INTRODUCTION
The outbreak of severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) disease, mostly called coronavirus disease-19 (COVID-19), has proven that new infectious diseases can spread in humans rapidly to pose a global public health challenge, especially where the containment of the disease is difficult (García de Abajo et al., 2020). This sudden outbreak of COVID-19 has surprised the vast majority of healthcare practitioners and scientists, who are working tirelessly to educate people and combat the pandemic (Rai et al., 2020). The SARS-CoV-2 is an enveloped positive-sense, single-stranded ribonucleic acid (RNA) virus belonging to the class of beta-coronaviruses (Anderson et al., 2020; Rahman et al., 2021). Severe Acute Respiratory Syndrome Corona Virus-1 (SARS-CoV-1) and Middle East Respiratory-Corona Virus (MERS-CoV) are endemic viruses that have previously wreaked havoc on human healthcare systems through animal-to-human, human-to-human, and, recently reported, human-to-animal transmissions making it spread quickly (Ayipo et al., 2021; Banik et al., 2015; Cleary et al., 2020). Currently, no approved antiviral drug is used to treat SARS-CoV and MERS-CoV infections, but the deployment of several effective vaccines against SARS-CoV-2 infection is in progress (Abubakar et al., 2020; Amanat and Krammer, 2020; Habas et al., 2020; Rahman et al., 2021). The SARS-CoV-1 and MERS-CoV are responsible for the epidemics of SARS in 2003 and MERS in 2012. The viruses are easily transmitted through droplets and air (Zhu et al., 2020). The effective and quick control of SARS-CoV-2 outbreaks can be achieved through the epidemiological knowledge of the disease, accurate viral detection, preventive strategies, and acceptable hygiene practices to decrease the risk of transmission. Although health practitioners in both developed and developing countries are overwhelmed with the pandemic, the need for a solid motivation to limit the spread and adopt future strategic plans for effective prevention remains necessary (Boyce and Pittet, 2002).
Viruses such as influenza, the common cold rhinovirus, and CoVs can be easily transmitted from an infected person to a healthy individual through coughing, sneezing, talking, and sometimes breathing (Asadi et al., 2020). Suggestively, these physiological actions produce aerosol droplets of various sizes and may carry infectious viruses that could initiate new infections, especially when inhaled by individuals (García de Abajo et al., 2020). The people at high risk of hospital-acquired infections such as SARS-CoV-2 are the healthcare professionals (HCPs) and emergency rescue workers (Wilson et al., 2020). This was evident from early reports of several HCPs infected from the origin of SARS-CoV-2, Wuhan, China (Wang et al., 2020a). Not only are these exposed HCPs at higher risk, but they are also potential carriers of the virus, especially those with closer contact with patients such as dentists, emergency physicians, and maxillofacial surgeons. Hence, there is a need for regular disinfection, decontamination, and proper sterilization techniques to prevent viral transmission (Krajewska et al., 2020; Peng et al., 2020).
One of the recommended practices for inactivating and removing pathogenic organisms from surfaces is disinfecting and sterilizing agents through stipulated procedures and protocols. Disinfection is a process of reducing virtually all recognizable pathogenic microorganisms using chemical agents only (Rai et al., 2020). Meanwhile, sterilization eliminates or destroys all microbial life forms by applying both chemicals and heat methods. Both sterilization methods at large are routinely carried out in healthcare facilities (Hassandarvish et al., 2020).
There are scientific guidelines and protocols for selecting and using disinfectants in hospitals, laboratories, homes, and public places. This is to minimize health risks and ensure the appropriate use of chemicals (Rutala et al., 2000). However, recently, due to the outbreak of COVID-19, there has been an upsurge in the indiscriminate use of alcohol- and iodine-based agents with no adherence to the stipulated guidelines and monitoring protocols for preventing and inactivating SARS-CoV-2 (McDonnell and Russell, 1999). This malpractice exposes humans to public health dangers and environmental hazards. It also has negative consequences on biodiversity due to the toxicological effects of such disinfectants (Agnelo et al., 2020; Nabi et al., 2020). Therefore, the excessive use of these antimicrobial agents has raised much public health and environmental concerns.
MATERIALS AND METHODS
Literature information was sourced from PubMed, ScienceDirect, Embase, MEDLINE, and China National Knowledge Infrastructure (CNKI) databases using Google Scholars and Free Full PDF as search engines. Articles written in the English language were retrieved and included in the study. This article discussed the physical and chemical countermeasures of microbial reduction agents and the prevention of CoVs, their potential toxicity, and safety to humans and the environment during the COVID-19 pandemic. Lastly, possible ways of developing drug resistance due to indiscriminate production and practices were highlighted.
DISINFECTANTS AND STERILIZING AGENTS
Disinfection is a process that eliminates many or all microorganisms from inanimate objects, whereas sterilization removes all microbes. Agents used to kill pathogenic microbes from inanimate objects or surfaces are called disinfectants, and those capable of destroying all microbes are sterilizing agents (Rutala and Weber, 2013; 2016).
Physical disinfectants and sterilant
Disinfectants that destroy pathogens utilizing physical agents such as heat, pressure, light, and irradiation are referred to as physical disinfection. These agents can directly damage microbes by various mechanisms such as damage to the cell membrane, deoxyribonucleic acid (DNA) or RNA, enzyme, or protein (Rutala and Weber, 2013; 2016).
Heat
Heat treatment is one of the simplest, widely used, most effective, and oldest methods. Heat can be applied in a hydrated (moist heat; 121°C–134°C) or dry state (160°C–180°C). Heat sterilization denatures or coagulates the protein or enzyme of the virus or cell, which causes the cell to die. Dry heat kills microbes through oxidative damage (Popat et al., 2010). Incineration, hot air oven, red heat, flaming, and infrared are examples of dry heat sterilization (Rutala and Weber, 2013; 2016). To supply heat, there are various methods as follows.
a. Solar
Solar energy can be used for disinfection. Several reactors are available that can convert energy from solar irradiation (Abraham et al., 2015). Ultraviolet (UV) and visible light inactivation is often used along with solar power and can be used alone, such as for black-box solar heaters or solar water heat exchangers. Light is not exposed to the media (Safapour and Metcalf, 1999). It is necessary to use a thermometer or indicator as sunlight may not supply enough heat (Ray and Jain, 2014).
b. Microwave
1–350 GHz is the lethal range of microwave for microbes, with deadly peak effects at 60 GHz (Fleming, 1944; Green et al., 1997). Microwaves kill microbes by affecting proteins and depend highly on the molecules’ bound water content. Absorbed energy is converted to heat energy (Hong et al., 2014; Park et al., 2006). It has the advantage of fast heating and lowers energy expenditure, but they need more equipment and technical expertise (Green et al., 1997).
Sonication
Sonic or supersonic waves kill microbes by a rapid compression and liquid release, tearing the suspended cells into pieces (Otte et al., 2018; Rahn, 1945).
Radiation processes
Electromagnetic radiation (UV light and gamma rays) and particulate radiation such as accelerated electrons are used for sterilization. Radiation targets microbial DNA to kill them. Free radical is produced when exposed to gamma rays, whereas UV light causes excitation. Cobalt-60 is the source of gamma rays. 260 nm is the optimum wavelength of UV sterilization, and a mercury lamp that gives peak emission at 254 nm is a suitable source (Rattanakul and Oguma, 2018).
Pulsed electric field
A system that produces an electric field utilizing two-electrode generates acoustic and shock waves, UV irradiation, and reactive oxygen species. Although it is unaffected by particles, this process is expensive and very effective for disinfection (Anpilov et al., 2002; Frey et al., 2013; Gusbeth et al., 2009; Poyatos et al., 2011; Yadollahpour et al., 2014).
Hydrodynamic cavitation
Despite having a similar mechanism as sonication, high pressure and local temperatures are achieved by rapid mixing or pumping the process solution. Steam injection, shock wave, high-speed homogenizer, high-pressure systems, and liquid whistle are the types of reactors used (Gogate, 2011; Gogate and Pandit, 2010).
Plasma emission and shock waves
Plasma emission and shock waves, visible light emission, and UV are used for disinfection. The inactivation mechanism is thought to be irreversible destruction of membrane for bacteria and DNA and RNA damage for viruses (Mosqueda-Melgar et al., 2008; Sale and Hamilton, 1967; Sabino et al., 2020; Stratton et al., 2015).
Ultrasound
It is a complex process that inactivates microbes by the growth of bubbles. Dust or bacteria become part of the bubbles in company with vapor and gas. When the bubble collapse, microbes are exposed to high pressure (100 MPa) and temperature (5,000 K) for a few seconds, which cause their inactivation (Crum, 1994; Flint and Suslick, 1991; Suslick et al., 1999; Tandiono et al., 2011).
Magnetic treatment
Magnetic treatment is a new method of physical disinfection of water. The magnetic field creates a polarizing effect on ions and water molecules when the water and its impurities are in a state of thermodynamic equilibrium. There are several different hypotheses about the mechanism of magnetic treatment, and more research is needed for a better understanding (Biryukov et al., 2005; Li et al., 2020b; Vaskina et al., 2020).
Filtration
It is the process that removes microbes without destroying them. Trapping, sieving, and adsorption within the matrix of filter material is the mechanism involved in the filtration technique (Nnadozie et al., 2015).
Chemical disinfectants and sterilant
Disinfectants are chemically diverse agents with small and usually lipophilic molecules that eliminate many pathogenic organisms and penetrate the skin quickly to induce a direct reaction. Therefore, they can destroy pathogenic microorganisms on surfaces (Chernyshov and Kolodzinska, 2020). There are different types of chemical disinfectants, and they kill microbes through other mechanisms.
Alcohols
Other than bacterial spores, alcohol can kill microbes efficiently. The antimicrobial effect of alcohol depends on the presence of water, as proteins tend to denature quickly in the presence of water. Ethyl alcohol and isopropyl alcohol are most commonly used in healthcare settings, and their optimum bactericidal concentration is 60%–90% v/v in water. Alcohol-based disinfectant activity against microbes drops when the concentration is below 50% (Block, 2001; Morton, 1950; Jing et al., 2020; McDonnell and Russell, 2001). Concentration between 60% and 80% of ethyl alcohol is an effective virucidal agent for all lipophilic viruses and many hydrophilic viruses such as rotavirus and adenovirus, but not hepatitis A virus or poliovirus (Mbithi et al., 1990; Tyler et al., 1990). On the other hand, isopropyl alcohol is active against lipid viruses (Armstrong and Froelich, 1964; Kampf et al., 2020).
Chlorine and chlorine compounds
The most commonly used chlorine disinfectants are the hypochlorites, available in solid (sodium hypochlorite) and liquid (calcium hypochlorite) forms as a household bleach sodium hypochlorite is used as an aqueous solution at 5.25%–6.15% concentration (Rutala and Weber, 1997). Sodium dichloroisocyanurate, chlorine dioxide, and chloramine-T are the chlorine-releasing agents used in healthcare settings as their bactericidal effect is more prolonged (Clasen and Edmondson, 2006; Coates and Wilson, 1989). There are various possible mechanisms of action for these compounds, although the precise mechanism is not known. Sulfhydryl enzymes and amino acids oxidation, losing intracellular contents, protein synthesis inhibition, decreasing uptake of nutrients and oxygen, respiratory component oxidation, DNA breaks, decreased production of adenosine triphosphate, ring chlorination of amino acids, and depressed DNA synthesis are the possible modes of action of these disinfectants (Block, 2001). The combination of these factors or the effect of the disinfectant on a binding site may cause the death of microbes (Hernández-Navarrete et al., 2014).
Formaldehyde
Formaldehyde is an effective disinfectant and sterilant in its aqueous and gaseous form (Kinyoun, 2006; Lin et al., 2020). The aqueous solution of formaldehyde is known as formalin which contains 37% formaldehyde (McCulloch and Costigan, 1936). Alkylation of the ring nitrogen atoms present in purine bases and sulfhydryl amino groups of the proteins by formaldehyde causes the microbe to be inactivated (Block, 2001). Formaldehyde is a potent carcinogen, and the US Federal Agency on Occupational Safety and Health Administration instructed it to be handled carefully in the workplace. It can be fatal if ingested by employees and can cause skin irritation and respiratory problems (Costa et al., 2019; Sweatt, 2020).
Glutaraldehyde
It is a saturated dialdehyde which is not only an effective disinfectant but also a sterilant. An aqueous solution of glutaraldehyde is not sporicidal unless activated by adding an alkylating agent (pH 7.5–8.5) with a shelf-life of a minimum of 14 days. To overcome this limitation, a novel formulation such as glutaraldehyde-phenol-sodium phenate, potentiated acid glutaraldehyde, and stabilized alkaline glutaraldehyde is used, having its microbicidal activity for 28–30 days (Miner et al., 1977; Sehmi et al., 2016). Glutaraldehyde kills microbes by altering DNA, RNA, and proteins by alkylating the hydroxyl, carboxyl, sulfhydryl, and amino groups (Block, 2001). Because of its excellent biocidal property, ability to work even in the presence of organic load (20% bovine serum), and noncorrosive action to various equipment, it is used widely in healthcare facilities (Lu et al., 2020; Rutala et al., 1991).
Quaternary ammonium compounds (QACs)
They are an established disinfectant and good cleaning agent. However, cotton and gauze pad-like materials and high-water hardness can make them less microbicidal. The active ingredient can be absorbed by cotton and gauze materials and insoluble precipitates, respectively (Gerba, 2015; Nasr et al., 2018). The disintegration of the cell membrane, essential cellular protein denaturation, and energy-producing enzyme inactivation caused by these compounds kill microbes (Kampf et al., 2020; Ogilvie et al., 2021; Pratelli, 2008; Saknimit et al., 1988). Alkyl didecyl dimethyl ammonium chloride, alkyl dimethyl benzyl ammonium chloride, and dialkyl dimethyl ammonium chloride are some of the QACs used in healthcare settings. Fourth-generation QACs, also referred to as twin-chain or dialkyl quaternary (e.g., dioctyl dimethyl ammonium bromide and didecyl dimethyl ammonium bromide), are capable of retaining their activity in hard water and also can tolerate anionic residues (Block, 2001).
Phenolics
Phenols are protoplasmic poisons at high concentrations; they precipitate the cellular proteins by penetrating and distorting the cell wall. Phenol derivatives of low molecular weight and phenols of low concentration inactivate (Walsh et al., 2019), essential enzyme systems cause critical metabolite leakage, resulting in bacterial death (Block, 2001). Ortho-phenylphenol and ortho-benzyl-para-chlorophenol are commonly used phenol derivatives found in hospital disinfectants, and they work more efficiently than the parent compound. Porous materials absorb the phenolics, and the residual disinfectant is capable of irritating tissue. Para-tertiary butyl-phenol and para-tertiary amyl phenol in phenolic detergent can cause skin depigmentation (Kahn, 1970).
Peracetic acid
It is an effective agent that works against all microbes and has several advantages. It does not leave any residue, can remove organic material, and does not disintegrate into harmful products such as acetic acid and reactive oxygen species (Ao et al., 2021; Block, 2001; Kahn, 1970). Although not clearly understood, it is assumed to work similarly to other oxidizing agents such as protein denaturation, disruption of cell walls permeability oxidation of sulfhydryl and sulfur bonds in enzymes, proteins, and other metabolites (Block, 2001; McDonnell and Russell, 1999). Diluted peracetic acid solution (e.g., 1%) is less stable, but with higher concentration (e.g., 40%), it retains its activity for a more extended period. Its corrosive effect on several metals (e.g., steel, galvanized iron, copper, bronze, and brass) can be minimized by pH modification and additives (Ao et al., 2021; Block, 2001; Kahn, 1970).
Hydrogen peroxide
Hydrogen peroxide is a strong and effective biocidal agent and works against a wide range of microbes and spores. It produces destructive hydroxyl free radicals that attack DNA, essential cell components, and membrane lipids. Although aerobic and facultative anaerobes with cytochrome systems can withstand metabolically produced hydrogen peroxide, they cannot tolerate the concentration of hydrogen peroxide in disinfectants (Block, 2001; Ríos-Castillo et al., 2017). 3% hydrogen peroxide is an effective disinfectant when used on inanimate surfaces, and 3%–6% concentration is used for soft contact lenses (Silvany et al., 1990), ventilator (Judd et al., 1968), endoscope (Vesley et al., 1992), fabrics (Neely and Maley, 1999), and tonometer biprisms (Lingel and Coffey, 1992).
Ortho-phthalaldehyde
Ortho-phthalaldehyde (OPA) is a clear, pale-blue liquid that contains 0.55% 1,2-benzenedicarboxaldehyde with a pH of 7.5. Despite having a similar mode of action as glutaraldehyde, OPA has less potency in cross-linking. It is reimbursed by its lipophilic aromatic nature that assists its uptake by the outer layer of Gram-negative bacteria and mycobacteria (Simons et al., 2000; Walsh et al., 1999). OPA kills spores by blocking their germination process (Cabrera-Martinez et al., 2002). Although excellent material compatibility, it stains protein in gray and should be handled carefully (Rutala and Weber, 1999).
Iodophors
Iodophors are a mixture of iodin and its solubilizing agent or carrier. They are iodine-releasing agents. The released iodine can penetrate the microbial cell membrane and damage proteins by attacking the sulfuryl and disulfide bonds. It can also damage nucleic acid. Povidone-iodine is the most common and widely used iodophor. They are nonstaining, nontoxic, and nonirritating (Block, 2001; Eggers et al., 2018a; 2018b; Gharpure et al., 2020; Kariwa et al., 2006).
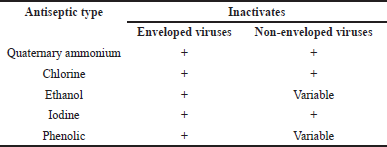
CORONAVIRUSES
The main component of the virus, a nucleic acid, is surrounded by capsids which protect the nucleic acid and facilitate binding of the virus to the host cell. The nucleic acid is the component that codes for the essential element for viral replication (Martin, 2003). Viruses are incapable of replicating when they are outside of the host cell. Still, they can survive for a defined time depending on the environment and infect a suitable host cell to replicate. Viruses use the host cell machinery to replicate (Yeargin et al., 2016). They can infect various host cells, including bacteria, and cause disease (Sidwell et al., 1966). CoVs are the member of the subfamily Orthocoronavirinae from the family Coronaviridae of the order Nidovirales. They are +ssRNA enveloped viruses (V’kovski et al., 2021). They can infect a wide range of hosts (Saif et al., 2019) and cause respiratory disease. Although human coronaviruses (HCoVs) cause mild respiratory diseases and common cold in humans, the adapted forms from the nonhuman host such as SARS-CoV-1, MERS-CoV, and SARS-CoV-2 are capable of causing severe illness (Xu, 2020a).
The novel coronavirus, SARS-CoV-2, contains spike glycoprotein that binds to the sialic acid receptor of the host cell (Tortorici et al., 2019). It is an enveloped virus and causes respiratory infection (V’kovski et al., 2021; Xu, 2020b). The binding of the spike glycoprotein to the specific receptor of the human respiratory tract, angiotensin-converting enzyme-2, facilitates viral entry. The low endosomal pH helps with the proteolytic activation of the spike glycoprotein. So, the coating structure that enables the access of the virus to the host cell is a crucial target of antiviral drug discovery (Zhang et al., 2020). The disinfectants inactivate viruses by causing damage to either their proteins or their genome (Alvarez and O’Brien, 1982; Dennis Jr et al., 1979; Kim et al., 1980; O’Brien and Newman, 1979; Roy et al., 1981). Disinfecting agents used for different coronaviruses are shown in Table 1.
STABILITY OF SARS-COV-2 IN AIR AND ON DIFFERENT SURFACES
The SARS-CoV-2 is spread on the dry surfaces through respiratory droplets secreted from the infected person’s nose, mouth, and eyes and is considered the primary route of transmission of this virus (Chan et al., 2020). Low humidity and temperatures increase the viability of SARS-CoV-2 in the droplets (Moriyama et al., 2020). HCoVs can remain infectious for 2 hours to 9 days at room temperature on different surfaces (Kampf et al., 2020). This time can be up to 28 days for veterinary coronaviruses, and an increase in the temperature to 30°C or more induces shorter endurance of coronavirus (Kampf et al., 2020). Studies by Kampf et al. (2020) and van Doremalen et al. (2020) also showed that SARS-CoV-2 could survive on a variety of surfaces from hours to days (Table 2) (Choi et al., 2021; van Doremalen et al., 2020). The SARS-CoV-2 was more stable on plastic and stainless steel than on copper and cardboard, and the viable virus was detected up to 72 hours, and its titer was significantly reduced afterward (van Doremalen et al., 2020). The virus can remain infectious and feasible in aerosols for 3 hours and on surfaces up to days (van Doremalen et al., 2020). The persistence time on inanimate surfaces varied from minutes to days, depending on environmental conditions. SARS-CoV-2 can be sustained in the air in closed unventilated buses for at least 30 minutes without losing infectivity. Additionally, MERS-CoV can survive 28 days or more (Ren et al., 2020). Absorbent materials like cotton are safer than unabsorbent materials for protection from virus infection. The risk of transmission via touching contaminated paper is low (Ren et al., 2020). However, the significance of indirect communication through contamination of inanimate surfaces is uncertain and requires further investigation (Armstrong and Froelich, 1964; Chan et al., 2020; Choi et al., 2021; Moriyama et al., 2020; Ren et al., 2020; van Doremalen et al., 2020).
PHYSICAL INACTIVATION OF SARS-COV-2
The inactivation of airborne viruses and those deposited on active surfaces reduces disease transmission, which is a necessary counterpreventive measure in combating the COVID-19 pandemic. Physical factors such as temperature and humidity greatly influence the survival of viruses on surfaces. However, scientists reported the rapid inactivation of gastroenteritis virus (TGEV) and mouse hepatitis virus (MHV) at all humidity levels (Casanova et al., 2010). Furthermore, in an indoor space, heat and irradiation such as UV inactivated TGEV and MHV (Casanova et al., 2010; Garcia de Abajo et al., 2020). Nevertheless, a study has shown that the spread of SARS-CoV-2 is not strongly affected by the change in weather conditions (Casanova et al., 2010). Therefore, it is crucial to efficiently decrease viral transmission rates within indoor spaces such as shared offices, classrooms, healthcare facilities, and public transport vehicles. The use of physical disinfecting agents in such areas is easily deployable and economically affordable (Garcia de Abajo et al., 2020).
HEAT AND ULTRAVIOLET IRRADIATION
Sufficient physical inactivation of SARS-CoV-2 can be achieved through exposure to heat and UV radiation. For instance, more than 50% viral inactivation was effectively achieved within 5 min of exposure of SARS-CoV-2 to heat at 56°C or by applying UV irradiation. The viral cytopathic effect and infectivity were drastically distorted due to physical manipulations on the cells, affecting the titer, stability, and virulence (Kariwa et al., 2006). A study revealed that the SARS-CoV-2 virus is highly stable at 4°C, and when exposed to varying temperatures, exceptionally as high as 56oC, the virus loses its infectivity and virulence. The decrease in viral titer supports heat as a crucial physical inactivator of the virus during the pandemic (Abraham et al., 2020; Chin et al., 2020). Similarly, prolonged exposure of the virus to heat for about 30 min reportedly affects viral infectivity and stability, and therefore, a high temperate climate might be beneficial in inactivating the virus (Kariwa et al., 2006).
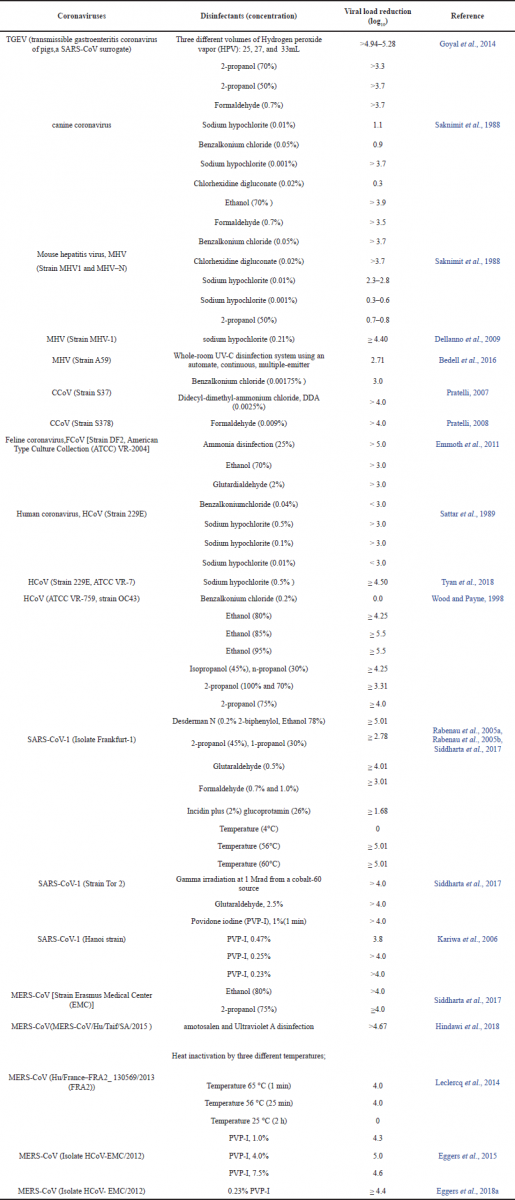 | Table 1. Disinfectants and their ability to reduce the viral load for different coronaviruses (Bedell et al., 2016, Dellanno et al., 2009, Eggers et al., 2015, Eggers et al., 2018a, Emmoth et al., 2011, Goyal et al., 2014, Hindawi et al., 2018, Kariwa et al., 2006, Leclercq et al., 2014, Noorimotlagh et al., 2021, Pratelli, 2007, Pratelli, 2008, Rabenau et al., 2005a, Rabenau et al., 2005b, Saknimit et al., 1988, Sattar et al., 1989, Siddharta et al., 2017, Tyan et al., 2018, Wood and Payne, 1998). [Click here to view] |
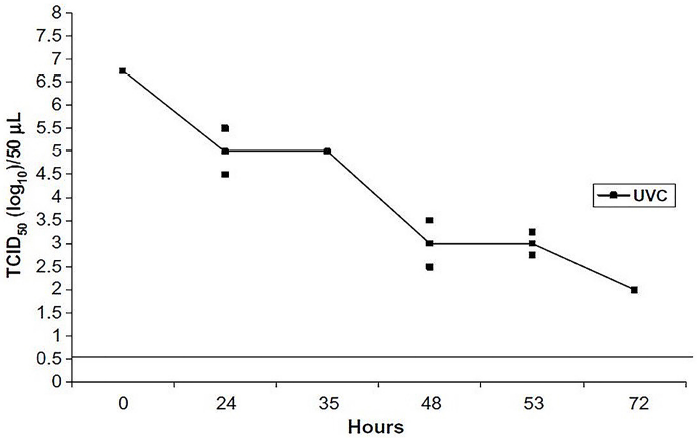 | Figure 1. Effect of UV-C radiation on the infectivity of CCoV in vitro. Virus aliquots were placed at about 4 cm from the UV-C source, then removed, and then titrated by the TCID50 assay at fixed time points. The straight line delineates the detection limit of the test (reprinted with permission from Pratelli et al. (2008), licensed under CC-BY-4.0, Copyright, (2008), @ Elsevier Ltd.). [Click here to view] |
Furthermore, UV, especially UV-C radiation, is one of the primary methods for the physical inactivating of viruses. It is harmful to pathogenic microorganisms due to its molecular damage to RNA and DNA bases. At the range of 200−280 nm wavelength, specifically using fluorescence light of 254 nm, UV-C reportedly inactivates influenza and SARS-CoV-2 viruses. Thus, using these specific lights in the sterilization process in hospitals, laboratories, and homes is essential (Abraham et al., 2020; Derraik et al., 2020; Garcia de Abajo et al., 2020). A previous study revealed the advantages of UV-C in preventing infection by viruses, especially SARS-CoV-2 (Mackenzie, 2020; Szeto et al., 2020). In animals, UV-C has proven to decrease Canine CoV (CCoV), seen in puppies (Fig. 1). Therefore, this can ideally experiment on human CoVs (Pratelli, 2008).
Moreover, UV-C is recently used in reducing air transmission of viruses. It is also an essential method of inactivating viruses and, therefore, can experiment in the disinfection process against the SAR-CoV-2 (Beck et al., 2017; Mphaphlele et al., 2015; Xia et al., 2019). However, precautionary measures should be adopted in applying UV-C light as a sterilization method because it can significantly damage eyes and produce carcinogenic effects considerably if the recommended limit exceeds (Garcia de Abajo et al., 2020).
Several other scientific studies also highlighted the importance of UV-induced viral inactivation. Inagaki et al. (2020) reported the concentration-dependent rapid inactivation of SARS-CoV-2 upon exposure to UV light-emitting diode (LED) of wavelength 280 ± 5 nm and subsequent decrease in cytopathic effect. In addition to heat and UV, sunlight is one of the physical inactivation processes of the SARS-CoV-2 virus. It was reported that bright day sunlight above sea level causes variations in the life cycle of CoVs and rapidly inactivates the virus on the surface. This implies that viruses in indoor and outdoor spaces are affected by the different amounts of radiation. However, this needs to be further investigated to ascertain the effects of sunlight (Fig. 2) (Ratnesar-Shumate et al., 2020). The variations in the reported cases of CoV infection across various temperate regions have not realistically proven the hypothesis. For instance, the total reported cases in France as of November 2020 stand at 2,086,288 (3.19%). In comparison, a less temperate Ukraine recorded 583,510 (1.34%) with a death rate of 2.26% and 1.78%, respectively (Quinn et al., 2021), indicating the need for further investigation to assert the hypothesis.
It is imperative to note that fomites, inanimate objects contaminated with infectious agents, serve as a medium for spreading endemic diseases, including coronaviruses. Therefore, there is a need to decontaminate and inactivate surfaces and other indoor places to avoid spreading the disease (Castaño et al., 2021; Choi et al., 2021). Physical inactivation is relevant to disease control due to the destruction of the glycoprotein and the lipid membrane bilayer of the virus leading to molecular structural damage. The UV-C light is proven to effectively reduce the cytopathic effects of the virus, reducing the air transmission of viruses. Hence, UV-C light is essential for further advances in curbing the spread of viral diseases, including SARS-CoV-2.
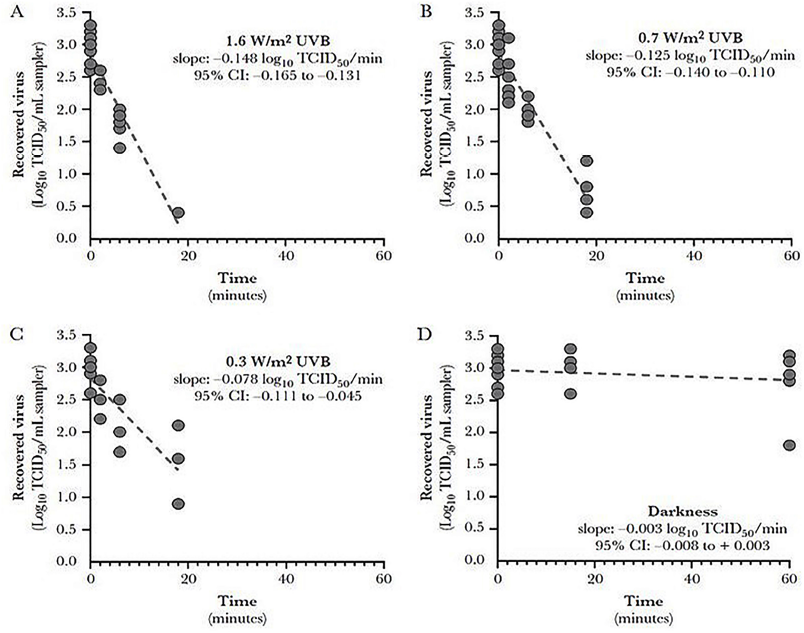 | Figure 2. Inactivation rates for SARS-CoV-2 suspended in simulated saliva as a function of UVB irradiance. Linear regression fits SARS-CoV-2 suspended in simulated saliva and recovered from stainless steel coupons following exposure to different light conditions. Inactivation rates for exposure to any level of UVB irradiance were significant than those observed in darkness (p < 0.001). Additionally, the inactivation rates observed for UVB irradiances of 1.6 and 0.7 W/m2 were significantly greater than those observed for 0.3 W/m2 (p ≤ 0.065). The slope of the regression line for darkness was not significantly different from zero. Goodness of fit parameters, specifically r2 and standard deviation of the residuals (RMSE), for each fit were (A) r2 = 0.922 and RMSE = 0.24; (B) r2 = 0.906 and RMSE = 0.28; (C) r2 = 0.670 and RMSE = 0.40; and (D) r2 = 0.041 and RMSE = 0.32. CI, confidence interval; TCID50, median tissue culture infectious dose (reprinted with permission from Ratnesar-Shumate et al. (2020), licensed under CC-BY-4.0, Copyright (2020), @ Elsevier). [Click here to view] |
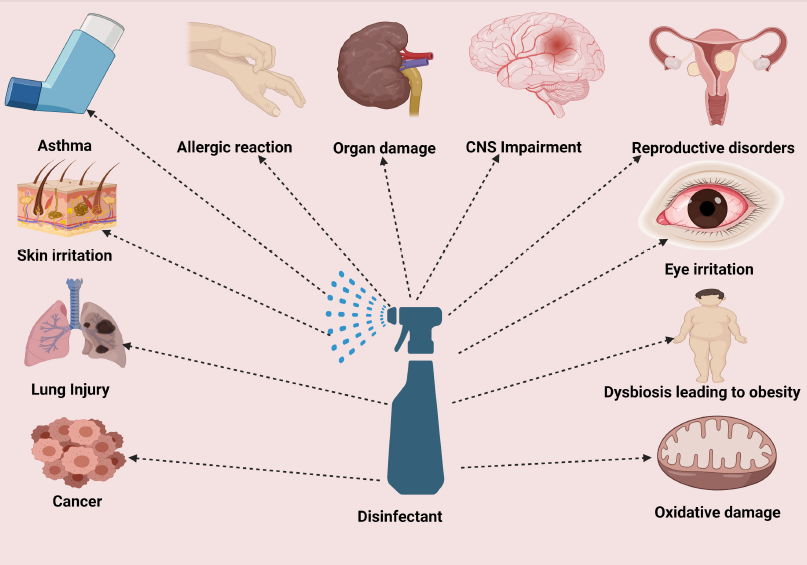
CHEMICAL INACTIVATION OF SARS-COV-2
Some of the most influential and domestic-friendly disinfectants are recommended by the World Health Organization (WHO) for hand rubbing include ethanol (80% v/v) and isopropanol (75% v/v) (Pittet et al., 2009). Classes and examples of common disinfectants are depicted (Table 3) (Al-Sayah, 2020; Benzoni and Hatcher, 2019; Kim et al., 2018), commonly applied during the COVID-19 pandemic (Chernyshov and Kolodzinska, 2020). Unfortunately, disinfection alone may not prevent the spread of any pandemic. General hygienic conditions such as hand washing using soap and water, antiseptic, and hand sanitization, especially using alcohol-based sanitizers or hand rubs, are essential in curbing pandemic spread (Gold et al., 2021). Gold and Avva (2018) reported the WHO definition of alcohol-based hand rub (ABHR) as “an alcohol-containing preparation (liquid, gel or foam) designed for application to the hands to inactivate microorganisms and temporarily suppress their growth. Such preparations may contain one or more types of alcohol, other active ingredients with excipients, and humectants” (WHO, 2009). Other classes that are nonalcohol-based are also available. Still, they are less preferred by health agencies like the Centre for Disease Control and Prevention (CDC) (Berardi et al., 2020) and the WHO (Kampf and Kramer, 2004; Todd et al., 2010) in fighting COVID-19. They have low efficacy and a narrow spectrum of activity compared to alcohol-based products and hence the recommendation and acceptability of alcohol-based products (Yip et al., 2020).
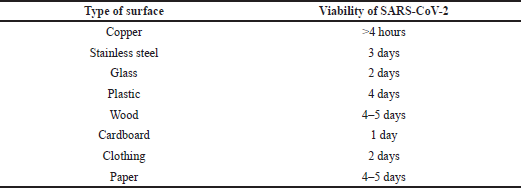 | Table 2. Sustainability of SARS-CoV-2 on different surfaces as reported by Choi et al. (2021) and van Doremalen et al. (2020). [Click here to view] |
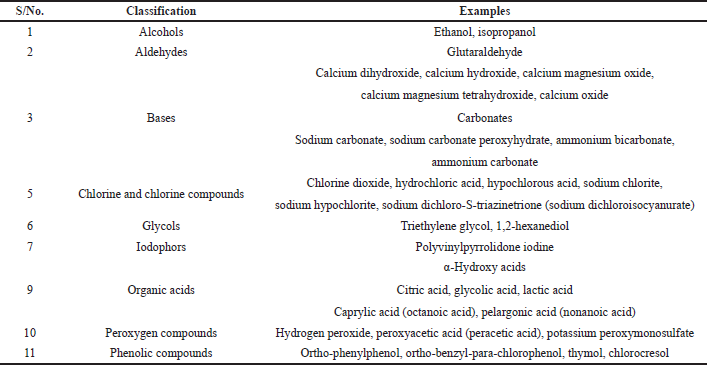 | Table 3. Commonly used disinfectants and other additional compounds. [Click here to view] |
Most disinfectant products contain additional ingredients which aid in fighting several pathogenic organisms. Such active ingredients include QACs, hydrogen peroxide, peroxyacetic acid, isopropanol, ethanol, sodium hypochlorite, octanoic acid, phenolic, trimethylene glycol, L-lactic acid, and glycolic acid (Table 2) (Nawrocki et al., 2010). On many occasions, the products are designed to achieve particular needs and avoid the harmful effects of the chemicals involved. For instance, isopropanol is irritating to the skin; as such, emollients (glycerol or propylene glycol) are added to decrease possible skin irritations when applied (Berardi et al., 2020). It is essential to carefully read the labels of all products before use to avoid toxic and harmful effects on human health.
IODINE-BASED AGENTS
Povidone-iodine, chemically known as polyvinylpyrrolidone (PVP-I), is an iodine-based synthetic polymer obtained by polymerizing a monomeric compound N-vinylpyrrolidone. The PVP-I can incorporate hydrophilic and hydrophobic compounds due to its chemical characteristics such as nontoxic, stability of pH, high temperature-resistant, compatibility, inert, and biodegradable properties. These properties enable the PVP-I to be formulated in various domestic personal hygiene solutions to effectively prevent pathogenic microorganisms, including the CoVs disease (Kurakula and Rao, 2020). The virucidal activities of five personal hygiene products including antiseptic solution (10%), skin cleanser (7.5%), gargle/mouth wash (1%), gargle/mouth wash (1.0%, 1:2 dilution), and throat spray (0.45%) were reported to contain PVP-I at different percentages. They have been assessed against SARS-CoV-2 using suspension, cytotoxicity (on Vero E6 cells), and virus kill-time assays. The products demonstrated satisfactory virucidal activity of ≥ 99.99%, equivalent to 4 log10 reductions of viral titer against SARS-CoV-2 just within a 30 s period of contact. Anderson et al. (2020) reported the virucidal activity of different PVP-I products (Table 4) (Hassandarvish et al., 2020). Similar action has been previously reported for the products against SARS-CoV-1 and MERS-CoV, suggesting their applicability as effective disinfectants in preventing CoV infections (Hassandarvish et al., 2020).
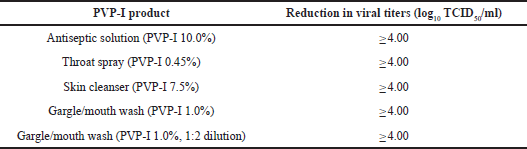 | Table 4. Virucidal activity of PVP-I products against SARS-CoV-2 virus with 30s contact time as rreported by Hassandarvish et al. (2020). [Click here to view] |
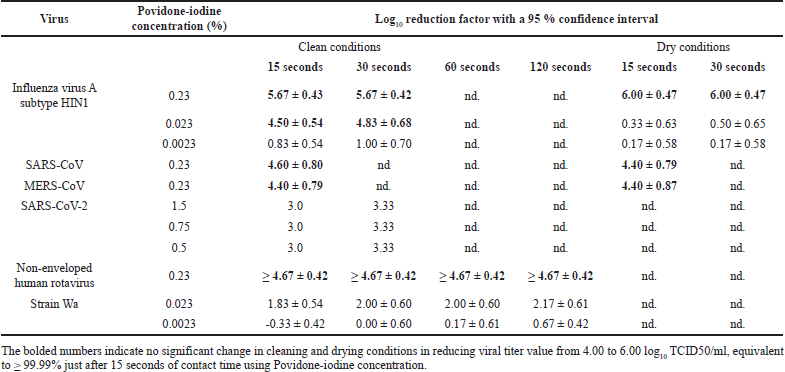 | Table 5. Virucidal activity of various concentrations of PVP-I in mouthwash against SARS-CoV-1, SARS-CoV-2, MERS-CoV, influenza virus A, and rotavirus as reported by Bidra et al. (2020b) and Eggers et al. (2018a). [Click here to view] |
In another separate study, the virucidal effects of an oral antiseptic PVP-I solution at concentrations of 0.5%, 1.0%, and 1.5% were evaluated in vitro against SARS-CoV-2 using 70% ethanol as a positive control. The infectivity of the virus was demonstrated and quantified using dilution assay and the reduction of log value (LRV) in comparison with the positive control (ethanol) and negative control (water). The results indicate that SARS-CoV-2 viruses become inactivated by all tested concentrations after 15 s of administration better than 70% ethanol, whose inactivation effect was later 30 s. At each concentration, 0.5%, 1.0%, and 1.5% solutions show a virus titer and LRV of < 0.67 and 3.0, respectively, compared to 70% ethanol with virus titer of 1.5 and LRV 2.17 after 15 s. The oral antiseptics display a potent virucidal activity even at a low concentration of 0.5%, suggesting its applicability and effectiveness in preprocedural oral rinsing as adjunctive treatment in patients infected with SARS-CoV-2 (Bidra et al., 2020b). Similarly, PVP-I oral antiseptic rinses show more potent virucidal activity in vitro at concentrations of 0.5%, 1.25%, and 1.5% compared to hydrogen peroxide (H2O2) at 1.5% and 3.0%. At the same time, ethanol and water serve as positive and negative controls, respectively. Subsequently, the SARS-CoV-2 strains were entirely inactivated by the tested concentrations of PVP-I after 15 and 30 s of contact time. Simultaneously, minimal virucidal effects were observed with H2O2 at lower and higher concentrations, suggesting PVP-I preprocedural oral rinsing preference over H2O2 (Bidra et al., 2020a). The PVP-I at a concentration of 0.23% was reported to rapidly inactivate SARS-CoV, MERS-CoV, influenza virus A (H1N1), and rotavirus after 15 s of exposure. In another study, when used as mouthwash at 7% concentration, PVP-I possesses virucidal activity against SARS-CoV-1, MERS-CoV, and influenza virus A quantitatively using suspension assay. Furthermore, PVP-I at a dilution ratio of 1:30 with water (concentration of 0.23%) inactivated SARS-CoV-1, MERS-CoV, influenza virus A, and rotavirus and significantly decreased viral titer value from 4.00 to 6.00 log10 TCID50/ml, equivalent to ≥ 99.99% just after 15 seconds of contact time. However, Eggers et al. (2018a) and Bidra et al. (2020b) reported little or no significant change when extending contact time (Table 5). Therefore, PVP-I’s comprehensive coverage and effective inactivation make it an oropharyngeal agent of choice for protecting individuals from viral infections (Eggers et al., 2018a).
Some PVP-I products were reported to effectively reduce SARS-CoV-2 infectivity below detectable limits, similar to 70% ethanol (Kariwa et al., 2006). They have overwhelming acceptability as disinfectants due to their broad virucidal activity against many pathogens. Therefore, this suggests a strong indication that PVP-I products are adequate for the inactivation of SARS-CoV-2 and other pathogenic microorganisms. However, the inefficiency of iodine-based compounds has been documented earlier for environmental/surface disinfection of hepatitis A virus (HAV). Similarly, few other studies found Iodophors with less virucidal efficacy (Bond et al., 1983; Lloyd-Evans et al., 1986; Sattar et al., 1989). In addition, many iodine-based products and their by-products such as diatrizoate, iomeprol, and iopamidol are unavailable for surface disinfection due to their staining and toxicity pollution properties to the environment and in some instances highly persistent and difficult to remove from surfaces. Accumulation of such compounds in large amounts might pose potential threats and destabilization of the ecosystem. Therefore, iodine-based products are mostly not recommended for surface disinfection (Steger-Hartmann et al., 2002).
ALCOHOL-BASED AGENTS
Alcohol-based hand preparations containing isopropanol, ethanol, n-propanol, or their combinations are undoubtedly some of the most frequently used hand rubs during the SARS-CoV-2 pandemic and other viral pandemics such as MERS. The effectiveness of the preparations depends on the type of alcohol and the quantity applied, concentration, and time of exposure (Boyce and Pittet, 2002; Todd et al., 2010). The enveloped viruses, including SARS-CoV-2, SARS-CoV-1, and MERS-CoV, possess a lipid layer protecting the viral core, of which most antiseptic agents can effectively inactivate within 1 min of exposure (Wang et al., 2020b). One of the strategic approaches to inactivate CoVs is to target the lipid envelope, representing the organism’s virucidal potency. In the 2003 SARS outbreak, the strategy was applied using 60%–70% ethanol concentration to decontaminate viral material detected on surfaces within a hospital effectively. Therefore, ethanol at higher concentrations will effectively interfere with the lipid envelope of CoV (Hulkower et al., 2011; Sattar et al., 1989). Studies have also indicated that, to effectively inactivate the lipid envelope of some viruses, alcohol-based antiseptic preparations such as isopropanol at 70%–91.3% and ethanol at 60%–71% concentrations are highly recommended (Berardi et al., 2020; Kampf et al., 2020). The United States Federal Drug Agency reaffirmed the concentration-dependent effectiveness of some alcohol-based disinfectants and recommended them during the COVID-19 health emergency (Baye et al., 2021). Furthermore, the CDC recommends a baseline concentration of 60% for ethanol preparations meant for healthcare and the public for adequate disinfection, especially when foam and water are not easily accessible (Ramphul and Mejias, 2020). Moreover, a recent study conducted on Zika virus, Ebola virus, SARS-CoV-1, and MERS-CoV indicated that alcohol-based formulations such as ethanol 80% (v/v), isopropyl alcohol 75% (v/v), or the combination of both preparations effectively killed the envelope viruses and therefore, the WHO recommended the concentrations during the SARS-CoV-2 pandemic (Siddharta et al., 2017). To further buttress this point, commercially available alcohol-based hand sanitizers in the US market with a concentration of 70% ethanol effectively decreased the amount of SARS-CoV-2 virus below the threshold limit of >3 log10 reductions (Leslie et al., 2021). Similarly, ethanol at >30% concentration efficiently inactivated the virus when exposed within 30 seconds (Kratzel et al., 2020). The alcohol-based sanitizers have a significant setback in skin dryness, primarily when used for a long time. Therefore, emollients such as glycerol and glycerine are added to overcome such effects (Ahmed-Lecheheb et al., 2012).
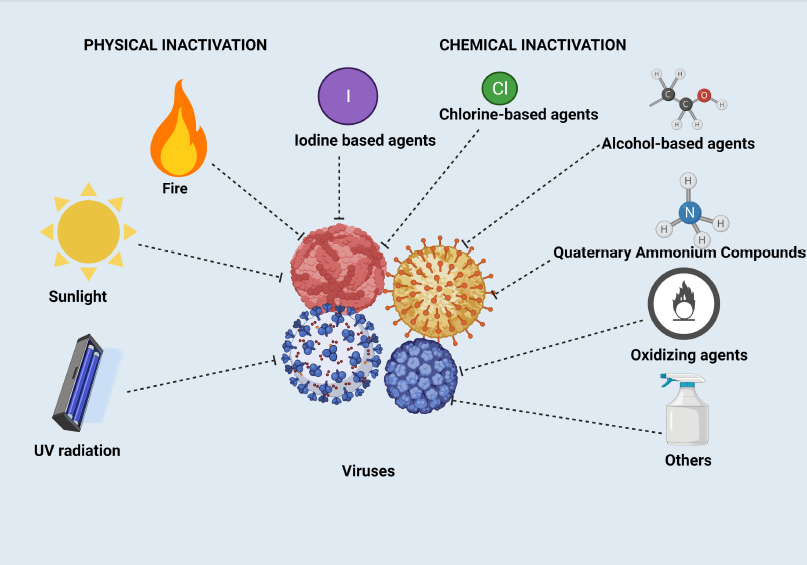 | Figure 3. Physical and chemical inactivation of SARS-CoV-2. [Click here to view] |
Generally, alcohol-based hand sanitizers are the most commonly employed hand rubbing disinfecting agents against SARS-CoV-2 and other endemic viruses. One of the most common added ingredients in alcohol-based disinfectants with potential antiviral activity is the QACs, with a broad spectrum of activity against enveloped viruses and CoVs. Illustrations regarding different types of disinfectants that are physical and chemical inactivation of SARS-CoV-2 are shown in Figure 3.
OTHER DISINFECTANTS
Other essential disinfectants effective in decontaminating and inactivating viruses include chlorine-based, halogen compounds, potent oxidizing agents, and sodium hypochlorite (Chernyshov and Kolodzinska, 2020; Pradhan et al., 2020). Recently, large amounts of chlorine-based disinfectants have been widely used to control the spread of the SARS-CoV-2 outbreak in environments due to low cost and effectiveness on viral infection. Chlorine-based disinfectants are the most common agents that threaten aquatic life and the environment. Halogen compounds such as hypochlorous acid and hypochlorite ions are effective in decontamination and inactivating viruses and pathogenic microorganisms. Scheme 1 represents how sodium hypochlorite solutions can be prepared by reacting chlorine and sodium hydroxide solutions to give hypochlorous acid (HOCl) and sodium hypochlorite (NaOCl) solution (Pradhan et al., 2020).
Cl2 + H20 favored in alkaline pH → HOCl + H+ + Cl−
HOCl + NaOH favored in alkaline pH → NaOCl + H+
Scheme 1. Formation of sodium hypochlorite solution.
The hypochlorous acid is a potent oxidizing agent with higher biocidal potency compared to NaOCl. The recommended disinfectant concentration of sodium hypochlorite is 5% in 1:100 dilutions for effective mopping of nonporous surfaces at ≥ 10 min contact time. In contrast, 30 min contact time is required (Carr et al., 1996; Chen et al., 2016). Sodium chlorite is another essential disinfectant with proven efficacy against HAV compared to other disinfectants such as chlorhexidine digluconate, sodium hypochlorite, phenol, sodium phenate, and diethylenetriamine disinfectants (Abad et al., 1997). However, sodium chlorite was ineffective at 0.275% concentration against HAV (Mbithi et al., 1990). Recently, a more environmentally friendly chemical, N-decyl dimethyl ammonium chloride or bromide, effectively inactivates SARS-CoV-2 on surfaces within 0.5 min in a laboratory experiment. Therefore, this could be suggested to disinfect surfaces contaminated with the virus (Xiling et al., 2021).
Oxidizing agents are one of the most effective disinfectants that inactivate viruses and other pathogenic microorganisms. Oxidizing solid compounds such as 1% hydrogen peroxide are disinfectants in intraoral procedures due to their effectiveness (Ather et al., 2020; Diegritz et al., 2020; Izzetti et al., 2020; Jamal et al., 2021; Zimmermann and Nkenke, 2020). Hydrogen peroxide is recommended because it can inactivate SARS-CoV-2 through an oxidation mechanism (Peng et al., 2020). Furthermore, it is worth noting that 62%–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite, and povidone-iodine can rapidly inactivate CoVs such as SARS and MERS on inanimate surfaces within 1 min of exposure (Kampf et al., 2020). A study by Mileto and coworkers reported the inactivation of SARS-CoV-2 using a diluted solution of 3% H2O2 with citric acid and an aqueous solution of sodium percarbonate on surfaces within 5 and 15 minutes, respectively, while H2O2 with no additives displayed little or no virucidal activity (Ayipo et al., 2021; Brown et al., 2021).
Similarly, a combination of 0.1% chlorhexidine, 0.05% cetylpyridinium chloride, H202 0.1% chlorhexidine, and 0.05% cetylpridiniumchloride inactivated SARS-CoV-2 particles within 30 s application as a mouth rinse, while H2O2 and chlorhexidine alone have no virucidal effects. Therefore, the combination might be used in preprocedural mouth rinse during dental treatments (Koch-Heier et al., 2021). Moreover, in SARS-CoV-2 positive subjects, 1% hydrogen peroxide used as mouth rinse could not reduce oral viral load. Therefore, hydrogen peroxide preparation alone is not recommended as an oral rinse to destroy the SARS-CoV-2 virus (Gottsauner et al., 2020). Other commonly used disinfectants include peroxides and peracids, which act by generating free radicals. These free radicals oxidize the important biochemical content of the virus, including nucleic acid, proteins, and lipids bilayer, and subsequently inactivate the virus. However, the free radicals-based preparations are usually considered the last option as disinfectants, replacing formaldehyde due to their severe systematic and neurological toxicity associated with their exposure. Hence, this limited their use against the SARS-CoV-2 virus (Songur et al., 2010).
Most disinfectants meant for household use have additional ingredients, such as the same amount of 0.50% triclosan, 0.12% parachlorometaxylenol, 0.23% pine oil, and 0.10% QACs, which are invariably reported to inactivate hepatitis virus. Among these compounds, QACs are the most common ingredients in more than 200 disinfectant preparations against the SARS-CoV-2 pandemic (Cegolon et al., 2020; Dellanno et al., 2009). There are three classes of QACs identified to have antiviral activity against CoVs and other pathogenic microorganisms, namely, (i) cetylpyridinium chloride, which is used to reduce pathogenic organisms in the mouth. It is also used in cosmetics as cleaning and personal care agents, (ii) ammonium chloride, an antiviral agent in many disinfectant preparations, and (iii) miramistin, which has a broad spectrum of activity against nonenveloped and enveloped viruses (Cegolon et al., 2020; Sanderson et al., 2003). Therefore, these agents can be formulated with other disinfectants for effective decontamination and inactivating viruses and other pathogenic microorganisms through additive and synergistic activity (Dellanno et al., 2009). This is evident when two formulated detergents containing QACs demonstrated an efficient inactivation of the SARS-CoV-2 by disrupting the lipid envelope and the spike glycoprotein of the virus, which eventually would have invaded lung cells of the host when interacting with the angiotensin-converting enzyme-receptor of the infected person (Schrank et al., 2020). In another research, it was indicated that a combination of commercially available disinfectants containing about 70% alcohol with N-alkyldimethylbenzylammonium chloride produced a reduction in viral titer by 2.03-fold.
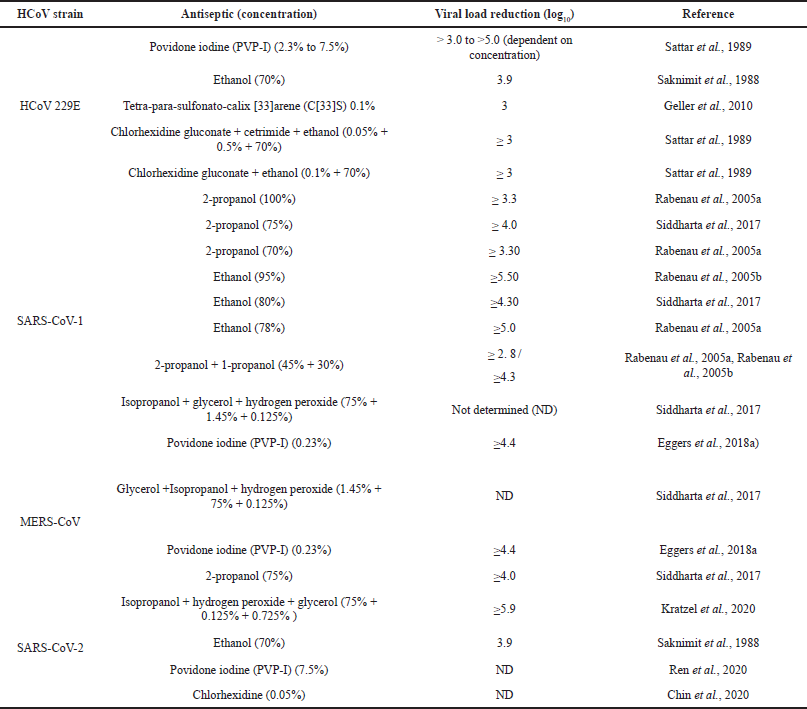 | Table 6. Effective antiseptics for different HCoVs (Chin et al., 2020, Eggers et al., 2018a, Kratzel et al., 2020, Rabenau et al., 2005a, Rabenau et al., 2005b, Ren et al., 2020, Saadatpour and Mohammadipanah, 2020, Saknimit et al., 1988, Sattar et al., 1989, Siddharta et al., 2017). [Click here to view] |
In contrast, phenolic disinfectant (o-phenyl phenol and p-tertiary amyl phenol) with ortho-phthalaldehyde reduced the titer value by 2.27 folds, indicating superior efficacy of the first combination against TGEV (Hulkower et al., 2011). Only two disinfectants, containing Nalkyldimethylbenzylammonium chloride and Lysol, demonstrated excellent activity below the viral reduction factor against poliovirus, indicating not all products are effective against viruses (Rutala et al., 2000). In another study, QAC’s, hydrochloric acid, and sodium hypochlorite-based formulations inactivated SARS-CoV-2 and other coronaviruses with virucidal efficacies between ≥ 3 and ≥ 6 log10 reduction factors (Ijaz et al., 2021). Consequently, a viral reduction factor of ?3 has been suggested as the most effective benchmark for inactivation of virucidal activity of CoVs and other life-threatening infections during surface decontamination (Abad et al., 1997; Hulkower et al., 2011; Rutala et al., 2000). However, natural products with disinfectant properties such as vinegar were less toxic and effective than commercial household disinfectants against some pathogenic organisms (Schrank et al., 2020).
Antiseptics
Substances that arrest microbial growth or activity, especially in or on living tissue, by either inhibiting their action or destroying them are antiseptics (Patterson, 1932). Skin can be contaminated directly when contact with patient secretions or indirectly by touching contaminated surfaces (L’Huillier et al., 2015). Some chemical disinfectants that are safe to use in or on tissue are used as antiseptics. Table 6 shows the efficacy of the antiseptics used for HCoVs.
Antimicrobial Resistance
Antimicrobial agents are natural, synthetic, or semisynthetic substances capable of killing or inhibiting microbial growth in vivo by interacting specifically with a target component (Donaghy et al., 2019). The ability of a microorganism to grow despite an antimicrobial agent is referred to as antimicrobial resistance (AMR), which can be acquired or intrinsic (Wales and Davies, 2015). Unlike antimicrobial agents, disinfectants and sanitizers nonspecifically target multiple components of microbes, frequently causing lethal damage to their membranes or damaging their proteins by reacting with a functional group. Because of their nonspecific nature and multiple modes of action, the microbes are less likely to become resistant to these chemicals (Donaghy et al., 2019; Wales and Davies, 2015). It is unclear that the COVID-19 pandemic has increased AMR. Many patients infected with COVID-19 were treated with antibiotics due to secondary bacterial coinfection (Rodrigo et al., 2020). About 70% of the COVID-19 patient who was hospitalized received antibiotics and often broad-spectrum antibiotics, whereas only 16% developed secondary coinfections (Abelenda-Alonso et al., 2020; Beovi? et al., 2020; Langford et al., 2020). The increased use of antibiotics is seen in nursing homes and long-term care facilities. A possible increase in self-medication with antibiotics is seen in some countries or regions of the world, increasing the risk of rising AMR (Nasir et al., 2020).
Despite having huge factors that increase the risk of raising AMR during this pandemic, some factors might favor decreasing AMR. A study result shows that only 1.3% of COVID-19 patients from the Intensive care unit and no other units got infected with nosocomial superinfection with AMR bacteria (Fattorini et al., 2020). Another study shows that only 3.5% of COVID-19 patients got bacterial coinfection (Langford et al., 2020). A significant decrease in international air travel also decreased AMR bacteria and genes (Kommenda, 2020; Murray, 2020).
RESISTANCE OF PATHOGENIC ORGANISMS TO INACTIVATING AGENTS
A considerable number of disinfectants containing antibiotics have been used in public. The high concentration of these disinfectants wastewater and the soil leads to environmental and aquatic toxicity and, in some cases, resistance to viruses (Chen et al., 2021; Wang et al., 2020b). Resistance poses a serious global concern, thereby exposing the vast, vulnerable population to devastating situations. Many disinfectants contain chlorine-releasing agents. Excessive use of these can give rise to chlorine-tolerant microbes, which are also competent cells and can more efficiently transfer plasmids (Jin et al., 2020). Therefore, it is pertinent to monitor disinfectants for potential risks of developing resistance due to the discriminate application of the agents during the pandemic period (Berardi et al., 2020; Dellanno et al., 2009; Okeke et al., 2005).
Moreover, the CDC and the European Committee for Standardization recommend methods and testing protocols for disinfectant preparations to effectively determine efficiency and inactivation potential against viruses, especially on enveloped viruses. This represents the vast majority of emerging infectious diseases. Therefore, it is recommended to use tested and well-recommended formulations such as PVP-I and ethanol preparations less susceptible to resistance development when used appropriately (Boyce and Pittet, 2002; Eggers, 2019). As discussed under iodine-based disinfecting products, PVP-I is one of the most widely used alternative antiseptics to alcohol prepared in clinical settings for disinfecting skin during and after surgical operations. It inactivates resistant strains of pathogenic microorganisms effectively (Gottrup et al., 2014). It was demonstrated by Eggers et al. (2018), that iodine has superior activity against enveloped and nonenveloped viruses (Table 7), hence its lack of cross-resistance among many pathogens. Besides its inability to develop resistance, PVP-I has been more effective and superior to chlorhexidine against pathogenic microorganisms, especially handwashing disinfectants (Eggers, 2019).
So far, no significant resistance has been acquired by iodine, mainly when used for specific purposes and stipulated procedures (Eggers, 2019). Iodine maintains equilibrium due to constant replacement by the PVP-bound iodine, leading to disruptions and leakage of the organism (Mayer et al., 2001). Therefore, the long-lasting efficacy and continuous supply of iodine during its action suggest decreased possibility of resistance developed by many pathogenic organisms (Eggers, 2019). In summary, PVP-I and ethanol preparations are less susceptible to resistance development when used appropriately and adequately. PVP-I’s constant equilibrium supply and efficacy during its action against viruses make it one of the disinfectants of choice for many decades. The development of resistance to various disinfectants and antimicrobial agents is demonstrated (Fig. 4).
 | Table 7. Comparison of anti-viral activities of standard antiseptic classes as indicated by Eggers et al. (2019). [Click here to view] |
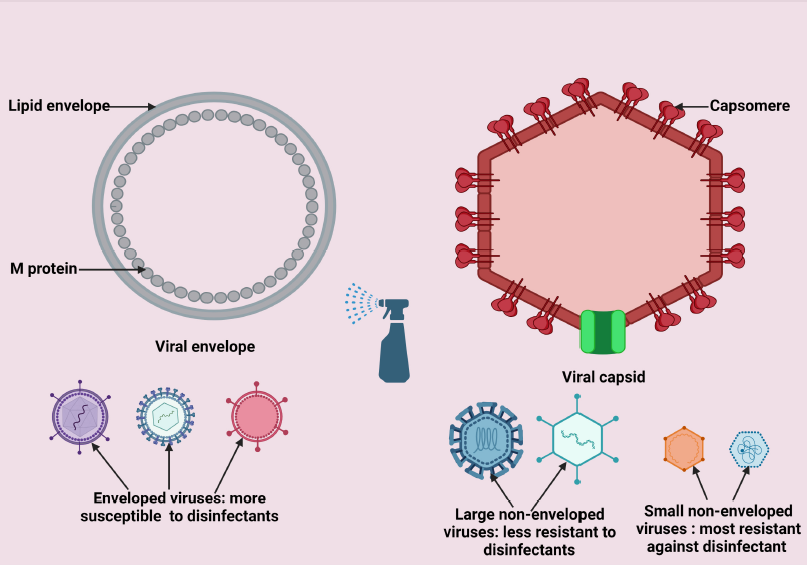
TOXICITY OF INACTIVATING AGENTS
The WHO’s declaration of COVID-19 as a global pandemic and misinformation on the public health emergency leads to misconceptions, rumors, and subsequently cynicism on the disease by some individuals (Xu and Li, 2020). In addition, misinformation on the use of disinfectants triggers panic, anxiety, and hysteria in people. Thus, individuals adopt inappropriate, excessive, and unethical actions such as the application of equipment sterilizers on the skin, washing food products with disinfectants, and in some instances, ingesting chemicals, all in the name of preventive measures. The SARS-CoV-2 pandemic has skyrocketed the demand for disinfectants globally, exposing human, environmental, and aquatic life to the toxic effects of these chemicals (Sefah et al., 2020). This could culminate in increasing secondary disasters detrimental to the fragile healthcare system (Rai et al., 2020). Residual chemicals left on the surfaces can be inhaled and cause serious health problems such as allergic reactions and asthma (Medina-Ramón et al., 2005). The long-term effect of such substances could be harmful to health, causing chronic diseases like cancer and central nervous system (CNS) impairment. Other effects include oxidative damage and reproductive disorders (Choi et al., 2020). Most of these cleaning agents contain harmful materials and are corrosive to both humans and the environment; therefore, caution and strict adherence to safety and protocol measures must be exercised when applying disinfecting agents on both humans and the environment (Arevalo-Silva et al., 2006; Nabi et al., 2020; Sawalha, 2007; Sharafi et al., 2020).
In humans, toxicity due to disinfectants is usually experienced upon long-term exposure to the agents through mouth, skin, and inhalation routes. The toxicological effects vary according to the course and the type of the disinfecting agent. For instance, alcohol-based disinfectants and sanitizers display short contact time on humans due to their volatility. They are considered less harmful than other less volatile agents with extended contact time. Therefore, alcohol-based disinfectants are mostly recommended for homes and hospitals (Li et al., 2020a). Other agents such as hypochlorous and peroxides are primarily used in dental clinics due to their ability to produce aerosols at a low cost to prevent contact with most patients (Scarano et al., 2020). It was reported that most chemical disinfectant by-products increased the risk of chronic obstructive pulmonary disease (COPD) like asthma and irritation of the eyes and skin, primarily when misused. Other hazards include cancers and reproductive and respiratory disorders (Chen et al., 2021; Rume and Islam, 2020; Sharafi et al., 2020). Children are the most affected when exposed to hazardous chemicals, with reported cases of dysbiosis in the infant gut leading to overweight and obesity (Chen et al., 2021). Excessive use of alcohol-based hand sanitizer as a protective measure for the current pandemic has caused alcohol toxicity (Ghafoor et al., 2021). It can also increase the risk of other viral infections such as norovirus outbreaks (Blaney et al., 2011). Some ABHR or sanitizers contain nonvolatile biocides such as benzalkonium chloride, chlorhexidine digluconate, didecyldimethylammonium chloride, polihexanide, triclosan, or octenidine dihydrochloride (Kampf, 2016). Although they do not have any proven health benefit or superior bactericidal efficacy, they can raise AMR (Kampf, 2016; Kampf et al., 2017; Palumbo et al., 2017). Chlorhexidine, povidone-iodine, benzalkonium chloride, or octenidine are used in some alcohol-based skin antiseptics (Kampf, 2016). Of these, only chlorhexidine and octenidine have proven health benefits in preventing infection despite some risks (Chaiyakunapruk et al., 2002; Darouiche et al., 2010; Dettenkofer et al., 2010; Harnoss et al., 2018; Mimoz et al., 2015; Tuuli et al., 2016). Other agents such as glutaraldehyde and ethylene oxide were also reported to cause severe lung disease (Dumas et al., 2019). Therefore, caution should be exercised, especially when mixtures of disinfectants are preferred. For instance, the combination of bleach with an acid-based cleaner could release gaseous chlorine or hypochlorous acid. When inhaled, even in small amounts, it may cause acute severe lung injury (Bracco et al., 2005). People are exposed to toxic effects of these chemicals with an increased risk of COPD, asthma, and eye irritation due to the knowledge gap in safe preparations of cleaning and disinfecting agents, even among adults. Therefore, discourage self-preparation without the requisite skills and knowledge (Casey et al., 2017; Dumas et al., 2019; Gharpure et al., 2020; Weinmann et al., 2019). Moreover, a study indicated that about 5% of cancer in children and 30% of childhood asthma are linked to long-term chemical exposures due to the inability to handle or use the chemicals properly and subsequently damaging essential organs in the body (Landrigan et al., 2002). Another necessary caution is excessive, frequent, and vigorous hand rubbing when using alcohol-based antiseptics, which could be inhaled and may generate potential threats to eyes and skin and subsequently lead to contact and allergic dermatitis to mild or moderate inflammatory effects (Shetty et al., 2020).
 | Figure 4. Processes of developing resistance by commonly used disinfectants and other antimicrobial agents. [Click here to view] |
During the COVID-19 pandemic, there was an increase in biomedical and untreated wastes (Wang et al., 2020b), which endangers both humans and the environment. Chlorine-based disinfectants are the most widely used agents on environments during the SARS-CoV-2 pandemic, thereby causing high residual concentrations in water bodies, soil, and the environment. Ultimately, these affect agricultural production due to excessive chlorine (Cl-), soil degradation, and ecosystem destruction. A high chlorine residue concentration on the soil affects the ecosystem by reacting with bromide in raw materials or soil and organic matter. This subsequently leads to disinfectants-by-products formations, especially trihalomethanes and bromides, toxic to the environment (soil), human, and aquatic animals (Srivastav et al., 2020). Chlorine-based disinfectants are prone to the formation of carcinogenic chloramines and nitrosamines, observed in drinking water around Washington D.C (Montazeri et al., 2017; National Research Council, 1980). However, chlorine-based disinfectants’ toxic effects on plants are short-lived and quickly neutralized by some organic matters in the soil (Montazeri et al., 2017). The aquatic animals are also endangered due to exposure to toxic by-products of the disinfecting chemicals (Nabi et al., 2020; Sharafi et al., 2020). Also, disinfecting water for consumption using chlorine produces products and, when used for the long-term, may be harmful to aquatic and human life, causing chronic diseases such as cancer (Agnelo et al., 2020; Srivastav et al., 2020). The excessive applications of disinfectants undoubtedly increase their presence within the ecosystem, causing air, water, and soil pollution.
In summary, even though some disinfectants are toxic to individuals and the environment, they are essential in curbing the spread of COVID-19. The vast majority of the disinfectants, such as alcohol and chlorine-based products, are mainly used on humans and the environment, respectively. Frequent exposure to disinfectants during the COVID-19 pandemic poses risks of chronic diseases such as cancers, respiratory, and reproductive disorders. Therefore, guidelines, procedures, and recommendations made by WHO, CDC, and other recognized health agencies should be followed to minimize the health risks associated with exposure to chemical disinfectants. Possible toxicity and other health hazards resulting from disinfectant use are demonstrated (Fig. 5).
MITIGATING STRATEGIES TO REDUCE THE TOXIC EFFECTS OF INACTIVATING AGENTS
The COVID-19 pandemic posed several challenges and seemed unmanageable through current preventive measures and strategies (Habas et al., 2020; Rahman et al., 2021). Disinfectants are essential prophylactic agents; however, there is indiscriminate disinfectant use during the pandemic. Despite having a beneficial role in controlling and preventing SARS-CoV-2, there are concerns regarding the large-scale use of disinfectants, including the toxic effect on human health and the chance of developing drug resistance. Various national and international healthcare authorities, that is, WHO (2020) and CDC (Government, 2021), have developed recommendations for the appropriate utilization of suitable disinfectants to prevent the pandemic.
The following essential mitigation strategies are recommended to reduce the toxic effects of disinfectants in humans and the environment (Chen, 2020; Dhama et al., 2021):
 | Figure 5. Demonstration of toxicity and health-related hazards by disinfecting agents. [Click here to view] |
1. Use of natural disinfectants, for example, sunlight and plant-based disinfectants.
2. Use only recommended dose of disinfection.
3. Substitute cleaning and disinfectant sprays with liquid products that are manually applied with a cloth.
4. Increase ventilation during and following treatment.
5. Follow label usage instructions and avoid mixing cleaning and disinfectant products.
6. Avoid using cleaning and disinfectant products around children.
7. Allow the area being treated to air out the following application.
8. Clearly label disinfectants and store them away from children and pets.
9. Avoid any accidental leakage of disinfectants into water.
10. Development of nanomaterials or nanoparticles for surface decontamination.
11. Improve personal protective equipment (PPE) worn by users.
12. Incorporation of nanobiotechnology to develop PPEs and sanitization.
13. Efficient disposal of PPEs and medical waste using techniques like incineration and vitrification.
14. Provide proper worker training in safe cleaning and disinfection practices.
15. Strictly follow national health and safety guidelines for using disinfectants.
CONCLUSION AND RECOMMENDATIONS
COVID-19 is a highly infectious and transmissible disease. The inability to detect symptoms within a few days of getting infected by individuals further complicates its proper prevention and disinfection process, especially in a frequented indoor space. Initially, when the disease was declared a public healthcare emergency by the WHO, different nations adopted temporary confinement of people indoor to curb the disease spread. Nonetheless, this policy has negatively impacted the global economies, individuals’ psychological and mental health, and the overwhelming healthcare system. Briefly, this article highlighted the relevance of physical inactivation, such as temperature and humidity, controlling the viral survival on the surfaces, and ultimately reducing the virus’s transmission through droplets. Although the SARS-CoV-2 is highly stable at 4°C, it becomes inactive when exposed to high temperatures. The UV radiation, incredibly the UV-C light, has also proven to effectively reduce air transmission of several pathogenic diseases, including airborne viruses, hence essential in curbing the spread of SARS-CoV-2. However, due to the harmful effects of UV radiation on normal cells, especially at high wavelengths, its use is limited.
Consequently, the application of UV radiation for the control of SARS-CoV-2 infection requires specifications with lesser health-damaging effects on humans and animals. Furthermore, the literature review emphasized the commonly used disinfectants during the SARS-CoV-2 pandemic, such as alcohol- and iodine-based products. The alcohol-based disinfectant represents the widest hand-rub antiseptics recommended by various health agencies and organizations, including the WHO and CDC, during the SARS-CoV-2 outbreak. The alcohol-based disinfectants are easily accessible and effective in preventing the spread of SARS-CoV-2. The iodine-based counterpart has also proven efficacious against many pathogenic microorganisms over many years. Most of its preparations demonstrated efficient virucidal activity against SARS-CoV-1, MERS-CoV, and SARS-CoV-2, suggesting its broad applicability on many viral diseases. However, a high concentration of these disinfectants in wastewater and the soil leads to environmental and aquatic toxicity and, in some cases, resistance to viruses. Notably, the residual chemical remaining on the surfaces or inhaled by individuals may have long-term effects on public health, such as reproductive disorders, COPD, cancers, skin damage, and CNS impairment. Therefore, further research on long-term preventive alternatives such as formulating disinfectants with natural products as active ingredients is necessary to mitigate the effects of alcohol- and iodine-based chemicals on humans and the environment.
Additionally, effective technologies and strategies need to be developed for minimizing these toxic effects and drug resistance. Safe, eco-friendly technologies should be used to produce safe, effective, and affordable disinfectants using nanotechnology and nanomedicine. Comprehensive guidelines for rational disinfectants are also necessary at regional, national, and international levels to reduce the toxic effects on humans and the environment.
PROFESSIONAL ANNOTATION
Disinfection pronounces a procedure that eradicates several or all infective microbes, excluding bacteriological spores, on nonliving objects (Baron et al., 1996; Basta and Annamaraju, 2020; Council, 1977; Protano et al., 2019; Rutala and Weber, 2008; Rutala and Weber, 2016). Nevertheless, sterilization labels a method that abolishes or exterminates all microbiological life forms and is regularly conducted in all sorts of healthcare facilities by physical or chemical approaches (Anderson et al., 2018; Ling et al., 2018; Protano et al., 2019; Rutala and Weber, 2008; Rutala and Weber, 2016). The disinfection of health professional hands is a significant avenue to transfer through healthcare providers. It was first noticed by the Hungarian Obstetrician Professor (Dr.) Ignaz Phillip Semmelweis in 1847 (Haque, 2020; Haque et al., 2018). Dr. Ignaz Phillip Semmelweis is primarily known as the father of infection control (Flynn, 2020; Habboush et al., 2021 a). The essential standing of hand sanitization and other issues in managing infection control has been similarly advocated by Florence Nightingale, Oliver Wendell Holmes, Louis Pasteur, Joseph Lister, and Robert Koch (Ataman et al., 2013; Gebel et al., 2013; Görig et al., 2019; Glass, 2014; Haque et al., 2020; Hillier, 2020; Kampf et al., 2009; La Rochelle and Julien, 2013; Lane et al., 2010; Pitt and Aubin, 2012; Smith et al., 2012; Tulchinsky and Varavikova, 2014; Tyagi and Barwal, 2020; Worboys, 2013). After that, the importance of hand hygiene practice was validated through multiple scientific works and remains essential and pertinent (Allegranzi and Pittet, 2009; Magiorakos et al., 2010; Mathur, 2011; Reichardt et al., 2013).
Healthcare-associated infections (HCAIs) and community infections remain safety concerns for health professionals and patients (Monegro et al., 2021). Thereby, it increases considerable morbidity and mortality and prolongs the hospital stay and healthcare overhead length (Badia et al., 2017; Grant et al., 2017; Jia et al., 2019; Zhou et al., 2019). Therefore, multiple studies revealed that efforts need to promote infection preventive strategies in all healthcare facilities and communities to avert infection and maximize healthcare benefits (Cheung et al., 2019; Schmid et al., 2018; Wagh and Sinha, 2018; Worth et al., 2018). Infection management denotes the strategy and measures to be implemented to curb and curtail the spreading and propagation of HCAIs infections in different types of healthcare facilities that include ambulatory surgical centers, birth centers, blood banks, clinics, and medical offices, diabetes education centers, dialysis centers, hospice homes, hospitals, primary healthcare centers, imaging and radiology centers, mental health and addiction treatment centers, nursing homes, orthopedic and other rehabilitation centers, urgent care, telehealth, and communities (Boev and Kiss, 2017; Collins, 2008; Gandra and Ellison, 2014; Guzman, 2021; Haque et al., 2018; Hsu, 2014). The infection control strategy was reported as a well-established practice in US hospitals in the early 1950s (Dixon, 2011; Habboush et al., 2021a; Monegro et al., 2021). Additionally, multiple pieces of research revealed that efficient practice infection prevention program reduces morbidity, mortality, healthcare financial overhead, and disability-adjusted life years (DALYs) and maximizes proper utilization of healthcare (De la Rosa-Zamboni et al., 2018; Friedrich, 2019; La Rochelle and Julien, 2013; Zacher et al., 2019). The health management system progressively recognizes the importance of surface disinfection (Gebel et al., 2013). Notwithstanding, several unanswered questions remain to be determined (Gebel et al., 2013).
Surface disinfection is an essential procedure in healthcare facilities and infectious diseases such as COVID-19. It is vital to curbing contagious diseases and reducing the risk of direct and indirect contact transmission from healthcare personnel to patients. This could decrease surfaces to act as reservoirs for various infectious diseases (Donskey, 2013). For many years, alcohol-based preparations have been used as low-level disinfectants in hospitals against bacteria. Recently, a combination of alcohol-based and QACs was used to disinfect surfaces against Ebola viruses and several coronaviruses. The antiseptic preparations are used due to their ability to evaporate rapidly and short contact time on the skin, therefore, less damaging the skin due to lesser exposure to the agents (Boyce, 2018). Most of these disinfectants, such as chlorine-based, are inexpensive and readily available in rural and urban areas (Gallandat et al., 2021). However, disinfections are necessary to inactive and reduce the viral load on surfaces. However, many disadvantages follow. The high amount of surface disinfectants is corrosive to the environment, especially iodine-based disinfectants. Also, most of these disinfectants cause irritation when applied in high concentrations and on stain surfaces and can be quickly inactivated by organic matter (Gallandat et al., 2021).
Moreover, some disinfecting agents have antibacterial agents in their formulation; inappropriate exposure to bacteria could cause bacterial resistance development (Chen et al., 2021). In some cases, prolonged exposure to these disinfectants could cause serious health problems such as cancers, respiratory problems, and genetic defects in an unborn baby (Ahmed-Lecheheb et al., 2012; Choi et al., 2020). In most cases, not all disinfectants products eradicate the coronaviruses. Therefore, further investigation on individual disinfecting agents is required to validate their merit and demerit potentials further.
DECLARATIONS
Ethics approval and consent to participate: This is a review paper. Thereby does not require Institutional Review Board’s approval and consent.
ACKNOWLEDGMENT
The corresponding author is grateful to Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kem Perdana Sungai Besi, 57000 Kuala Lumpur, Malaysia.
AUTHORS’ CONTRIBUTION
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
FUNDING
This paper was not funded.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
CONSENT FOR PUBLICATIONS
All authors reviewed and approved the final version and have agreed to be accountable for all aspects of the work, including any issues related to accuracy or integrity.
COMPETING INTEREST
The authors declare that they have no competing interests.
ABBREVIATIONS
AMR: Antimicrobial resistance
CNS: Central nervous system
CDC: Centre for Disease Control and Prevention
CNKI: China National Knowledge Infrastructure
DNA: Deoxyribonucleic acid
RNA: Ribonucleic acid
COPD: Chronic obstructive pulmonary disease
HCPs: Healthcare professionals
HCoVs: Human coronaviruses
MERS-CoV: Middle East Respiratory-Corona Virus
UV: Ultraviolet
SARS-CoV-1: Severe acute respiratory syndrome corona virus-1
SARS-CoV-2: Severe acute respiratory syndrome corona virus-2
TGEV: Transmissible gastroenteritis coronavirus of pigs, a SARS-CoV surrogate
MHV: Mouse hepatitis virus
CCoV: Canine coronavirus
ATCC: American Type Culture Collection
PVP-I: Polyvinylpyrrolidone
EMC: Erasmus Medical Center
QACs: Quaternary ammonium compounds
REFERENCES
Abad FX, Pintó RM, Bosch A. Disinfection of human enteric viruses on fomites. FEMS Microbiol Lett, 1997; 156(1):107–11. CrossRef
Abelenda-Alonso G, Padullés A, Rombauts A, Gudiol C, Pujol M, Alvarez-Pouso C, Jodar R, Carratalà J. Antibiotic prescription during the COVID-19 pandemic: a biphasic pattern. Infect Control Hosp Epidemiol, 2020; 41(11):1371–2. CrossRef
Abraham JP, Plourde BD, Cheng L. Using heat to kill SARS-CoV-2. Rev Med Virol, 2020; 30(5):e2115. CrossRef
Abraham JP, Plourde BD, Minkowycz WJ. Continuous flow solar thermal pasteurization of drinking water: methods, devices, microbiology, and analysis. Renew Energy, 2015; 81:795–803. CrossRef
Abubakar AR, Sani IH, Godman B, Kumar S, Islam S, Jahan I, Haque M. Systematic Review on the therapeutic options for COVID-19: clinical evidence of drug efficacy and implications. Infect Drug Resist, 2020; 13:4673–95. CrossRef
Agnelo L, Leonel LP, Silva NB, Candello FP, Schneider J, Tonetti AL. Effects of wastewater disinfectants on the soil: Implications for soil microbial and chemical attributes. Sci Total Environ, 2020; 706:136007. CrossRef
Ahmed-Lecheheb D, Cunat L, Hartemann P, Hautemaniere A. Prospective observational study to assess hand skin condition after application of alcohol-based hand rub solutions. Am J Infect Control, 2012; 40(2):160–4. CrossRef
Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect, 2009; 73(4):305–15. CrossRef
Al-Sayah MH. Chemical disinfectants of COVID-19: an overview. J Water Health, 2020; 18(5):843–8. CrossRef
Alvarez ME, O’Brien RT. Mechanisms of inactivation of poliovirus by chlorine dioxide and iodine. Appl Environ Microbiol, 1982; 44(5):1064–71. CrossRef
Amanat F, Krammer F. SARS-CoV-2 Vaccines: status report. Immunity, 2020; 52(4):583–9. CrossRef
Anderson DE, Sivalingam V, Kang AEZ, Ananthanarayanan A, Arumugam H, Jenkins TM, Hadjiat Y, Eggers M. Povidone-iodine demonstrates rapid in vitro virucidal activity against SARS-CoV-2, the virus causing COVID-19 disease. Infect Dis Ther, 2020; 9(3):669–75. CrossRef
Anderson DJ, Moehring RW, Weber DJ, Lewis SS, Chen LF, Schwab JC, Becherer P, Blocker M, Triplett PF, Knelson LP, Lokhnygina Y, Rutala WA, Sexton DJ; CDC Prevention Epicenters Program. Effectiveness of targeted enhanced terminal room disinfection on hospital-wide acquisition and infection with multidrug-resistant organisms and Clostridium difficile: a secondary analysis of a multicentre cluster randomized controlled trial with crossover design (BETR Disinfection). Lancet Infect Dis, 2018; 18(8):845–53; doi: 10.1016/S1473-3099(18)30278-0 CrossRef
Anpilov AM, Barkhudarov EM, Christofi N, Kop’ev VA, Kossyi IA, Taktakishvili MI, Zadiraka Y. Pulsed high voltage electric discharge disinfection of microbially contaminated liquids. Lett Appl Microbiol, 2002; 35(1):90–4. CrossRef
Ao XW, Eloranta J, Huang CH, Santoro D, Sun WJ, Lu ZD, Li C. Peracetic acid-based advanced oxidation processes for decontamination and disinfection of water: a review. Water Res, 2021; 188:116479. CrossRef
Arevalo-Silva C, Eliashar R, Wohlgelernter J, Elidan J, Gross M. Ingestion of caustic substances: a 15-year experience. Laryngoscope, 2006; 116(8):1422–6. CrossRef
Armstrong JA, Froelich EJ. Inactivation of viruses by benzalkonium chloride. Appl Microbiol, 1964; 12(2):132–7. CrossRef
Asadi S, Bouvier N, Wexler AS, Ristenpart WD. The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles? Aerosol Sci Technol, 2020; 54(6):1–4. CrossRef
Ataman AD, Vatano?lu-Lutz EE, Y?ld?r?m G. Medicine in stamps-Ignaz Semmelweis and Puerperal Fever. J Turk Ger Gynecol Assoc, 2013; 14(1):35–9. CrossRef
Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod, 2020; 46(5):584–95. CrossRef
Ayipo YO, Yahaya SN, Alananzeh WA, Babamale HF, Mordi MN. Pathomechanisms, therapeutic targets, and potent inhibitors of some beta-coronaviruses from bench-to-bedside. Infect Genet Evol, 2021:104944. CrossRef
Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect, 2017; 96(1):1–15; doi: 10.1016/j.jhin.2017.03.004 CrossRef
Banik GR, Khandaker G, Rashid H. Middle East respiratory syndrome coronavirus “MERS-CoV”: current knowledge gaps. Paediatr Respir Rev, 2015; 16(3):197–202. CrossRef
Baron S, editor. Medical microbiology. 4th edition, University of Texas Medical Branch, Galveston, TX, 1996. Available via https://www.ncbi.nlm.nih.gov/books/NBK7627/ (Accessed 24 June 2021).
Basta M, Annamaraju P. Bacterial Spores. [Updated 2021 Feb 9]. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021. Available via https://www.ncbi.nlm.nih.gov/books/NBK556071/ (Accessed 24 Jun 2021).
Baye AM, Ababu A, Bayisa R, Abdella M, Diriba E, Wale M, Selam MN. Perspectives of compounding pharmacists on alcohol-based hand sanitizer production and utilization for COVID-19 prevention in Addis Ababa, Ethiopia: a descriptive phenomenology study. PLoS One, 2021; 16(4):e0250020. CrossRef
Beck SE, Ryu H, Boczek LA, Cashdollar JL, Jeanis KM, Rosenblum JS, Lawal OR, Linden KG. Evaluating UV-C LED disinfection performance and investigating potential dual-wavelength synergy. Water Res, 2017; 109:207–16. CrossRef
Bedell K, Buchaklian AH, Perlman S. Efficacy of an automated multiple emitter whole-room ultraviolet-C disinfection system against coronaviruses MHV and MERS-CoV. Infect Control Hosp Epidemiol, 2016; 37(5):598–9; doi:10.1017/ice.2015.348 CrossRef
Benzoni T, Hatcher JD. Bleach toxicity. [Updated 2021 Jun 29]. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021. Available via https://www.ncbi.nlm.nih.gov/books/NBK441921/ (Accessed July 2021).
Beovi? B, Doušak M, Ferreira-Coimbra J, Nadrah K, Rubulotta F, Belliato M, Berger-Estilita J, Ayoade F, Rello J, Erdem H. Antibiotic use in patients with COVID-19: a ‘snapshot’ Infectious Diseases International Research Initiative (ID-IRI) survey. J Antimicrob Chemother, 2020; 75(11):3386–90. CrossRef
Berardi A, Perinelli DR, Merchant HA, Bisharat L, Basheti IA, Bonacucina G, Cespi M, Palmieri GF. Hand sanitizers amid CoViD-19: a critical review of alcohol-based products on the market and formulation approaches to respond to increasing demand. Int J Pharm, 2020; 584:119431. CrossRef
Bidra AS, Pelletier JS, Westover JB, Frank S, Brown SM, Tessema B. Rapid In-vitro inactivation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using povidone-iodine oral antiseptic rinse. J Prosthodont, 2020a; 29(6):529–33. CrossRef
Bidra AS, Pelletier JS, Westover JB, Frank S, Brown SM, Tessema B. Comparison of in vitro inactivation of SARS CoV-2 with hydrogen peroxide and povidone-iodine oral antiseptic rinses. J Prosthodont, 2020b; 29(7):599–603. CrossRef
Biryukov A, Gavrikov V, Nikiforova L, Shcheglov V. New physical methods of disinfection of water. J Russian Laser Res, 2005; 26(1):13–25. CrossRef
Blaney DD, Daly ER, Kirkland KB, Tongren JE, Kelso PT, Talbot EA. Use of alcohol-based hand sanitizers as a risk factor for norovirus outbreaks in long-term care facilities in northern New England: December 2006 to March 2007. Am J Infect Control, 2011; 39(4):296–301. CrossRef
Block SS. Disinfection, sterilization, and preservation. Lippincott Williams & Wilkins, Philadelphia, PA, 2001. Available via https://books.google.com.my/books (Accessed July 2021).
Boev C, Kiss E. Hospital-acquired infections: current trends and prevention. Crit Care Nurs Clin North Am, 2017; 29(1):51–65. CrossRef
Bond WW, Favero MS, Petersen NJ, Ebert JW. Inactivation of hepatitis B virus by intermediate-to-high-level disinfectant chemicals. J Clin Microbiol, 1983; 18(3):535–8; doi: 10.1128/jcm.18.3.535-538.1983 CrossRef
Boyce JM. Alcohols as surface disinfectants in healthcare settings. Infect Control Hosp Epidemiol, 2018; 39(3):323–8. CrossRef
Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep, 2002; 51(Rr-16):1–45, quiz CE41-44.
Bracco D, Dubois MJ, Bouali R. Intoxication by bleach ingestion. Can J Anaesth, 2005; 52(1):118-9. CrossRef
Brown AN, Strobel G, Hanrahan KC, Sears J. Antiviral activity of the propylamylatin(TM) formula against the novel coronavirus SARS-CoV-2 in vitro using direct injection and gas assays in virus suspensions. Viruses, 2021; 13(3):415. CrossRef
Cabrera-Martinez RM, Setlow B, Setlow P. Studies on the mechanisms of the sporicidal action of ortho-phthalaldehyde. J Appl Microbiol, 2002; 92(4):675–80. CrossRef
Carr AC, van den Berg JJ, Winterbourn CC. Chlorination of cholesterol in cell membranes by hypochlorous acid. Arch Biochem Biophys, 1996; 332(1):63–9. CrossRef
Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol, 2010; 76(9):2712–7. CrossRef
Casey ML, Hawley B, Edwards N, Cox-Ganser JM, Cummings KJ. Health problems and disinfectant product exposure among staff at a large multispecialty hospital. Am J Infect Control, 2017; 45(10):1133–8. CrossRef
Castaño N, Cordts SC, Kurosu Jalil M, Zhang KS, Koppaka S, Bick AD, Paul R, Tang SKY. Fomite transmission, physicochemical origin of virus-surface interactions, and disinfection strategies for enveloped viruses with applications to SARS-CoV-2. ACS Omega, 2021; 6(10):6509–27. CrossRef
Cegolon L, Javanbakht M, Mastrangelo G. Nasal disinfection for the prevention and control of COVID-19: A scoping review on potential chemo-preventive agents. Int J Hyg Environ Health, 2020; 230:113605. CrossRef
Chaiyakunapruk N, Veenstra DL, Lipsky BA, Saint S. Chlorhexidine compared with povidone-iodine solution for vascular catheter site care: a meta-analysis. Ann Intern Med, 2002; 136(11):792–801. CrossRef
Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Lo SK, Chan KH, Poon VK, Chan WM, Ip JD, Cai JP, Cheng VC, Chen H, Hui CK, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet, 2020; 395(10223):514–23. CrossRef
Chen CJ, Chen CC, Ding SJ. Effectiveness of hypochlorous acid to reduce the biofilms on titanium alloy surfaces in vitro. Int J Mol Sci, 2016; 17(7). CrossRef
Chen T. A rapid review of disinfectant chemical exposures and health effects during COVID-19 pandemic. national collaborating center for environmental health, pp 1–25, 2020. Available via https://ncceh.ca/documents/field-inquiry/rapid-review-disinfectant-chemical-exposures-and-health-effects-during (Accessed 20 August 2021).
Chen Z, Guo J, Jiang Y, Shao Y. High concentration and high dose of disinfectants and antibiotics used during the COVID-19 pandemic threaten human health. Environ Sci Eur, 2021; 33(1):11. CrossRef
Chernyshov PV, Kolodzinska L. Prospective study on hand dermatitis in nurses and doctors during COVID-19 pandemic and its improvement by use of adopted recommendations of the European Academy of Dermatology and Venereology Task Force on Contact Dermatitis. Dermatol Ther, 2020; 33(6):e14396. CrossRef
Cheung R, Roland D, Lachman P. Reclaiming the systems approach to pediatric safety. Arch Dis Child, 2019; 104(12):1130–3. CrossRef
Chin AWH, Chu JTS, Perera MRA, Hui KPY, Yen HL, Chan MCW, Peiris M, Poon LLM. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe, 2020; 1(1):e10. CrossRef
Choi H, Chatterjee P, Coppin JD, Martel JA, Hwang M, Jinadatha C, Sharma VK. Current understanding of the surface contamination and contact transmission of SARS-CoV-2 in healthcare settings. Environ Chem Lett, 2021:1–10. CrossRef
Choi HY, Lee YH, Lim CH, Kim YS, Lee IS, Jo JM, Lee HY, Cha HG, Woo HJ, Seo DS. Assessment of respiratory and systemic toxicity of Benzalkonium chloride following a 14-day inhalation study in rats. Part Fibre Toxicol, 2020;17(1):5. CrossRef
Clasen T, Edmondson P. Sodium dichloroisocyanurate (NaDCC) tablets as an alternative to sodium hypochlorite for the routine treatment of drinking water at the household level. Int J Hyg Environ Health, 2006; 209(2):173–81. CrossRef
Cleary SJ, Pitchford SC, Amison RT, Carrington R, Robaina Cabrera CL, Magnen M, Looney MR, Gray E, Page CP. Animal models of mechanisms of SARS-CoV-2 infection and COVID-19 pathology. Br J Pharmacol, 2020; 177(21):4851–65. CrossRef
Coates D, Wilson M. Use of sodium dichloroisocyanurate granules for spills of body fluids. J Hosp Infect, 1989; 13(3):241–51. CrossRef
Collins AS. Preventing Health Care-Associated Infections. In: Hughes RG (ed.). Patient safety and quality: an evidence-based handbook for nurses. Agency for Healthcare Research and Quality (US), Rockville, MD, 2008, Chapter 41. Available via https://www.ncbi.nlm.nih.gov/books/NBK2683/ (Accessed 26 June 2021). CrossRef
Costa S, Costa C, Madureira J, Valdiglesias V, Teixeira-Gomes A, Guedes de Pinho P, Laffon B, Teixeira JP. Occupational exposure to formaldehyde and early biomarkers of cancer risk, immunotoxicity, and susceptibility. Environ Res, 2019; 179(Pt A):108740.
Crum L. Sonoluminescence, sonochemistry, and sonophysics. J Acoustical Soc Am, 1994; 95(1):559–62. CrossRef
Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, Miller HJ, Awad SS, Crosby CT, Mosier MC, Alsharif A, Berger DH. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med, 2010; 362(1):18–26. CrossRef
De la Rosa-Zamboni D, Ochoa SA, Laris-González A, Cruz-Córdova A, Escalona-Venegas G, Pérez-Avendaño G, Torres-García M, Suaréz-Mora R, Castellanos-Cruz C, Sánchrez-Flores YV, Vázquez-Flores A, Águila-Torres R, Parra-Ortega I, Klünder-Klünder M, Arellano-Galindo J, Hernández-Castro R, Xicohtencatl-Cortes J. Everybody hands-on to avoid ESKAPE: effect of sustained hand hygiene compliance on healthcare-associated infections and multidrug resistance in a paediatric hospital. J Med Microbiol, 2018; 67(12):1761–71. CrossRef
Dellanno C, Vega Q, Boesenberg D. The antiviral action of common household disinfectants and antiseptics against murine hepatitis virus, a potential surrogate for SARS coronavirus. Am J Infect Control, 2009; 37(8):649–52. CrossRef
Dennis Jr W, Olivieri V, Kruse C. Mechanism of disinfection: incorporation of Cl-36 into f2 virus. Water Res, 1979; 13(4):363–9. CrossRef
Derraik JGB, Anderson WA, Connelly EA, Anderson YC. Rapid review of SARS-CoV-1 and SARS-CoV-2 viability, susceptibility to treatment, and the disinfection and reuse of PPE, particularly filtering facepiece respirators. Int J Environ Res Public Health, 2020; 17(17): 6117. CrossRef
Dettenkofer M, Wilson C, Gratwohl A, Schmoor C, Bertz H, Frei R, Heim D, Luft D, Schulz S, Widmer AF. Skin disinfection with octenidine dihydrochloride for central venous catheter site care: a double-blind, randomized, controlled trial. Clin Microbiol Infect, 2010; 16(6):600–6. CrossRef
Dhama K, Patel SK, Kumar R, Masand R, Rana J, Yatoo MI, Tiwari R, Sharun K, Mohapatra RK, Natesan S, Dhawan M, Ahmad T, Emran TB, Malik YS, Harapan H. The role of disinfectants and sanitizers during COVID-19 pandemic: advantages and deleterious effects on humans and the environment. Environ Sci Pollut Res Int, 2021; 28(26):34211–28. CrossRef
Diegritz C, Manhart J, Bücher K, Grabein B, Schuierer G, Kühnisch J, Kunzelmann KH, Hickel R, Fotiadou C. A detailed report on the measures taken in the Department of Conservative Dentistry and Periodontology in Munich at the beginning of the COVID-19 outbreak. Clin Oral Investig, 2020; 24(8):2931–41. CrossRef
Dixon RE. Control of health-care-associated infections, 1961–2011. MMWR Suppl, 2011; 60(4):58–63.
Donaghy JA, Jagadeesan B, Goodburn K, Grunwald L, Jensen ON, Jespers AD, Kanagachandran K, Lafforgue H, Seefelder W, Quentin MC. Relationship of sanitizers, disinfectants, and cleaning agents with antimicrobial resistance. J Food Prot, 2019; 82(5):889–902. CrossRef
Donskey CJ. Does improving surface cleaning and disinfection reduce healthcare-associated infections? Am J Infect Control, 2013; 41(5 Suppl):S12–9. CrossRef
Dumas O, Varraso R, Boggs KM, Quinot C, Zock JP, Henneberger PK, Speizer FE, Le Moual N, Camargo CA Jr. Association of occupational exposure to disinfectants with incidence of chronic obstructive pulmonary disease among US female nurses. JAMA Netw Open, 2019; 2(10):e1913563. CrossRef
Eggers M. Infectious disease management and control with povidone iodine. Infect Dis Ther, 2019; 8(4):581–93. CrossRef
Eggers M, Eickmann M, Zorn J. Rapid and effective virucidal activity of povidone-iodine products against middle east respiratory syndrome coronavirus (MERS-CoV) and modified vaccinia virus ankara (MVA). Infect Dis Ther, 2015; 4(4):491–501. CrossRef
Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther, 2018a; 7(2):249–59. CrossRef
Eggers M, Koburger-Janssen T, Ward LS, Newby C, Müller S. Bactericidal and virucidal activity of povidone-iodine and chlorhexidine gluconate cleansers in an in vivo hand hygiene clinical simulation study. Infect Dis Ther, 2018b; 7(2):235–47. CrossRef
Emmoth E, Ottoson J, Albihn A, Belák S, Vinnerås B. Ammonia disinfection of hatchery waste for elimination of single-stranded RNA viruses. Appl Environ Microbiol, 2011; 77(12):3960–6. CrossRef
Fattorini L, Creti R, Palma C, Pantosti A; Unit of Antibiotic Resistance and Special Pathogens; Unit of Antibiotic Resistance and Special Pathogens of the Department of Infectious Diseases, Istituto Superiore di Sanità, Rome. Bacterial coinfections in COVID-19: an underestimated adversary. Ann Ist Super Sanita, 2020; 56(3):359–64.
Fleming H. Effect of high-frequency fields on micro-organisms. Electric Eng, 1944; 63(1):18–21. CrossRef
Flint EB, Suslick KS. The temperature of cavitation. Science, 1991; 253(5026):1397–9. CrossRef
Frey W, Gusbeth C, Schwartz T. Inactivation of Pseudomonas putida by pulsed electric field treatment: a study on the correlation of treatment parameters and inactivation efficiency in the short-pulse range. J Membrane Biol, 2013; 246(10):769–81. CrossRef
Friedrich AW. Control of hospital-acquired infections and antimicrobial resistance in Europe: the way to go. Wien Med Wochenschr, 2019; 169(Suppl 1):25–30. CrossRef
Gallandat K, Kolus RC, Julian TR, Lantagne DS. A systematic review of chlorine-based surface disinfection efficacy to inform recommendations for low-resource outbreak settings. Am J Infect Control, 2021; 49(1):90–103. CrossRef
Gandra S, Ellison RT, 3rd. Modern trends in infection control practices in intensive care units. J Intensive Care Med, 2014; 29(6):311–26. CrossRef
Garcia de Abajo FJ, Hernandez RJ, Kaminer I, Meyerhans A, Rosell-Llompart J, Sanchez-Elsner T. Back to normal: an old physics route to reduce SARS-CoV-2 transmission in indoor spaces. ACS Nano, 2020; 14(7):7704–13. CrossRef
Gebel J, Exner M, French G, Chartier Y, Christiansen B, Gemein S, Goroncy-Bermes P, Hartemann P, Heudorf U, Kramer A, Maillard JY, Oltmanns P, Rotter M, Sonntag HG. The role of surface disinfection in infection prevention. GMS Hyg Infect Control, 2013; 8(1):Doc10.
Geller C, Fontanay S, Mourer M, Dibama HM, Regnouf-de-Vains JB, Finance C, Duval RE. Antiseptic properties of two Calix [4]arenes derivatives on the human coronavirus 229E. Antiviral Res, 2010; 88(3):343–6. CrossRef
Gerba CP. Quaternary ammonium biocides: efficacy in application. Appl Environ Microbiol, 2015; 81(2):464–9. CrossRef
Ghafoor D, Khan Z, Khan A, Ualiyeva D, Zaman N. Excessive use of disinfectants against COVID-19 posing a potential threat to living beings. Curr Res Toxicol, 2021; 2:159–68. CrossRef
Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, Berling K, Mercante JW, Murphy JL, Garcia-Williams AG. Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention—United States, May 2020. MMWR Morb Mortal Wkly Rep, 2020; 69(23):705–9. CrossRef
Glass GE. Beyond antisepsis: examining the relevance of the works of Joseph Baron Lister to the contemporary surgeon-scientist. Indian J Plast Surg, 2014; 47(3):407–11. CrossRef
Gogate PR. Hydrodynamic cavitation for food and water processing. Food Bioprocess Technol, 2011; 4(6):996–1011. CrossRef
Gogate PR, Pandit AB. Cavitation generation and usage without ultrasound: hydrodynamic cavitation. Theoretical and experimental sonochemistry involving inorganic systems. Springer, Dordrecht, The Netherlands, p 69–106, 2010. doi:10.1007/978-90-481-3887-6_3 CrossRef
Gold NA, Mirza TM, Avva U. Alcohol Sanitizer. [Updated 2021 Jun 26]. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021. Available via https://www.ncbi.nlm.nih.gov/books/NBK513254/ (Accessed July 2021).
Görig T, Dittmann K, Kramer A, Heidecke CD, Diedrich S, Hübner NO. Active involvement of patients and relatives improves subjective adherence to hygienic measures, especially self-reported hand hygiene: Results of the AHOI pilot study. Antimicrob Resist Infect Control, 2019; 8:201. CrossRef
Gottrup F, Apelqvist J, Bjarnsholt T, Cooper R, Moore Z, Peters EJ, Probst S. Antimicrobials and Non-Healing Wounds. Evidence, controversies, and suggestions-key messages. J Wound Care, 2014; 23(10):477–8, 480, 482. CrossRef
Gottsauner MJ, Michaelides I, Schmidt B, Scholz KJ, Buchalla W, Widbiller M, Hitzenbichler F, Ettl T, Reichert TE, Bohr C, Vielsmeier V, Cieplik F. A prospective clinical pilot study on the effects of a hydrogen peroxide mouthrinse on the intraoral viral load of SARS-CoV-2. Clin Oral Investig, 2020; 24(10):3707–13. CrossRef
Government of the District of Columbia. Coronavirus 2019 (COVID-19): guidance on Routine Cleaning and Disinfection for Community Facilities, 2021. Available via https://coronavirus.dc.gov/sites/default/files/dc/sites/coronavirus/page_content/attachments/Guidance-on-Routine-Cleaning-and-Disinfection-for-Community-Facilities.pdf (Accessed 23 June 2021).
Goyal SM, Chander Y, Yezli S, Otter JA. Evaluating the virucidal efficacy of hydrogen peroxide vapor. J Hosp Infect, 2014; 86(4):255–. CrossRef
Grant MC, Yang D, Wu CL, Makary MA, Wick EC. Impact of enhanced recovery after surgery and fast track surgery pathways on healthcare-associated infections: results from a systematic review and meta-analysis. Ann Surg, 2017; 265(1):68–79. CrossRef
Green NG, Morgan H, Milner JJ. Manipulation and trapping of sub-micron bioparticles using dielectrophoresis. J Biochem Biophys Methods, 1997; 35(2):89–102. CrossRef
Gusbeth C, Frey W, Volkmann H, Schwartz T, Bluhm H. Pulsed electric field treatment for bacteria reduction and its impact on hospital wastewater. Chemosphere, 2009; 75(2):228–33. CrossRef
Guzman BV, Elbel B, Jay M, Messito MJ, Curado S. Age-dependent association of obesity with COVID-19 severity in paediatric patients. Pediatr Obes, 2021:e12856. CrossRef
Habas K, Nganwuchu C, Shahzad F, Gopalan R, Haque M, Rahman S, Majumder AA, Nasim T. Resolution of coronavirus disease 2019 (COVID-19). Expert Rev Anti Infect Ther, 2020; 18(12):1201–11. CrossRef
Habboush Y, Yarrarapu SNS, Guzman N. Infection Control. Updated 2021 Jan 5]. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021a. Available via https://www.ncbi.nlm.nih.gov/books/NBK19017/ (Accessed 26 June 2021).
Habboush Y, Benham MD, Louie T, Noor A, Sprague RM. New York State infection control. 2021 Aug 22. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021b. PMID: 33351423.
Haque M, McKimm J, Sartelli M, Dhingra S, Labricciosa FM, Islam S, Jahan D, Nusrat T, Chowdhury TS, Coccolini F, Iskandar K, Catena F, Charan J. Strategies to prevent healthcare-associated infections: a narrative overview. Risk Manag Healthc Policy, 2020; 13:1765–80. CrossRef
Haque M, Sartelli M, McKimm J, Abu Bakar M. Healthcare-associated infections—an overview. Infect Drug Resist, 2018; 11:2321–3. CrossRef
Haque M. Handwashing in averting infectious diseases: Relevance to COVID-19. J Popul Ther Clin Pharmacol, 2020; 27(S Pt 1):e37–e52. CrossRef
Harnoss JC, Assadian O, Kramer A, Probst P, Müller-Lantzsch C, Scheerer L, Bruckner T, Diener MK, Büchler MW, Ulrich AB. Comparison of chlorhexidine-isopropanol with isopropanol skin antisepsis for prevention of surgical-site infection after abdominal surgery. Br J Surg, 2018; 105(7):893–9. CrossRef
Hassandarvish P, Tiong V, Mohamed NA, Arumugam H, Ananthanarayanan A, Qasuri M, Hadjiat Y, Abubakar S. In vitro virucidal activity of povidone-iodine gargle and mouthwash against SARS-CoV-2: implications for dental practice. Br Dent J, 2020 Dec 10:1–4. CrossRef
Hernández-Navarrete MJ, Celorrio-Pascual JM, Lapresta Moros C, Solano Bernad VM. Fundamentos de antisepsia, desinfección y esterilización [Principles of antisepsis, disinfection and sterilization]. Enferm Infecc Microbiol Clin, 2014; 32(10):681–8 [Spanish]. CrossRef
Hillier MD. Using effective hand hygiene practice to prevent and control infection. Nurs Stand, 2020; 35(5):45–50. CrossRef
Hindawi SI, Hashem AM, Damanhouri GA, El-Kafrawy SA, Tolah AM, Hassan AM, Azhar EI. Inactivation of Middle East respiratory syndrome-coronavirus in human plasma using amotosalen and ultraviolet A light. Transfusion, 2018; 58(1):52–9. CrossRef
Hong SM, Park JK, Lee YO. Mechanisms of microwave irradiation involved in the destruction of fecal coliforms from biosolids. Water Res, 2004; 38(6):1615–25. CrossRef
Hsu V. Prevention of healthcare-associated infections. Am Fam Phys, 2014; 90(6):377–82.
Hulkower RL, Casanova LM, Rutala WA, Weber DJ, Sobsey MD. Inactivation of surrogate coronaviruses on hard surfaces by health care germicides. Am J Infect Control, 2011; 39(5):401–7. CrossRef
Ijaz MK, Nims RW, Zhou SS, Whitehead K, Srinivasan V, Kapes T, Fanuel S, Epstein JH, Daszak P, Rubino JR, McKinney J. Microbicidal actives with virucidal efficacy against SARS-CoV-2 and other beta- and alpha-coronaviruses and implications for future emerging coronaviruses and other enveloped viruses. Sci Rep, 2021; 11(1):5626. CrossRef
Inagaki H, Saito A, Sugiyama H, Okabayashi T, Fujimoto S. Rapid inactivation of SARS-CoV-2 with deep-UV LED irradiation. Emerg Microbes Infect, 2020; 9(1):1744–7. CrossRef
Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 Transmission in dental practice: brief review of preventive measures in Italy. J Dent Res, 2020; 99(9):1030–8. CrossRef
Jamal M, Shah M, Almarzooqi SH, Aber H, Khawaja S, El Abed R, Alkhatib Z, Samaranayake LP. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Dis, 2021; 27(Suppl 3):655–64. CrossRef
Jia H, Li L, Li W, Hou T, Ma H, Yang Y, Wu A, Liu Y, Wen J, Yang H, Luo X, Xing Y, Zhang W, Wu Y, Ding L, Liu W, Lin L, Li Y, Chen M. Impact of healthcare-associated infections on length of stay: a study in 68 hospitals in China. Biomed Res Int, 2019;2019:2590563. CrossRef
Jin M, Liu L, Wang DN, Yang D, Liu WL, Yin J, Yang ZW, Wang HR, Qiu ZG, Shen ZQ, Shi DY, Li HB, Guo JH, Li JW. Chlorine disinfection promotes the exchange of antibiotic resistance genes across bacterial genera by natural transformation. ISME J, 2020; 14(7):1847–56. CrossRef
Jing JLJ, Pei Yi T, Bose RJC, McCarthy JR, Tharmalingam N, Madheswaran T. Hand sanitizers: a review on formulation aspects, adverse effects, and regulations. Int J Environ Res Public Health, 2020; 17(9):3326. CrossRef
Judd PA, Tomlin PJ, Whitby JL, Inglis TC, Robinson JS. Disinfection of ventilators by ultrasonic nebulization. Lancet (London, England), 1968; 2(7576):1019–20. CrossRef
Kahn G. Depigmentation caused by phenolic detergent germicides. Arch Dermatol, 1970; 102(2):177–87.
Kampf G, Kramer A, Suchomel M. Lack of sustained efficacy for alcohol-based surgical hand rubs containing ‘residual active ingredients’ according to EN 12791. J Hosp Infect, 2017; 95(2):163–8; doi: 10.1016/j.jhin.2016.11.001 CrossRef
Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev, 2004; 17(4):863–93. CrossRef
Kampf G, Löffler H, Gastmeier P. Hand hygiene for the prevention of nosocomial infections. Dtsch Arztebl Int, 2009; 106(40):649–55. CrossRef
Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect, 2020; 104(3):246–51. CrossRef
Kampf G. Acquired resistance to chlorhexidine—is it time to establish an ‘antiseptic stewardship’ initiative? J Hosp Infect, 2016; 94(3):213–27. CrossRef
Kariwa H, Fujii N, Takashima I. Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents. Dermatology, 2006; 212 (Suppl 1):119–23. CrossRef
Kim CK, Gentile DM, Sproul OJ. Mechanism of ozone inactivation of bacteriophage f2. Appl Environ Microbiol, 1980; 39(1):210–8. CrossRef
Kim M, Weigand MR, Oh S, Hatt JK, Krishnan R, Tezel U, Pavlostathis SG, Konstantinidis KT. Widely used benzalkonium chloride disinfectants can promote antibiotic resistance. Appl Environ Microbiol, 2018; 84(17):e01201–18. CrossRef
Kinyoun JJ. Formaldehyde as a disinfecting agent and its practical application. 1897. Public Health Rep, 2006; 121(Suppl 1):5–15; discussion 4.
Koch-Heier J, Hoffmann H, Schindler M, Lussi A, Planz O. Inactivation of SARS-CoV-2 through Treatment with the Mouth Rinsing Solutions ViruProX(®) and BacterX(®) Pro. Microorganisms, 2021; 9(3):521. CrossRef
Kommenda N. How is the coronavirus affecting global air traffic? London. The Guardian, 2020. Available via https://www.theguardian.com/world/ng-interactive (Accessed July 2021).
Krajewska J, Krajewski W, Zub K, Zato?ski T. COVID-19 in otolaryngologist practice: a review of current knowledge. Eur Arch Otorhinolaryngol, 2020; 277(7):1885–97.
Kratzel A, Todt D, V’kovski P, Steiner S, Gultom M, Thao TTN, Ebert N, Holwerda M, Steinmann J, Niemeyer D, Dijkman R, Kampf G, Drosten C, Steinmann E, Thiel V, Pfaender S. Inactivation of severe acute respiratory syndrome coronavirus 2 by WHO-recommended hand rub formulations and alcohols. Emerg Infect Dis, 2020; 26(7):1592–5. CrossRef
Kurakula M, Rao G. Pharmaceutical assessment of polyvinylpyrrolidone (PVP): As excipient from conventional to controlled delivery systems with a spotlight on COVID-19 inhibition. J Drug Deliv Sci Technol, 2020; 60:102046. CrossRef
La Rochelle P, Julien AS. How dramatic were the effects of handwashing on maternal mortality observed by Ignaz Semmelweis? J R Soc Med, 2013; 106(11):459–60. CrossRef
Landrigan PJ, Schechter CB, Lipton JM, Fahs MC, Schwartz J. Environmental pollutants and disease in American children: estimates of morbidity, mortality, and costs for lead poisoning, asthma, cancer, and developmental disabilities. Environ Health Persp. 2002;110(7):721–8. CrossRef
Lane HJ, Blum N, Fee E. Oliver Wendell Holmes (1809–1894) and Ignaz Philipp Semmelweis (1818-1865): preventing the transmission of puerperal fever. Am J Public Health, 2010; 100(6):1008–9. CrossRef
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, Soucy JR, Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect, 2020; 26(12):1622–9. CrossRef
Leclercq I, Batéjat C, Burguière AM, Manuguerra JC. Heat inactivation of the Middle East respiratory syndrome coronavirus. Influenza Other Respir Viruses, 2014; 8(5):585–6. CrossRef
Leslie RA, Zhou SS, Macinga DR. Inactivation of SARS-CoV-2 by commercially available alcohol-based hand sanitizers. Am J Infect Control, 2021; 49(3):401–2. CrossRef
L’Huillier AG, Tapparel C, Turin L, Boquete-Suter P, Thomas Y, Kaiser L. Survival of rhinoviruses on human fingers. Clin Microbiol Infect, 2015; 21(4):381–5. CrossRef
Li D, Sangion A, Li L. Evaluating consumer exposure to disinfecting chemicals against coronavirus disease 2019 (COVID-19) and associated health risks. Environ Int, 2020a; 145:106108. CrossRef
Li X, Wang C, Zhang J, Liu J, Liu B, Chen G. Preparation and application of magnetic biochar in water treatment: a critical review. Sci Total Environ, 2020b; 711:134847. CrossRef
Lin J, Zhou Q, Zhu W, Li Q, Xu L, Chen W, Wang J, Zhang X, Hu W, Li M. Formation of formaldehyde as an artifact peak in headspace GC analysis resulting from decomposition of sample diluent DMSO: A GC-MS investigation with deuterated DMSO. J Pharm Biomed Anal, 2020; 188:113361. CrossRef
Ling ML, Ching P, Widitaputra A, Stewart A, Sirijindadirat N, Thu LTA. APSIC guidelines for disinfection and sterilization of instruments in health care facilities. Antimicrobial Res Infection Cont, 2018; 7:25. CrossRef
Lingel NJ, Coffey B. Effects of disinfecting solutions recommended by the Centers for Disease Control on Goldmann tonometer biprisms. J Am Optom Assoc, 1992; 63(1):43–8.
Lloyd-Evans N, Springthorpe VS, Sattar SA. Chemical disinfection of human rotavirus-contaminated inanimate surfaces. J Hyg (Lond), 1986; 97(1):163–73. CrossRef
Lu Z, Wang H, Zhang A, Liu X, Zhou W, Yang C, Guddat L, Yang H, Schofield CJ, Rao Z. Structures of Mycobacterium tuberculosis penicillin-binding protein 3 in complex with five β-Lactam antibiotics reveal mechanism of inactivation. Mol Pharmacol, 2020; 97(4):287–94. CrossRef
Mackenzie D. Ultraviolet light fights new virus. Engineering (Beijing), 2020; 6(8):851–3. CrossRef
Magiorakos AP, Leens E, Drouvot V, May-Michelangeli L, Reichardt C, Gastmeier P, Wilson K, Tannahill M, McFarlane E, Simon A. Pathways to clean hands: highlights of successful hand hygiene implementation strategies in Europe. Euro Surveill, 2010; 15(18):19560. CrossRef
Martin WJ. Complex intracellular inclusions in the brain of a child with a stealth virus encephalopathy. Exp Mol Pathol, 2003; 74(3):197–209. CrossRef
Mathur P. Hand hygiene: back to the basics of infection control. Indian J Med Res, 2011; 134(5):611–20. CrossRef
Mayer S, Boos M, Beyer A, Fluit AC, Schmitz FJ. Distribution of the antiseptic resistance genes qacA, qacB, and qacC in 497 methicillin-resistant and -susceptible European isolates of Staphylococcus aureus. J Antimicrob Chemother, 2001; 47(6):896–7.
Mbithi JN, Springthorpe VS, Sattar SA. Chemical disinfection of hepatitis A virus on environmental surfaces. Appl Environ Microbiol, 1990; 56(11):3601–4. CrossRef
McCulloch EC, Costigan S. A comparison of the efficiency of phenol, liquor cresolis, formaldehyde, sodium hypochlorite, and sodium hydroxide against Eberthella typhi at various temperatures. J Infect Dis, 1936:281–4. CrossRef
McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev, 1999; 12(1):147–79. CrossRef
Flynn M. The man who discovered that unwashed hands could kill—and was ridiculed for it. The Washington Post, 2020. Available via https://www.washingtonpost.com/nation/2020/03/23/ignaz-semmelweis-handwashing-coronavirus/ (Accesseed 24 June 2021).
Medina-Ramón M, Zock JP, Kogevinas M, Sunyer J, Torralba Y, Borrell A, Burgos F, Antó JM. Asthma, chronic bronchitis, and exposure to irritant agents in occupational, domestic cleaning: a nested case-control study. Occup Environ Med, 2005; 62(9):598–606. CrossRef
Mimoz O, Lucet JC, Kerforne T, Pascal J, Souweine B, Goudet V, Mercat A, Bouadma L, Lasocki S, Alfandari S, Friggeri A, Wallet F, Allou N, Ruckly S, Balayn D, Lepape A, Timsit JF; CLEAN trial investigators. Skin antisepsis with chlorhexidine-alcohol versus povidone iodine-alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomized, controlled, two-by-two factorial trial. Lancet, 2015; 386(10008):2069–77. CrossRef
Miner NA, McDowell JW, Willcockson GW, Bruckner NI, Stark RL, Whitmore EJ. Antimicrobial and other properties of a new stabilized alkaline glutaraldehyde disinfectant/sterilizer. Am J Hosp Pharm, 1977; 34(4):376–82. CrossRef
Monegro AF, Muppidi V, Regunath H. Hospital acquired infections. [Updated 2020 Sep 3]. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL, 2021. Available via https://www.ncbi.nlm.nih.gov/books/NBK441857/ (Accessed 26 June 2021).
Montazeri N, Manuel C, Moorman E, Khatiwada JR, Williams LL, Jaykus LA. Virucidal activity of fogged chlorine dioxide- and hydrogen peroxide-based disinfectants against human norovirus and its surrogate, feline calicivirus, on hard-to-reach surfaces. Front Microbiol. 2017;8:1031. CrossRef
Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol, 2020; 7(1):83–101. CrossRef
Morton HE. The relationship of concentration and germicidal efficiency of ethyl alcohol. Ann NY Acad Sci, 1950; 53(1):191–6. CrossRef
Mosqueda-Melgar J, Elez-Martínez P, Raybaudi-Massilia RM, Martín-Belloso O. Effects of pulsed electric fields on pathogenic microorganisms of major concern in fluid foods: a review. Crit Rev Food Sci Nutr, 2008; 48(8):747–59. CrossRef
Mphaphlele M, Dharmadhikari AS, Jensen PA, Rudnick SN, van Reenen TH, Pagano MA, Leuschner W, Sears TA, Milonova SP, van der Walt M, Stoltz AC, Weyer K, Nardell EA. Institutional tuberculosis transmission. controlled trial of upper room ultraviolet air disinfection: a basis for new dosing guidelines. Am J Respir Crit Care Med, 2015; 192(4):477–84. CrossRef
Murray AK. The Novel Coronavirus COVID-19 Outbreak: global Implications for antimicrobial resistance. Front Microbiol, 2020; 11:1020. CrossRef
Nabi G, Wang Y, Hao Y, Khan S, Wu Y, Li D. Massive use of disinfectants against COVID-19 poses potential risks to urban wildlife. Environ Res, 2020; 188:109916. CrossRef
Nasir M, Chowdhury A, Zahan T. Self-medication during COVID-19 outbreak: a cross-sectional online survey in Dhaka city. Int J Basic Clin Pharmacol, 2020; 9(9):1325–30. CrossRef
Nasr AM, Mostafa MS, Arnaout HH, Elshimy AAA. The effect of exposure to sub-inhibitory concentrations of hypochlorite and quaternary ammonium compounds on antimicrobial susceptibility of Pseudomonas aeruginosa. Am J Infect Control, 2018; 46(7):e57–63. CrossRef
National Research Council (US) Safe Drinking Water Committee. Drinking-water and health, Vol. 2. National Academies Press (US), Washington, DC, 1980. Available via https://www.ncbi.nlm.nih.gov/books/NBK234592/ (Accessed 24 June 2021).
Nawrocki J, Raczyk-Stanis?awiak U, Swietlik J, Olejnik A, Sroka MJ. Corrosion in a distribution system: Steady water and its composition. Water Res, 2010; 44(6):1863–72.
Neely AN, Maley MP. The 1999 Lindberg award. 3% hydrogen peroxide for the gram-positive disinfection of fabrics. J Burn Care Rehabil, 1999; 20(6):471–7. CrossRef
Nnadozie CF, Lin J, Govinden R. Selective isolation of bacteria for metagenomic analysis: Impact of membrane characteristics on bacterial filterability. Biotechnol Prog, 2015; 31(4):853–66. CrossRef
Noorimotlagh Z, Mirzaee SA, Jaafarzadeh N, Maleki M, Kalvandi G, Karami C. A systematic review of emerging human coronavirus (SARS-CoV-2) outbreak: focus on disinfection methods, environmental survival, and control and prevention strategies. Environ Sci Pollut Res Int, 2021; 28(1):1–15. CrossRef
O’Brien RT, Newman J. Structural and compositional changes associated with chlorine inactivation of polioviruses. Appl Environ Microbiol, 1979; 38(6):1034–9. CrossRef
Ogilvie BH, Solis-Leal A, Lopez JB, Poole BD, Robison RA, Berges BK. Alcohol-free hand sanitizer and other quaternary ammonium disinfectants quickly and effectively inactivate SARS-CoV-2. J Hosp Infect, 2021; 108:142–5. CrossRef
Okeke IN, Klugman KP, Bhutta ZA, Duse AG, Jenkins P, O’Brien TF, Pablos-Mendez A, Laxminarayan R. Antimicrobial resistance in developing countries. Part II: strategies for containment. Lancet Infect Dis, 2005; 5(9):568–80. CrossRef
Otte JM, Blackwell N, Soos V, Rughöft S, Maisch M, Kappler A, Kleindienst S, Schmidt C. Sterilization impacts on marine sediment—are we able to inactivate microorganisms in environmental samples? FEMS Microbiol Ecol, 2018; 94(12):fiy189. CrossRef
Palumbo VD, Bruno A, Di Trapani B, Tomasello G. 2016 WHO global guidelines for the prevention of surgical site infection: a new step to improve patients’ safety before, during and after surgery. Life Saf Secur, 2017; 5(1):1–13.
Park DK, Bitton G, Melker R. Microbial inactivation by microwave radiation in the home environment. J Environ Health, 2006; 69(5):17–24; quiz 39-40.
Patterson AM. Meaning of “Antiseptic,” “Disinfectant,” and related words. Am J Public Health Nations Health, 1932; 22(5):465–72. CrossRef
Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci, 2020; 12(1):9. CrossRef
Pitt D, Aubin JM. Joseph Lister: father of modern surgery. Can J Surg, 2012; 55(5): E8–9. CrossRef
Pittet D, Allegranzi B, Boyce J, World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of E. The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect Control Hosp Epidemiol, 2009; 30(7):611–22. CrossRef
Popat SC, Yates MV, Deshusses MA. Kinetics of inactivation of indicator pathogens during thermophilic anaerobic digestion. Water Res, 2010; 44(20):5965–72. CrossRef
Poyatos JM, Almecija MC, García-Mesa JJ, Munio MM, Hontoria E, Torres JC, Osorio F. Advanced methods for the elimination of microorganisms in industrial treatments: potential applicability to wastewater reuse. Water Environ Res, 2011; 83(3):233–46. CrossRef
Pradhan D, Biswasroy P, Kumar Naik P, Ghosh G, Rath G. A review of current interventions for COVID-19 prevention. Arch Med Res, 2020; 51(5):363–74. CrossRef
Pratelli A. Action of disinfectants on canine coronavirus replication in vitro. Zoonoses Public Health, 2007; 54(9–10):383–6. CrossRef
Pratelli A. Canine coronavirus inactivation with physical and chemical agents. Vet J, 2008; 177(1):71–9. CrossRef
Protano C, Cammalleri V, Romano Spica V, Valeriani F, Vitali M. Hospital environment as a reservoir for cross-transmission: cleaning and disinfection procedures. Ann Ig, 2019; 31(5):436–48.
Quinn V JM, Dhabalia TJ, Roslycky LL, Wilson V JM, Hansen JC, Hulchiy O, Golubovskaya O, Buriachyk M, Vadim K, Zauralskyy R, Vyrva O, Stepanskyi D, Ivanovitch PS, Mironenko A, Shportko V, McElligott JE. COVID-19 at War: The Joint Forces Operation in Ukraine. Disaster Med Public Health Prep, 2021:1–8. CrossRef
Rabenau HF, Cinatl J, Morgenstern B, Bauer G, Preiser W, Doerr HW. Stability and inactivation of SARS coronavirus. Med Microbiol Immunol, 2005a; 194(1–2):1–6. CrossRef
Rabenau HF, Kampf G, Cinatl J, Doerr HW. Efficacy of various disinfectants against SARS coronavirus. J Hosp Infect, 2005b; 61(2):107–11. CrossRef
Rahman S, Montero MTV, Rowe K, Kirton R, Kunik F Jr. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: a review of current evidence. Expert Rev Clin Pharmacol, 2021; 14(5):601–21. CrossRef
Rahn O. Physical methods of sterilization of microorganisms. Bacteriol Rev, 1945; 9(1):1–47.
Rai NK, Ashok A, Akondi BR. Consequences of chemical impact of disinfectants: safe preventive measures against COVID-19. Crit Rev Toxicol, 2020; 50(6):513–20. CrossRef
Ramphul K, Mejias SG. Coronavirus disease: a review of a new threat to public health. Cureus, 2020; 12(3):e7276. CrossRef
Ratnesar-Shumate S, Williams G, Green B, Krause M, Holland B, Wood S, Bohannon J, Boydston J, Freeburger D, Hooper I, