by Dr. R. Shope, University of Texas), Den-2 A15 strain [17], Den-3 116/00 strain [12] and Den-4 Dominica strain (also donated by Dr. R. Shope), were used in this study (Table 1). Aedes albopictus C6/36 HT cells (ATCC), grown in 24-well plates, were inoculated with the virus strains using the rapid centrifugation assay as described [26]. Undiluted virus stocks and 10-fold virus dilutions (from 10−1 to 10−3 or 10−4, depending on the virus stock) were inoculated in individual wells and incubated at 33°C and 5% CO2. Viruses were diluted in MEM (Gibco, USA) supplemented with 2% heat-inactivated fetal bovine serum. Culture supernatant samples were collected daily at different times postinoculation (from the second to the seventh day). Supernatants were directly used for ELISA (see section “Detection of dengue virus in supernatants using Mab H3-6”). Cells were collected at the seventh day and evaluated by IFA, using serotype-specific Mabs [14] to confirm the presence of viral particles in inoculated cells. Non-inoculated cells were run in parallel as virus-inoculated cells to obtain negative controls.
Serum samples and virus isolation
Serum samples collected during Cuban outbreaks [7, 12, 18] from 32 patients with a confirmed diagnosis of dengue fever were studied. Samples were obtained within the first four days after onset of fever. Virus detection and serotyping in each sample were carried out by viral isolation [26], IFA [14] and RT-nested PCR [20] with some modifications [27]. Twelve samples were positive for Den-3, nine for Den-4, seven for Den-2 and four for Den-1. Twenty-five sera from dengue-negative individuals (confirmed by viral isolation and anti-dengue IgM antibodies [34]) were also included. Twenty of these sera were from patients with infections from other pathogens (10 patients infected with influenza virus and 10 patients infected with Leptospira spp.). These samples were provided by the National Influenza Laboratory and the National Reference Laboratory on Leptospira of the Tropical Medicine Institute Pedro Kourí. The remaining five sera were from healthy individuals. All serum samples were diluted 1:20 in MEM (supplemented with 2% heat-inactivated fetal bovine serum) and inoculated in duplicate in C6/36 HT cell culture as described in section “Dengue viruses and cell culture” in order to collect supernatants daily from the second to the seventh day. Cells were harvested at either 3 or 7 days postinoculation (from each replicate) and tested by IFA [14]. Non-inoculated cells were run in parallel to serum-inoculated cells to obtain negative controls.
Virus titration
Plaque titration of serum and supernatant samples was performed by direct plaque assay on BHK-21 cells as described previously [24], with modifications [2].
Antibodies
Phage-displayed antibody fragments C, D, E, H (specific for Den-3 serotype) and M (specific for Den-4 serotype) were derived from a human single-chain Fv (scFv) naïve library. Such phage-displayed antibody fragments were cross-reactive against different strains within the corresponding serotype [5]. Phage particles were rescued on a 50-ml scale and purified [22]. Each purified phage was tested by ELISA on virus-containing supernatants as described previously [5]. Phage dilutions producing an absorbance at 492 nm of 1.50 ± 0.1 were chosen for the following experiments.
ScFvs derived from clones C and M were produced as soluble antibody fragments on a 200-ml scale using isopropyl-β-d-thiogalactopyranoside (IPTG), purified by immobilized metal affinity chromatography (IMAC), and tested by ELISA on virus-containing supernatants as described previously [5]. ScFv dilutions producing an absorbance at 492 nm of 1.50 ± 0.1 were chosen for the following experiments.
Polyclonal human anti-dengue IgG [34] was used as capture antibody.
The broadly cross-reactive anti-dengue mouse Mab H3-6 [15] was used to confirm the presence or absence of viruses in supernatant samples.
