Abstract
Despite the growing number of therapies that target cancer-specific pathways, cytotoxic treatments remain important clinical tools. The rationale for targeting cell proliferation by chemotherapeutic agents stems from the assumption that tumours harbour a greater fraction of actively dividing cells than normal tissues. One such group of cytotoxic drugs impair microtubule polymers, which are cytoskeletal components of cells essential for many processes including mitosis. However, in addition to their antimitotic action, these agents cause debilitating and dose-limiting neurotoxicity because of the essential functions of microtubules in neurons. To overcome this limitation, drugs against mitosis-specific targets have been developed over the past decade, albeit with variable clinical success. Here we review the key lessons learnt from antimitotic therapies with a focus on inhibitors of microtubule motor proteins. Furthermore, based on the cancer genome data, we describe a number of motor proteins with tumour type-specific alterations, which warrant further investigation in the quest for cytotoxic targets with increased cancer specificity.
Similar content being viewed by others
Main
Cell proliferation remains a fundamental feature of all tumours. Proliferating cells adhere to a strictly ordered cell cycle, whereby growth phases are interspersed with S-phase when DNA replication takes place and mitosis when nuclear and cytoplasmic division occurs. Orderly transition through these events is mediated by checkpoints that assess whether conditions are suitable for cell cycle progression. If a checkpoint cannot be satisfied, the cell cycle is stalled to resolve the issue, and when this is not feasible cells senesce or die.
A particularly vulnerable phase of the cell cycle is mitosis, the process responsible for the equal partitioning of the duplicated genome of a dividing cell into two daughter cells. The most recognisable feature of mitotic cells is the bipolar spindle, a multi-molecular machine that capture, align and separate the sister chromatid pairs. The mitotic spindle is composed of sliding microtubule polymers, intrinsically polar structures with relatively stable minus ends and dynamic plus ends, which undergo rapid polymerisation and depolymerisation. The plus ends of spindle microtubules emanate into the cytoplasm to facilitate microtubule-mediated chromosome capture, whereas the minus ends are focussed at the two spindle poles formed by centrosomes. The act of centrosome separation at the onset of mitosis is an important determinant of bipolar spindle formation. The spindle assembly checkpoint coordinates mitotic events by delaying sister chromatid separation and cell cleavage until all chromosomes are attached to microtubules emanating from opposite spindle poles (reviewed in Lara-Gonzalez et al, (2012)). Once the checkpoint is satisfied, rapid activation of the ubiquitin ligase, anaphase-promoting complex, triggers proteasome-dependent sister chromatid separation and destruction of cyclin B, the activating subunit of the mitotic kinase, cyclin-dependent kinase 1 (CDK1; reviewed in Sivakumar and Gorbsky (2015)). Sister chromatids are then pulled towards the spindle poles, followed by cleavage furrow formation and ingression, culminating in the physical separation of cells during cytokinesis. Extra- or intracellular stresses can elicit chronic activation of the spindle assembly checkpoint. This can trigger cell death within mitosis, but cells can also exit mitosis without cytokinesis in a process called mitotic slippage, which is caused by progressive degradation of cyclin B during mitotic arrest (Brito and Rieder, 2006).
Antimitotic therapies in cancer
Microtubules and their dynamic behaviour are essential for multiple steps in mitosis and as such represent good antimitotic targets. Indeed, plants have long been mixing their own cocktails of microtubule poisons to combat insects. It is perhaps not a coincidence that these compounds, which include the vinca alcaloids from Madagascar periwinkle and the yew tree-derived taxanes (e.g., paclitaxel and docetaxel), show excellent clinical efficacy in several tumour types. At low concentrations, paclitaxel suppresses the dynamic behaviour of microtubules, whereas at higher concentrations, it promotes polymerisation (Schiff et al, 1979; Jordan et al, 1993; Jordan and Wilson, 2004).
In dividing cells, paclitaxel impairs mitotic spindle function, causing a spindle assembly checkpoint-mediated mitotic arrest. Much focus has been placed on the mechanism of paclitaxel-induced cell death over the past few years. Briefly, these studies intimate a surprising degree of variation in apoptotic response both between cell lines and individual cells (Gascoigne and Taylor, 2008). In fact, the fate of individual cells seems stochastic; cells may die from mitosis or undergo mitotic slippage followed by cell cycle arrest or apoptosis, and some even survive and enter the next cell cycle (Shi et al, 2008; Gascoigne and Taylor, 2008). In most, but not all cell lines, cell death is mediated by caspases and, encouragingly, paclitaxel elicits greater apoptotic response in cancer than in untransformed cells (Brito and Rieder, 2009). These studies also reveal that the response depends on drug concentration, but not on the actual duration of mitotic arrest, arguing that chronic activation of the spindle assembly checkpoint is not essential for cell death. Despite decades of clinical use, the mechanism of action of paclitaxel in tumours is poorly understood. Recent studies have employed time-lapse microscopy to compare the effects of taxanes on cancer cells in culture and their corresponding subcutaneous xenografts in mice (Orth et al, 2011; Janssen et al, 2013). Intravital imaging revealed fewer mitotic cells, more mitotic slippage and less apoptosis in paclitaxel-treated tumours than cultured cells (Orth et al, 2011). Cells that undergo mitotic slippage following paclitaxel treatment displayed highly abnormal nuclei. In spite of containing plenty of cells with normal nuclear morphology, the number of mitotic cells plummeted in the xenografts 1 week after a single dose of paclitaxel (Orth et al, 2011). This raises the possibility that paclitaxel elicits an anti-proliferative effect even on cells that do not undergo mitosis during the time of peak drug concentration, although one cannot exclude that the effect is due to residual paclitaxel levels in the tumours. In another study, simultaneous imaging of mitosis and apoptosis in xenografts of docetaxel-treated animals revealed wide-scale drug-induced apoptosis in the tumour without an apparent increase in the mitotic index (Janssen et al, 2013). Collectively, these reports indicate that mitosis-independent function(s) of taxanes contribute to their overall antitumour efficacy. Whether this mechanism is cell intrinsic or acts on the tumour microenvironment such as the vasculature remains to be seen (Jordan and Wilson, 2004; Orth et al, 2011). As simultaneous disruption of multiple microtubule-dependent processes is likely to make a major contribution to the clinical benefit of paclitaxel, it is crucial to gain a better understanding of the impact of paclitaxel on interphase cells.
Microtubule poisons have poorly tolerated side effects such as myelosuppression and peripheral neuropathy (Jordan and Wilson, 2004). Although the former is due to antimitotic action in the hematopoietic system, and is largely reversible, the neuropathy that results from inhibition of essential neuron-specific roles of microtubules is permanent. To overcome neurotoxicity, much effort has been invested in developing mitosis-specific drugs. The two main classes of antimitotic therapies are compounds that (i) target mitotic kinases and (ii) impede mitosis-specific microtubule functions through inhibiting motor proteins (reviewed in Salmela and Kallio (2013)).
Mitotic kinases are the master regulators of mitosis (for detailed review, see Malumbres (2011)). They control entry and exit from mitosis, along with the vast structural changes that accompany mitosis. Cyclin-dependent kinase 1 activity is essential for entry into mitosis, and its inactivation by cyclin B destruction marks mitotic exit. Owing to its critical roles in organisms, complete inhibition of CDK1 is expected to be highly toxic; nonetheless there are pan CDK inhibitors in clinical trials that target CDK1 activity (summarised in Asghar et al (2015)). Other important mitotic kinases are the Aurora-A and Plk1 kinases, which promote CDK1 activation and also regulate spindle assembly and chromosome alignment. Aurora-B is involved in chromosome capture and spindle assembly checkpoint, but along with Plk1 it is also essential for cytokinesis. Although blocking the activity of these kinases disrupts mitosis in cultured cells, the same agents have shown limited efficacy in numerous clinical trials conducted over the past decade (reviewed in Salmela and Kallio (2013)). None of the compounds have been licensed for clinical use so far, albeit inhibitors of Aurora-A and Plk1 have recently reached phase III trials in haematological malignancies. There are several possibilities to explain the rather disappointing performance of these drugs in solid cancers, of which we highlight a few: (i) narrow therapeutic window because of dose-limiting toxicities, (ii) lack of biomarkers for patient stratification, (iii) poor compound specificity or uptake and (iv) lack of sensitivity as a result of low-proliferation rate and too few mitotic cells in solid tumours (Mitchison, 2012).
Another group of mitosis-specific targets are the kinesin (KIF) family of microtubule motors (for detailed review, see Vicente and Wordeman (2015)). So far, 45 KIF genes have been identified in mammals and these have been divided into 14 families based on structure (kinesin-1 to -14). All KIF proteins contain a globular motor domain and a tail domain, the latter being responsible for interactions with specific cargos and adaptor proteins. The relative position of the motor domain determines the directionality of KIFs: those with N- or C-terminal motor domains exhibit plus end- and minus end-directed motility, respectively, whereas those with a central motor domain utilise ATP for microtubule depolymerisation. Although there is some functional redundancy between members of the KIF family, mutations of single KIFs can cause developmental abnormalities both in mice and humans (reviewed in Hirokawa and Tanaka (2015)). Functional redundancy between KIFs can be a double-edged sword at the clinic; it can cause resistance to therapies, but it has also the potential to reduce neuron-related side effects. Kinesins are essential for transporting cargo such as membrane vesicles, organelles and RNA molecules along microtubules in an ATP-dependent manner. They also slide and cross-link microtubules, functions that contribute to almost every aspect of mitosis including spindle assembly and organisation, chromosome capture, alignment and cytokinesis.
In this review, we discuss the current standing of KIF inhibitors at the clinic and discuss the pros and cons of their use in cancer treatment. Moreover, our analysis of publicly available cancer genome data sets reveals tumour type-specific genome alterations in a number of KIFs, several of which have received little or no attention in cancer-related research to date.
The history and clinical performance of Eg5 inhibitors
The career of KIF-targeting antimitotics began in the late 1990s with the screen of a panel of cell-permeable small molecules, already known to be cytotoxic in multiple NCI-60 cell lines, for their ability to induce mitotic arrest (Mayer et al, 1999). One hit produced a peculiar phenotype, mitotic cells stalled in prometaphase with monoastral spindles, which was reminiscent of the phenotype seen in HeLa cells following microinjection with anti-Eg5 antibodies (Blangy et al, 1995). Eg5/KIF11 is crucial for centrosome separation and thus bipolar spindle formation in human cells. As a homotetramer with motor domains at both ends, it cross-links and slides antiparallel microtubules apart (Kapitein et al, 2005). Subsequently, it was demonstrated that the compound identified, aptly termed monastrol, is indeed a reversible, allosteric inhibitor of Eg5, which blocks the catalytic cycle of the motor by interfering with the release of ADP (Maliga et al, 2002). Crucially, unlike microtubule poisons, monastrol did not appear to perturb cytoskeletal organisation in interphase cells.
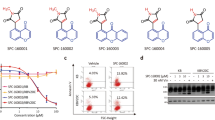
Whereas monastrol itself was neither potent nor sufficiently drug like to qualify as a therapeutic candidate, its discovery raised hope of finding clinically useful mitosis-specific compounds. Subsequently, multiple synthetic and natural small-molecule libraries were screened in search for drugs that inhibited Eg5. The first Eg5 inhibitor to enter clinical trials was ispinesib/SB-715992, one in a series of quinazolinone derivatives patented by Cytokinetics. Between 2003 and 2010, ispinesib was evaluated as a single agent or combination drug in 16 phase I/II trials for advanced leukaemia, lymphomas and solid tumours (reviewed in Rath and Kozielski, (2012); Salmela and Kallio (2013)). The drug displayed acceptable safety and tolerability profile, with neutropenia being the most frequent side effect; however, results were largely limited to disease stabilisation, with partial response in a few breast cancer patients (Gomez et al, 2012). Owing to poor clinical efficacy, none of these trials progressed to phase III, and development of ispinesib was suspended.
Ispinesib was followed by a number of new candidates, some sharing a similar chemical scaffold (e.g., SB-743921 or AZD4877), whereas others being structurally unrelated like litronesib and filanesib/ARRY-520 (Rath and Kozielski, 2012). Although all compounds exhibited antitumour activity in xenograft models, they have shown limited clinical efficacy in advanced solid tumours and relapsed/refractory lymphomas, with stable disease being the best tumour response achieved (Salmela and Kallio, 2013; Lorusso et al, 2015). As a combination therapy with proteasome inhibitors, filanesib elicited remarkable objective responses in pre-treated multiple myeloma (MM) patients and will become the first KIF inhibitor to reach phase III for the treatment of relapsed/refractory MM (Shah et al, 2013).
Lessons from the past–looking to the future: KIF inhibitors
Eg5 inhibitors are still being evaluated in clinical trials, but it is fair to say that they have not fulfilled their original promise. They have, however, taught us a number of valuable lessons for future development of antimitotic therapies.
First, choosing the right intensity of treatment could be pivotal. Eg5 inhibitors tested in the clinic act reversibly on their target, and thus mitotic arrest must be maintained long enough to elicit cell death. Moreover, as these drugs act only on cells that enter mitosis, prolonged exposure maximises number of cells affected by treatment, and thus sustained plasma levels are likely to be essential for clinical efficacy. Indeed, from published phase I studies, it appears that single-dose regimens were replaced by more frequent administration schedules, and continuous dosing of orally available drugs may be the way forward.
Second, patient stratification on the basis of predictive biomarkers is another key to improved outcomes. MM patients with low serum levels of alpha-1 acid glycoprotein, an acute-phase protein capable of binding to and reducing the availability of filanesib, have been shown to benefit more from treatment with the inhibitor (Lonial et al, 2013). In bladder cancer cell lines, high expression of p63 was found to be a positive predictor of response to AZD4877 (Marquis et al, 2012). Proliferation rate within the tumour may also be relevant as a predictive parameter, as antimitotic therapies can only eliminate cells that enter mitosis during treatment.
Third, in the case of Eg5, appropriate drug combinations need to be devised to combat resistance. Although, the role for Eg5 in bipolar spindle formation has long been considered essential and non-redundant, recent studies have reported a range of drug resistance mechanisms. For instance, cancer cells with overactive EGFR pathway display reduced dependence on Eg5 for bipolar spindle formation and, hence, reduced susceptibility to Eg5 inhibition (Mardin et al, 2013). Therefore, simultaneous suppression of EGFR could increase the antimitotic effect of Eg5 inhibitors in such tumours. Another potential source of resistance is the expression of KIF15, a KIF that becomes essential for spindle bipolarity when Eg5 activity is partially blocked (Tanenbaum et al, 2009). Targeting KIF15 with Eg5 could therefore elicit greater antitumour response. Moreover, vinblastine, a vinca alkaloid that depolymerises microtubules, showed strong synergy with ispinesib in a mouse model of triple negative breast cancer (Brandl et al, 2014).
There are several KIFs with putative roles in cancer, but to date only a handful of inhibitors has been developed (summarised in Rath and Kozielski (2012)). Of these, inhibitors of the centromere-associated protein E (CENP-E) are at the most advanced stage of development. CENP-E is a plus end-directed KIF with vital roles in chromosome alignment and congression (Yen et al, 1991). GSK923295, an allosteric inhibitor of CENP-E, prevents CENP-E motility, thereby causing chromosome congression defects, mitotic arrest and tumour regression in xenograft models (Wood et al, 2010). In a phase I clinical trial, however, GSK923295 elicited partial response in only 1 of 39 patients with refractory cancers (Chung et al, 2012). One reason why microtubule poisons have so far outperformed antimitotics at the clinic could be their ability to kill not only mitotic but also interphase/quiescent cells in the tumour and/or in its microenvironment. Thus, motor proteins that have both interphase and mitotic roles may be more attractive targets than mitosis-specific ones, especially if we can identify ones with non-essential neuronal functions.
KIFC1, a KIF with a putative tumour-specific function
Abnormal multipolar mitoses in cancer cells were described by von Hansemann in 1890, prompting Boveri’s hypothesis on a causative link between abnormal mitoses and malignant tumours in 1914. Bipolar spindle formation is facilitated by a tightly controlled centrosome duplication cycle, which ensures that cells have precisely two centrosomes when entering mitosis (Firat-Karalar and Stearns, 2014). A common cause of spindle multipolarity is the presence of extra centrosomes in cells. Centrosome amplification has been documented in many types of solid and haematological malignancies, and was recently shown to contribute to cellular invasion (Chan, 2011; Godinho et al, 2014). This raises the question as to how tumour cells survive with supernumerary centrosomes, considering that multipolar cell division is expected to cause catastrophic missegregation of chromosomes, and consequently cell death. As it happens, cancer cells can evade multipolar cell division by clustering extra centrosomes into pseudo-bipolar spindle poles that facilitate a normal bipolar cell division, albeit at a cost of low-level chromosome missegregation (reviewed in Marthiens et al (2012) and Godinho and Pellman (2014)).
A key factor in centrosome clustering is KIFC1, also known as HSET, a member of the KIF-14 family of minus end-directed microtubule motor proteins. KIFC1 crosslinks and slides microtubules, thereby producing forces that aid clustering of supernumerary centrosomes (reviewed in Marthiens et al (2012)). By contrast, in cells with normal centrosome complement, KIFC1 is dispensable for bipolar spindle formation, and thus represents an antimitotic target specific for tumour types with a high incidence of centrosome amplification. It is therefore timely to identify tumour types that could benefit from anti-KIFC1 therapy.
Survey of cancer-specific genomic alterations in KIFs
The microtubule motor proteins selected as putative cancer targets were chosen due to their perceived essential roles in mitosis (i.e., Eg5 and CENP-E). Although it is not a prerequisite for a putative drug target to show alterations on the genomic level, we wondered whether there was any evidence for genomic alterations in KIF genes in human cancers. If so, these might reveal potential oncogenic or tumour-suppressor roles of KIFs, or serve as biomarkers for patient stratification. To this end, we searched for mutations, amplifications and deletions in human KIF genes in The Cancer Genome Atlas (TCGA) database and used cBioPortal (http://cbioportal.org) for analysing this multidimensional data. For the purpose of this review, we probed 43 of 45 KIFs (KIF16A and KIF19B are not annotated) in studies with a cohort size of at least 100 patients.
We have found somatic mutations in a number of KIFs, in particular in endometrial cancer, lung squamous cell carcinoma and melanoma. However, these are unique to single samples and distributed evenly through the protein sequence, and therefore their biological significance is difficult to assess. By contrast, we have identified 10 KIF genes that are amplified in at least 10% of cases in one or more cancers, and 7 of these showed good correlation between mRNA expression and copy number alterations in specific tumour types (Table 1). KIF14, a KIF essential for cytokinesis, is amplified in ∼10% of liver, breast and lung adenocarcinomas, confirming earlier reports that it might be a putative oncogene in these very tumour types (Corson et al, 2005). Moreover, KIF14 modulates sensitivity to taxanes in a breast cancer cell line, and its expression negatively correlates with relapse-free survival in breast cancer (Singel et al, 2013). Another candidate from our screen is KIF5A, a neuron-specific KIF with amplification seen in ∼10% of glioblastomas. Indeed, a recent report has identified KIF5A as a putative driver gene in glioblastoma using the same TCGA data set (Ping et al, 2015). In breast cancer, overexpression of KIF5A correlates with taxol resistance (De et al, 2009). Our analysis has highlighted further KIFs such as KIFC2 with over 30% amplification in ovarian cancer, or KIF3A, KIF4B and KIF13A each with over 10% of amplification in at least one tumour type, and yet we know very little of their cellular roles that could be relevant to tumourigenesis.
Deletions in KIF genes seem less frequent than amplifications in cancers. Of these, the most prominent ones are homozygous deletions of KIF9 and KIF15 genes that co-occur in 12% of renal clear cell carcinomas. Although KIF9 function has not been characterised in epithelial cells, KIF15 can promote spindle bipolarity when Eg5 activity is partially blocked (Tanenbaum et al, 2009). The partial redundancy between Eg5 and KIF15 may contribute to resistance to anti-Eg5 therapies, and so the prevalence of KIF15 deletion in this sub-group of renal cancer patients could sensitize these tumours to Eg5 inhibitors. Another interesting example is KIF1A, deleted in ∼7% of sarcomas. This KIF is silenced through promoter methylation in certain tumour types, raising the possibility that it has antitumour activity (Guerrero-Preston et al, 2014).
While mining the TCGA data set we noted that amplifications were rare (<5%) of the genes encoding Eg5 and the mitotic kinases CDK1, Aurora-B and Plk1, although Aurora-A amplification was seen ∼10% in colorectal and ovarian cancers. As we focused our analysis solely on mutations, amplifications and deletions of KIF genes, it is not surprising that not all KIFs with reported tumour-related functions have been identified in our screen (Rath and Kozielski, 2012). Moreover, there seems to be limited overlap between our survey of KIF genes in the TCGA database and previously published KIF expression profiles in tumours (summarised in Rath and Kozielski (2012)). This is likely to arise from differences in the methodologies; our analysis focused exclusively on tumours that carry copy number alterations and concomitant changes in RNA levels of KIFs, whereas previously published studies assayed KIF levels by immunohistochemistry and to a lesser extent by RNA expression. Nevertheless, these studies collectively argue that there are significant changes in the expression levels of several KIFs in a variety of cancer types. It is therefore vital to establish if amplifications of KIF genes translate into elevated protein levels in the respective tumours.
Conclusions
Antimitotics have had limited success at clinical trials so far, but better understanding of dosing and drug resistance, together with the use of combination therapies, have the potential to improve their efficacy. Our analysis has highlighted a number of KIFs with altered expression profiles in several different cancer types. Amplifications were seen in 10–30% of patient samples, which could indicate pro-tumorigenic potential and cancer-specific roles of these motors, calling for further investigations in preclinical models. What the future holds for inhibitors of KIFs in cancer treatment, and whether they can eventually beat plant-derived microtubule poisons at the clinic, will depend largely on whether suitable targets can be identified for specific tumour types.
References
Asghar U, Witkiewicz AK, Turner NC, Knudsen ES (2015) The history and future of targeting cyclin-dependent kinases in cancer therapy. Nat Rev Drug Discov 14: 130–146.
Blangy A, Lane HA, D'herin P, Harper M, Kress M, Nigg EA (1995) Phosphorylation by p34cdc2 regulates spindle association of human Eg5, a kinesin-related motor essential for bipolar spindle formation in vivo. Cell 83: 1159–1169.
Brandl MB, Pasquier E, Li F, Beck D, Zhang S, Zhao H, Kavallaris M, Wong ST (2014) Computational analysis of image-based drug profiling predicts synergistic drug combinations: applications in triple-negative breast cancer. Mol Oncol 8: 1548–1560.
Brito DA, Rieder CL (2006) Mitotic checkpoint slippage in humans occurs via cyclin B destruction in the presence of an active checkpoint. Curr Biol 16: 1194–1200.
Brito DA, Rieder CL (2009) The ability to survive mitosis in the presence of microtubule poisons differs significantly between human nontransformed (RPE-1) and cancer (U2OS, HeLa) cells. Cell Motil Cytoskeleton 66: 437–447.
Chan JY (2011) A clinical overview of centrosome amplification in human cancers. Int J Biol Sci 7: 1122–1144.
Chung V, Heath EI, Schelman WR, Johnson BM, Kirby LC, Lynch KM, Botbyl JD, Lampkin TA, Holen KD (2012) First-time-in-human study of GSK923295, a novel antimitotic inhibitor of centromere-associated protein E (CENP-E), in patients with refractory cancer. Cancer Chemother Pharmacol 69: 733–741.
Corson TW, Huang A, Tsao MS, Gallie BL (2005) KIF14 is a candidate oncogene in the 1q minimal region of genomic gain in multiple cancers. Oncogene 24: 4741–4753.
De S, Cipriano R, Jackson MW, Stark GR (2009) Overexpression of kinesins mediates docetaxel resistance in breast cancer cells. Cancer Res 69: 8035–8042.
Firat-Karalar EN, Stearns T (2014) The centriole duplication cycle. Philos Trans R Soc Lond B Biol Sci 369.
Gascoigne KE, Taylor SS (2008) Cancer cells display profound intra- and interline variation following prolonged exposure to antimitotic drugs. Cancer Cell 14: 111–122.
Godinho SA, Pellman D (2014) Causes and consequences of centrosome abnormalities in cancer. Philos Trans R Soc Lond B Biol Sci 369.
Godinho SA, Picone R, Burute M, Dagher R, Su Y, Leung CT, Polyak K, Brugge JS, Thery M, Pellman D (2014) Oncogene-like induction of cellular invasion from centrosome amplification. Nature 510: 167–171.
Gomez HL, Philco M, Pimentel P, Kiyan M, Monsalvo ML, Conlan MG, Saikali KG, Chen MM, Seroogy JJ, Wolff AA, Escandon RD (2012) Phase I dose-escalation and pharmacokinetic study of ispinesib, a kinesin spindle protein inhibitor, administered on days 1 and 15 of a 28-day schedule in patients with no prior treatment for advanced breast cancer. Anticancer Drugs 23: 335–341.
Guerrero-Preston R, Hadar T, Ostrow KL, Soudry E, Echenique M, Ili-Gangas C, Perez G, Perez J, Brebi-Mieville P, Deschamps J, Morales L, Bayona M, Sidransky D, Matta J (2014) Differential promoter methylation of kinesin family member 1a in plasma is associated with breast cancer and DNA repair capacity. Oncol Rep 32: 505–512.
Hirokawa N, Tanaka Y (2015) Kinesin superfamily proteins (KIFs): various functions and their relevance for important phenomena in life and diseases. Exp Cell Res 334: 16–25.
Janssen A, Beerling E, Medema R, Van Rheenen J (2013) Intravital FRET imaging of tumor cell viability and mitosis during chemotherapy. PLoS One 8: e64029.
Jordan MA, Toso RJ, Thrower D, Wilson L (1993) Mechanism of mitotic block and inhibition of cell proliferation by taxol at low concentrations. Proc Natl Acad Sci USA 90: 9552–9556.
Jordan MA, Wilson L (2004) Microtubules as a target for anticancer drugs. Nat Rev Cancer 4: 253–265.
Kapitein LC, Peterman EJ, Kwok BH, Kim JH, Kapoor TM, Schmidt CF (2005) The bipolar mitotic kinesin Eg5 moves on both microtubules that it crosslinks. Nature 435: 114–118.
Lara-Gonzalez P, Westhorpe FG, Taylor SS (2012) The spindle assembly checkpoint. Curr Biol 22: R966–R980.
Lonial S, Shah JJ, Zonder J, Bensinger WI, Cohen AD, Kaufman JL, Nooka AK, Weber DM, Hilder B, Rush SA, Ptaszynski A, Walker D, Orlowski RZ (2013) Prolonged survival and improved response rates with ARRY-520 in relapsed/refractory multiple myeloma (RRMM) patients with low α-1 acid glycoprotein (AAG) levels: results from a phase 2 study. Blood 122: 285.
Lorusso PM, Goncalves PH, Casetta L, Carter JA, Litwiler K, Roseberry D, Rush S, Schreiber J, Simmons HM, Ptaszynski M, Sausville EA (2015) First-in-human phase 1 study of filanesib (ARRY-520), a kinesin spindle protein inhibitor, in patients with advanced solid tumors. Invest New Drugs 33: 440–449.
Maliga Z, Kapoor TM, Mitchison TJ (2002) Evidence that monastrol is an allosteric inhibitor of the mitotic kinesin Eg5. Chem Biol 9: 989–996.
Malumbres M (2011) Physiological relevance of cell cycle kinases. Physiol Rev 91: 973–1007.
Mardin BR, Isokane M, Cosenza MR, Kramer A, Ellenberg J, Fry AM, Schiebel E (2013) EGF-induced centrosome separation promotes mitotic progression and cell survival. Dev Cell 25: 229–240.
Marquis L, Tran M, Choi W, Lee IL, Huszar D, Siefker-Radtke A, Dinney C, Mcconkey DJ (2012) p63 expression correlates with sensitivity to the Eg5 inhibitor ZD4877 in bladder cancer cells. Cancer Biol Ther 13: 477–486.
Marthiens V, Piel M, Basto R (2012) Never tear us apart—the importance of centrosome clustering. J Cell Sci 125: 3281–3292.
Mayer TU, Kapoor TM, Haggarty SJ, King RW, Schreiber SL, Mitchison TJ (1999) Small molecule inhibitor of mitotic spindle bipolarity identified in a phenotype-based screen. Science 286: 971–974.
Mitchison TJ (2012) The proliferation rate paradox in antimitotic chemotherapy. Mol Biol Cell 23: 1–6.
Orth JD, Kohler RH, Foijer F, Sorger PK, Weissleder R, Mitchison TJ (2011) Analysis of mitosis and antimitotic drug responses in tumors by in vivo microscopy and single-cell pharmacodynamics. Cancer Res 71: 4608–4616.
Ping Y, Deng Y, Wang L, Zhang H, Zhang Y, Xu C, Zhao H, Fan H, Yu F, Xiao Y, Li X (2015) Identifying core gene modules in glioblastoma based on multilayer factor-mediated dysfunctional regulatory networks through integrating multi-dimensional genomic data. Nucleic Acids Res 43: 1997–2007.
Rath O, Kozielski F (2012) Kinesins and cancer. Nat Rev Cancer 12: 527–539.
Salmela AL, Kallio MJ (2013) Mitosis as an anti-cancer drug target. Chromosoma 122: 431–449.
Schiff PB, Fant J, Horwitz SB (1979) Promotion of microtubule assembly in vitro by taxol. Nature 277: 665–667.
Shah JJ, Feng L, Thomas SK, Weber DM, Wang M, Hilder B, Alexanian R, Orlowski RZ (2013) Phase 1 study of the novel kinesin spindle protein inhibitor ARRY-520+carfilzomib in patients with relapsed and/or refractory multiple myeloma. Blood 122: 1982.
Shi J, Orth JD, Mitchison T (2008) Cell type variation in responses to antimitotic drugs that target microtubules and kinesin-5. Cancer Res 68: 3269–3276.
Singel SM, Cornelius C, Batten K, Fasciani G, Wright WE, Lum L, Shay JW (2013) A targeted RNAi screen of the breast cancer genome identifies KIF14 and TLN1 as genes that modulate docetaxel chemosensitivity in triple-negative breast cancer. Clin Cancer Res 19: 2061–2070.
Sivakumar S, Gorbsky GJ (2015) Spatiotemporal regulation of the anaphase-promoting complex in mitosis. Nat Rev Mol Cell Biol 16: 82–94.
Tanenbaum ME, Macurek L, Janssen A, Geers EF, Alvarez-Fernandez M, Medema RH (2009) Kif15 cooperates with eg5 to promote bipolar spindle assembly. Curr Biol 19: 1703–1711.
Vicente JJ, Wordeman L (2015) Mitosis, microtubule dynamics and the evolution of kinesins. Exp Cell Res 334: 61–69.
Wood KW, Lad L, Luo L, Qian X, Knight SD, Nevins N, Brejc K, Sutton D, Gilmartin AG, Chua PR, Desai R, Schauer SP, Mcnulty DE, Annan RS, Belmont LD, Garcia C, Lee Y, Diamond MA, Faucette LF, Giardiniere M, Zhang S, Sun CM, Vidal JD, Lichtsteiner S, Cornwell WD, Greshock JD, Wooster RF, Finer JT, Copeland RA, Huang PS, Morgans DJ Jr., Dhanak D, Bergnes G, Sakowicz R, Jackson JR (2010) Antitumor activity of an allosteric inhibitor of centromere-associated protein-E. Proc Natl Acad Sci U S A 107: 5839–5844.
Yen TJ, Compton DA, Wise D, Zinkowski RP, Brinkley BR, Earnshaw WC, Cleveland DW (1991) CENP-E, a novel human centromere-associated protein required for progression from metaphase to anaphase. EMBO J 10: 1245–1254.
Acknowledgements
We thank members of the laboratory for the critical reading of the manuscript. Our work is funded by Cancer Research UK (C14303/A17197). We express our apology to all authors whose work could not be cited due to lack of space.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-Non-Commercial-Share Alike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Chandrasekaran, G., Tátrai, P. & Gergely, F. Hitting the brakes: targeting microtubule motors in cancer. Br J Cancer 113, 693–698 (2015). https://doi.org/10.1038/bjc.2015.264
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.264
Keywords
This article is cited by
-
MiR-19a/miR-96-mediated low expression of KIF26A suppresses metastasis by regulating FAK pathway in gastric cancer
Oncogene (2021)
-
Observations on spontaneous tumor formation in mice overexpressing mitotic kinesin Kif14
Scientific Reports (2018)
-
MYBL2 (B-Myb): a central regulator of cell proliferation, cell survival and differentiation involved in tumorigenesis
Cell Death & Disease (2017)
-
Upregulate KIF4A Enhances Proliferation, Invasion of Hepatocellular Carcinoma and Indicates poor prognosis Across Human Cancer Types
Scientific Reports (2017)
-
Forces and Disease: Electrostatic force differences caused by mutations in kinesin motor domains can distinguish between disease-causing and non-disease-causing mutations
Scientific Reports (2017)