Detection of dengue virus in supernatants using Mab H3-6
Supernatants from virus/serum-inoculated cells were evaluated by ELISA using Mab H3-6 in order to confirm the presence or absence of virus particles. Polystyrene plates (Costar, USA) were coated overnight at 4°C with human anti-dengue IgG at 2.5 μg/ml in phosphate-buffered saline (PBS). Plates were blocked with PBS containing 4% skim milk powder (M-PBS) for 1 h at room temperature (RT, 20-25°C). Supernatants from virus/serum-inoculated and non-inoculated cells, collected at different times postinoculation, were added directly to the plates. After 1 h at 37°C, plates were washed five times with PBS containing 0.1% Tween 20 (PBS-T). Mab H3-6 at 10 μg/ml in M-PBS was added to the wells. Plates were incubated for 1 h at RT and washed five times with PBS-T. An anti-mouse IgG/horseradish peroxidase conjugate (Amersham, USA), diluted 1:5000 in M-PBS, was added for 1 h at RT. Plates were washed eight times with PBS-T, and substrate solution (500 μg/ml ortho phenylenediamine and 0.015% hydrogen peroxide in 0.1 mol/l citrate buffer, pH 5.5) was added. The reaction was stopped 15 min later with 5 M sulphuric acid. The absorbances at 492 nm were determined using a microplate reader (MRX, Germany). Samples producing absorbances higher than twice the mean value of the negative controls (supernatants from non-inoculated cells) were considered to be positive.
Detection and serotyping of Den-3 and Den-4 viruses in supernatants from dengue-infected cells using phage ELISA
Supernatants from virus/serum-inoculated cells were evaluated by ELISA. The first steps (plate coating, blocking, addition of supernatants and washing) were performed as described in section “Detection of dengue virus in supernatants using Mab H3-6”. Each purified phage (appropriately diluted in M-PBS) was added to the wells. Plates were incubated for 1 h at RT and washed five times with PBS-T. An anti-M13 Mab (directed to the pVIII coat protein) coupled to horseradish peroxidase (Pharmacia, Sweden), diluted 1:5000 in M-PBS, was added to the plates and incubated for 1 h at RT. The next steps (from addition of substrate solution to absorbance measurement) were performed as described in section “Detection of dengue virus in supernatants using Mab H3-6”. Samples producing absorbances higher than twice the mean value of the negative controls (supernatants from non-inoculated cells) were considered to be positive.
Detection and serotyping of Den-3 and Den-4 viruses using soluble recombinant antibody fragments
Supernatants from serum-inoculated cells were evaluated in parallel by ELISA using phage-displayed antibody fragments and their soluble scFv counterparts (when they were available, C and M clones) in order to compare the suitability of both antibody formats for the detection and serotyping of dengue virus. Detection by soluble scFv was performed using an assay similar to the one described in section “Detection of dengue virus in supernatants using Mab H3-6”. Plate coating, blocking, addition of supernatants and washing were done as described in section “Detection of dengue virus in supernatants using Mab H3-6”. Purified soluble antibody fragments C or M, diluted at 5 and 1 μg/ml, respectively, in M-PBS, were incubated on the plates for 1 h at RT. Plates were washed five times with PBS-T, and Mab 9E10 (directed to the c-myc tag fused to antibody fragments) at 10 μg/ml in M-PBS was added for 1 h at RT. After washing again, an anti-mouse IgG/horseradish peroxidase conjugate (Amersham, USA) diluted 1:5000 in M-PBS was added for 1 h at RT. The next steps were performed as described in section “Detection of dengue virus in supernatants using Mab H3-6”. Samples producing absorbances higher than twice the mean value of the negative controls (supernatants from non-inoculated cells) were considered to be positive.
Results
Detection of Den-3 and Den-4 viruses using phage-displayed antibody fragments in supernatants harvested from cells infected with different viral strains
In order to evaluate whether our phage-displayed antibody fragments are suitable for Den-3 and Den-4 serotype determination early in infection, these recombinant fragments were first tested in ELISA with culture supernatants harvested from cells infected with Den-1, Den-2, Den-3 and Den-4 virus at different times postinoculation (from two to seven days). Each serotype had been inoculated at several viral titers. IFA performed on day 7 confirmed viral isolation and serotyping. Table 2 shows the times postinoculation at which anti-Den-3 phage-displayed antibody fragments first detected the virus in supernatants. Den-3 was detected in supernatants harvested from the cells inoculated with the higher viral titers (104 and 103 pfu/ml) as early as 2 days postinoculation. Supernatants from cells inoculated with lower viral titers became positive later, between 3 and 5 days postinoculation. Supernatants collected from Den-1-, Den-2- and Den-4-inoculated cells were negative at all times postinoculation, as expected, even though these supernatants started to be positive at 2-4 days postinoculation when evaluated with the cross-reactive Mab H3-6.
The recognition ability of C, D, E and H antibody fragments was similar, making it possible to use any of them for serotype determination in patients’ samples. Detailed results obtained with the H phage-displayed antibody fragment are shown in Fig. 1.
Detection of dengue 3 virus by phage ELISA in cell culture supernatants. C6/36 HT cells were inoculated with undiluted virus stock and 10-fold virus dilutions, and supernatants were collected daily and evaluated by ELISA. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages displaying H antibody fragment were added to the plates. Bound phages were detected with an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. The black line represents twice the mean value of the negative controls (supernatants from non-inoculated cells)
Anti-Den-4 phage-displayed M antibody fragment was also suitable for early dengue virus detection (Fig. 2). Supernatants harvested from the cells inoculated with the higher viral titers (103 and 102 pfu/ml) were positive from day 2 postinoculation onward. Supernatants from cells inoculated with lower viral titers became positive at day 3 postinoculation. Supernatants from cells infected with the three remaining serotypes gave negative results at all times postinoculation, even though they started to be positive between the second and the fourth day of culture when using the cross-reactive Mab H3-6.
Detection of dengue 4 virus by phage ELISA in cell culture supernatants. C6/36 HT cells were inoculated with undiluted virus stock and 10-fold virus dilutions, and supernatants were collected daily and evaluated by ELISA. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages displaying anti-dengue 4 M antibody fragment were added to the plates. Bound phages were detected with an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. The black line represents twice the mean value of the negative controls (supernatants from non-inoculated cells)
All of these results indicate that anti-Den-3 and anti-Den-4 phage-antibody fragments are potential tools for the early detection and serotype determination of dengue virus in infected cell cultures.
Serotyping Den-3 and Den-4 viruses in supernatants from serum-inoculated cells using phage-displayed antibody fragments
To address the question of whether Den-3- and Den-4-specific phage-displayed antibody fragments can be reliably used for early dengue virus serotyping in infected patients, a panel of viremic sera from Den-3, Den-4, Den-1 and Den-2-infected patients as well as negative sera were tested. C6/36 HT cells were inoculated with each of these samples, and supernatants were analyzed by phage ELISA. IFA performed on day 7 confirmed viral isolation.
Table 3 shows the times postinoculation at which the virus was first detected by phage ELISA in supernatants from cell cultures inoculated with serum from Den-3 patients (serum viral titers ranging from 5.6 × 102 to 3.8 × 104 pfu/ml). All of these supernatants were positive from day 4 postinoculation onward. Most of them (10/12) became positive even earlier, between days 2 and 3 postinoculation, and in these cases, IFA was also positive beginning on day 3 (Fig. 3a, b), making the two serotyping methods comparable. In one case (serum 4) phage ELISA using H recombinant antibody fragment was able to detect viral particles in the supernatant sample taken on the third day, whereas IFA performed at the same postinoculation time was negative (Fig. 3c) and became positive on day 7 (Fig. 3d). This result could indicate an advantage of phage ELISA for certain samples. Since the remaining anti-Den-3 recombinant antibody fragments were not able to detect viral particles in the same sample, further experiments with a larger serum panel will help to define the best anti-Den-3 antibody fragment for virus detection in order to achieve maximum sensitivity in a shorter time.
Indirect immunofluorescence assay (IFA) of dengue 3 serum-inoculated C6/36 HT cells. Viral particles were detected with dengue-3-specific mouse monoclonal antibody 8A1 and an anti-mouse IgG conjugated to FITC. IFA results for serum 2-inoculated cells—collected 3 (a) and 7 (b) days postinoculation—and IFA results for serum 4-inoculated cells—collected 3 (c) and 7 (d) days postinoculation—are shown. Magnification 400×
Supernatants from negative and Den-1-, Den-2- and Den-4-positive serum-inoculated cells were negative by anti-Den-3 phage ELISA at all times postinoculation, whereas the presence of viral particles in supernatants from all dengue sera-inoculated cells was shown with the cross-reactive anti-dengue H3-6 Mab between days 2 and 6 postinoculation. These results confirmed the absence of undesired serotype cross-reactivities in the phage ELISA. Figure 4 shows detailed results with the whole serum panel, taking phage-displayed H antibody fragment as an example of detector antibody.
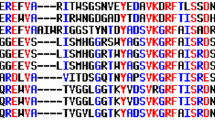
Dengue 3 virus detection by phage ELISA in supernatants from cells inoculated with patients’ sera. C6/36 HT cells were inoculated with a panel of acute-phase serum specimens from twelve dengue 3-, nine dengue 4-, four dengue 1- and seven dengue 2-infected patients and 25 dengue-negative sera (10 sera from patients infected with influenza virus, 10 sera from patients infected with Leptospira spp. as well as 5 sera from healthy individuals), and supernatants were collected daily. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages displaying H antibody fragment were added to the plates. Bound phages were detected with an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. The black line represents twice the mean value of the negative controls (supernatants from non-inoculated cells)
Anti-Den-4 phage-displayed antibody fragment M was tested with the same panel (Fig. 5). Virus-containing supernatants from all Den-4 serum-inoculated cells (serum viral titers from 40 to 3.8 × 104 pfu/ml) were positive by phage ELISA at day 5 postinoculation and later. Most of them (6/9) were positive from 2 to 3 days postinoculation onward. In these cases, IFA was also positive starting on day 3 (Fig. 6a, b). For some sera (2/6), IFA was weakly positive on day 3 (less than three stained cells) and strongly positive on day 7 (Fig. 6c, d). However, supernatants from these serum-inoculated cells became highly positive by phage ELISA on the third day postinoculation. The absence of undesired serotype cross-reactivities with anti-Den-4 phage ELISA was also confirmed with a diverse serum panel in the same way as for the anti-Den-3 assay (Fig. 5).
Dengue 4 virus detection by phage ELISA in supernatants from cells inoculated with patients’ sera. C6/36 HT cells were inoculated with a panel of acute-phase serum specimens from nine dengue 4-, twelve dengue 3-, four dengue 1- and seven dengue 2-infected patients and 25 dengue-negative sera (10 sera from patients infected with influenza virus, 10 sera from patients infected with Leptospira spp. as well as 5 sera from healthy individuals), and supernatants were daily collected. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages displaying M antibody fragment were added to the plates. Bound phages were detected with an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. The black line represents twice the mean value of the negative controls (supernatants from non-inoculated cells)
Indirect immunofluorescence assay (IFA) of dengue 4 serum-inoculated C6/36 HT cells. Viral particles were detected with Den-4 specific mouse monoclonal antibody 1H10-6-7 and an anti-mouse IgG conjugated to FITC. IFA results for serum 14-inoculated cells—collected 3 (a) and 7 (b) days postinoculation—and IFA results for serum 19-inoculated cells—collected 3 (c) and 7 (d) days postinoculation—are shown. Magnification 400×
All together, the above results indicate the usefulness of anti-Den-3 and anti-Den-4 phage-displayed antibody fragments for serotyping patients’ samples.
Comparison of phage-displayed and soluble single-chain antibody fragments
Supernatants from Den-3 and Den-4 serum-inoculated C6/36 HT cells were tested in parallel using C and M phage-displayed antibody fragments and their soluble scFv counterparts as detector reagents (Figs. 7, 8). Whereas supernatants from some serum-inoculated cells became positive as early as two days postinoculation when using phage-displayed antibody fragments, soluble scFvs were not able to detect virus particles in any of them at this time point. Even when soluble scFvs recognized virus in supernatants from serum-inoculated cells after three or more days of culture, the absorbances obtained for all samples were lower than those read with phage ELISA. The difference in detection sensitivity of the two formats was assessed by determining the minimum number of viral particles in the supernatant that could be detected. C and M phage-displayed antibody fragments were able to detect as little as 10 and 40 pfu/ml, respectively, in the supernatants, whereas C and M soluble scFvs detected minimal concentrations of 4 × 102 and 2.7 × 102 pfu/ml, respectively. These results indicate that our phage-displayed antibody fragments are more suitable than soluble scFvs for detecting and serotyping dengue virus.
Comparison of dengue 3 virus detection by phage-displayed and soluble C antibody fragment. Supernatants from twelve dengue 3 serum-inoculated C6/36 HT cells were tested in duplicate using phage-displayed (open triangle) and soluble scFv (open circle) antibody fragments as detector reagents. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages or soluble C antibody fragment were added to the plates. Bound phages were detected using an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. Bound soluble antibody fragments were detected using Mab 9E10, directed to the c-myc tag and an anti-mouse IgG antibody conjugated to horseradish peroxidase. Black lines represent twice the mean value of the negative controls (supernatants from non-inoculated cells)
Comparison of dengue 4 virus detection by phage-displayed and soluble M antibody fragment. Supernatants from nine dengue 4 serum-inoculated C6/36 HT cells were tested in duplicate using phage-displayed (open triangle) and soluble scFv (open circle) antibody fragments as detector reagents. Polystyrene plates coated with human anti-dengue IgG were incubated with supernatants. Diluted phages or soluble M antibody fragment were added to the plates. Bound phages were detected with an anti-M13 monoclonal antibody conjugated to horseradish peroxidase. Bound soluble antibody fragments were detected using Mab 9E10 directed to the c-myc tag and an anti-mouse IgG antibody conjugated to horseradish peroxidase. Black lines represent twice the mean value of the negative controls (supernatants from non-inoculated cells)
Discussion
For many years, diagnosis of dengue infection during the acute phase of illness has relied on virus isolation and subsequent identification with serotype-specific Mabs by IFA and RNA detection. Viral isolation and identification by IFA is the gold standard for dengue virus serotype analysis [25] and is a highly specific and sensitive method. However, at least seven days of culture are required to confirm diagnosis and determine the infecting serotype [35]. RNA detection provides sensitive and more rapid diagnosis. It can be done using traditional nested RT-PCR [20] or the more recently described real-time RT-PCR assay [8]. Nevertheless, these techniques require specialized laboratory equipment and are not widely available in most hospital diagnostic laboratories. That is why several studies have focused on the search for other rapid, sensitive and specific laboratory tests for diagnosis and serotyping of dengue virus.
In the last few years, serology techniques have appeared as an alternative for early diagnosis using NS1 protein as antigen [19, 29, 30]. Some of these authors also proposed NS1 as a good serotyping marker using tests based on NS1 serotype-specific IgG and IgM [29, 30]. However, correct dengue virus serotyping in patients’ samples was not always possible due to the cross-reactivity of antibodies raised against the four serotypes. An antigen-capture ELISA to detect NS1 in acute-phase sera of dengue-virus-infected patients has also been reported [1, 39]. The use of polyclonal antibodies reduced the specificity of this assay since NS1 amino acid sequence identity among the four dengue serotypes is about 80%. Recently, the identification of a panel of Mabs against specific epitopes of NS1 from Den-1 virus was described [38]. A sandwich ELISA to detect Den-1 virus infection in acute-phase sera was developed using such antibodies.
Our approach combines the infection of cells with virus from patients’ samples (as routinely done for virus isolation) with detection of viral particles by ELISA in cell culture supernatants. Four anti-Den-3 fragments and one anti-Den-4 phage-displayed antibody fragment were evaluated as serotype-specific detector antibodies in ELISA. This study showed the usefulness of these recombinant antibodies for viral serotyping in patients’ samples.
Phage ELISA results were compared with those obtained by IFA. Serum-inoculated cultures that were positive by phage ELISA from 2 to 3 days postinoculation onward were also positive by IFA at day 3. Some of them that were hardly detected as positive by IFA at day 3, since less than three stained cells were observed, were clearly positive by phage ELISA. Moreover, in one case, IFA was negative at day 3, whereas supernatant taken at the same time was positive by phage ELISA using one of the antibody fragments as detector. Despite the high sensitivity of IFA, most authors report needing between 6 and 10 days to confirm virus identification by IFA [11, 35]. Phage ELISA could allow earlier dengue virus serotyping.
Despite the emergence of PCR techniques, which are sensitive and very rapid, viral isolation combined with IFA remains as the gold standard for dengue serotyping. The current work is aimed to simplify the second stage of this approach and make it faster, while keeping its advantages. It is possible to evaluate supernatant samples by ELISA starting from the second day postinoculation and to continue growing inoculated cells and repeating the evaluation until supernatants become positive. This allows a rapid diagnosis and serotyping as early as 48 h postinoculation for some samples and an extended evaluation period for sera with lower viral load. Virus isolation from inoculated cells after testing of supernatants could preserve virus isolates derived from different patients with distinct clinical manifestations for virological and molecular epidemiological studies. The ELISA technique allows the evaluation of hundreds of samples.
The fact that viral particles are amplified and detected in cell cultures inoculated with small volumes of serum prevents the competition between endogenous anti-dengue antibodies (during secondary infections) and coating antibodies, which could reduce assay sensitivity in other assays aimed at detecting virus directly in patients’ samples.
Recombinant antibody fragments have been successfully isolated using phage display technology [4, 23]. Different library-derived antibody formats (soluble scFv and Fab fragments, whole antibodies) have been used for viral diagnosis. For instance, soluble antibody fragments recognizing hantaviruses [28], potato leafroll virus [33] and influenza A virus [9] have been evaluated for routine diagnosis by immunoassay. More recently, phage-displayed antibody fragments have been used directly as tools for detecting hepatitis B core antigen via phage ELISA [32].
In the present study, phage-displayed antibody fragments were better tools for early diagnosis and serotyping of Den-3 and Den-4 viruses than their soluble scFv counterparts. The use of a secondary antibody specific for the pVIII major coat protein amplifies the signal in phage ELISA because of the presence of 2700 copies of pVIII per M13 phage particle [31]. Whereas the interaction between the secondary antibody and the multiple copies of pVIII distributed along the large phage particle has been reported to be a disadvantage for immunocytochemical localization studies due to the diffuse images obtained [36], signal amplification in phage ELISA increased assay sensitivity without introducing undesired cross-reactivities. Since not all originally phage-displayed antibody fragments retain binding activity when expressed as soluble molecules [5], the possibility of using phages directly as diagnostic reagents is attractive.
In conclusion, the current work shows that anti-Den-3 and anti-Den-4 phage-displayed antibody fragments can be successfully used in the early detection and serotyping of dengue virus isolated from patients’ sera in less than one week (faster than identification by IFA). Future work should expand the availability of similar tools in order to detect each of the four serotypes. Further experiments with a larger panel of sera will be performed to validate this method as a routine diagnostic and serotyping procedure. Phage ELISA could then be used in a high-throughput way in order to identify in a short period of time the dengue virus serotypes that circulate in an endemic or non-endemic area. Such information is crucial for the management of patients and disease control.
References
Alcon S, Talarmin A, Debruyne M, Falconar A, Deubel V, Flamand M (2002) Enzyme-linked immunosorbent assay specific to dengue virus type 1 nonstructural protein NS1 reveals circulation of the antigen in the blood during the acute phase of disease in patients experiencing primary or secondary infections. J Clin Microbiol 40:376–381
Alvarez M, Rodriguez-Roche R, Bernardo L, Morier L, Guzman G (2005) Improved dengue virus plaque formation on BHK21 and LLCMK2 cells: evaluation of some factors. Dengue Bull 29:1–9
Alvarez M, Rodriguez-Roche R, Bernardo L, Vazquez S, Morier L, Gonzalez D, Castro O, Kouri G, Halstead SB, Guzman MG (2006) Dengue hemorrhagic fever caused by sequential dengue 1–3 virus infections over a long time interval: Havana epidemic, 2001–2002. Am J Trop Med Hyg 75:1113–1117
Barbas CF 3rd, Kang AS, Lerner RA, Benkovic SJ (1991) Assembly of combinatorial antibody libraries on phage surfaces: the gene III site. Proc Natl Acad Sci USA 88:7978–7982
Cabezas S, Rojas G, Pavon A, Alvarez M, Pupo M, Guillen G, Guzman MG (2008) Selection of phage-displayed human antibody fragments on dengue virus particles captured by a monoclonal antibody: application to the four serotypes. J Virol Methods 147:235–243
Calisher CH (2005) Persistent emergence of dengue. Emerg Infect Dis 11:738–739
Cantelar de Francisco N, Fernandez A, Albert Molina L, Perez Balbis E (1981) Survey of dengue in Cuba. 1978–1979. Rev Cubana Med Trop 33:72–78
de Oliveira Poersch C, Pavoni DP, Queiroz MH, de Borba L, Goldenberg S, dos Santos CN, Krieger MA (2005) Dengue virus infections: comparison of methods for diagnosing the acute disease. J Clin Virol 32:272–277
Desogus A, Burioni R, Ingianni A, Bugli F, Pompei R, Fadda G (2003) Production and characterization of a human recombinant monoclonal Fab fragment specific for influenza A viruses. Clin Diagn Lab Immunol 10:680–685
Gubler DJ (1998) Dengue and dengue hemorrhagic fever. Clin Microbiol Rev 11:480–496
Guzman MG, Kouri G (1996) Advances in dengue diagnosis. Clin Diagn Lab Immunol 3:621–627
Guzman MG, Kouri G (2003) Dengue and dengue hemorrhagic fever in the Americas: lessons and challenges. J Clin Virol 27:1–13
Guzman MG, Kouri G (2008) Dengue haemorrhagic fever integral hypothesis: confirming observations, 1987–2007. Trans R Soc Trop Med Hyg 102:522–523
Henchal EA, Gentry MK, McCown JM, Brandt WE (1982) Dengue virus-specific and flavivirus group determinants identified with monoclonal antibodies by indirect immunofluorescence. Am J Trop Med Hyg 31:830–836
Hermida C, Pupo M, Guzman MG, Gonzalez M, Marcet R (1992) Use of a dengue anti-complex monoclonal antibody in viral purification. Rev Cubana Med Trop 44:171–176
Köhler G, Milstein C (1975) Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256:52–53
Kouri G, Mas P, Guzman MG, Soler M, Goyenechea A, Morier L (1983) Dengue hemorrhagic fever in Cuba, 1981: rapid diagnosis of the etiologic agent. Bull Pan Am Health Organ 17:126–132
Kouri G, Guzman MG, Valdes L, Carbonel I, del Rosario D, Vazquez S, Laferte J, Delgado J, Cabrera MV (1998) Reemergence of dengue in Cuba: a 1997 epidemic in Santiago de Cuba. Emerg Infect Dis 4:89–92
Kumarasamy V, Wahab AH, Chua SK, Hassan Z, Chem YK, Mohamad M, Chua KB (2007) Evaluation of a commercial dengue NS1 antigen-capture ELISA for laboratory diagnosis of acute dengue virus infection. J Virol Methods 140:75–79
Lanciotti RS, Calisher CH, Gubler DJ, Chang GJ, Vorndam AV (1992) Rapid detection and typing of dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. J Clin Microbiol 30:545–551
Lorono Pino MA, Cropp CB, Farfan JA, Vorndam AV, Rodriguez Angulo EM, Rosado Paredes EP, Flores Flores LF, Beaty BJ, Gubler DJ (1999) Common occurrence of concurrent infections by multiple dengue virus serotypes. Am J Trop Med Hyg 61:725–730
Marks JD, Hoogenboom HR, Bonnert TP, McCafferty J, Griffiths AD, Winter G (1991) By-passing immunization. Human antibodies from V-gene libraries displayed on phage. J Mol Biol 222:581–597
McCafferty J, Griffiths AD, Winter G, DJ C (1990) Phage antibodies: filamentous phage displaying antibody variable domains. Nature 348:552–554
Morens DM, Halstead SB, Repik PM, Putvatana R, Raybourne N (1985) Simplified plaque reduction neutralization assay for dengue viruses by semimicro methods in BHK-21 cells: comparison of the BHK suspension test with standard plaque reduction neutralization. J Clin Microbiol 22:250–254
PAHO (1994) Dengue and dengue hemorrhagic fever in the Americas: guidelines for prevention and control.Scientific publication no.548. PAHO, Washington
Rodriguez-Roche R, Alvarez M, Guzman MG, Morier L, Kouri G (2000) Comparison of rapid centrifugation assay with conventional tissue culture method for isolation of dengue 2 virus in C6/36-HT cells. J Clin Microbiol 38:3508–3510
Rosario D, Alvarez M, Vazquez S, Amin N, Rodriguez-Roche R, Guzman MG (2001) Application of molecular method to the diagnosis and characterization of a dengue outbreak in Cuba. Biotecnologia Aplicada 18:203–206
Salonen EM, Parren PW, Graus YF, Lundkvist A, Fisicaro P, Vapalahti O, Kallio-Kokko H, Vaheri A, Burton DR (1998) Human recombinant Puumala virus antibodies: cross-reaction with other hantaviruses and use in diagnostics. J Gen Virol 79(Pt 4):659–665
Shu PY, Chen LK, Chang SF, Yueh YY, Chow L, Chien LJ, Chin C, Yang HH, Lin TH, Huang JH (2002) Potential application of nonstructural protein NS1 serotype-specific immunoglobulin G enzyme-linked immunosorbent assay in the seroepidemiologic study of dengue virus infection: correlation of results with those of the plaque reduction neutralization test. J Clin Microbiol 40:1840–1844
Shu PY, Chen LK, Chang SF, Su CL, Chien LJ, Chin C, Lin TH, Huang JH (2004) Dengue virus serotyping based on envelope and membrane and nonstructural protein NS1 serotype-specific capture immunoglobulin M enzyme-linked immunosorbent assays. J Clin Microbiol 42:2489–2494
Smith GP, Petrenko VA (1997) Phage Disp. Chem Rev 97:391–410
Tan GH, Yusoff K, Seow HF, Tan WS (2007) A phage-displayed single chain variable fragment that interacts with hepatitis B core antigen: library construction, selection and diagnosis. J Clin Virol 38:49–56
Toth R, Harper K, Mayo M, Torrance L (1999) Fusion proteins of single-chain variable fragments derived from phage dispaly libraries are effective reagents for routine diagnosis of potato leafroll virus infection in potato. Phytopathology 89:1015–1021
Vazquez S, Valdes O, Pupo M, Delgado I, Alvarez M, Pelegrino JL, Guzman MG (2003) MAC-ELISA and ELISA inhibition methods for detection of antibodies after yellow fever vaccination. J Virol Methods 110:179–184
Vorndam AV, Kuno G (1997) Laboratory diagnosis of dengue virus infections. In: Gubler D, Kuno G (eds) Dengue and dengue hemorrhagic fever. CAB International, Wallingford, pp 313–334
Willats WG (2002) Phage display: practicalities and prospects. Plant Mol Biol 50:837–854
Williamson RA, Burioni R, Sanna PP, Partridge LJ, Barbas CF, Burton DR (1993) Human monoclonal antibodies against a plethora of viral pathogens from single combinatorial libraries. Proc Natl Acad Sci USA 90:4141–4145
Xu H, Di B, Pan YX, Qiu LW, Wang YD, Hao W, He LJ, Yuen KY, Che XY (2006) Serotype 1-specific monoclonal antibody-based antigen capture immunoassay for detection of circulating nonstructural protein NS1: implications for early diagnosis and serotyping of dengue virus infections. J Clin Microbiol 44:2872–2878
Young PR, Hilditch PA, Bletchly C, Halloran W (2000) An antigen capture enzyme-linked immunosorbent assay reveals high levels of the dengue virus protein NS1 in the sera of infected patients. J Clin Microbiol 38:1053–1057
Acknowledgments
We thank Yamira Caballero (Tropical Medicine Institute ¨Pedro Kourí¨) for technical assistance in cell culture and Professor Virginia Capó (Tropical Medicine Institute “Pedro Kourí”) for processing of IFA results. This investigation received financial support from the Cuban Program for Dengue Vaccine Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cabezas, S., Rojas, G., Pavon, A. et al. Phage-displayed antibody fragments recognizing dengue 3 and dengue 4 viruses as tools for viral serotyping in sera from infected individuals. Arch Virol 154, 1035–1045 (2009). https://doi.org/10.1007/s00705-009-0401-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-009-0401-1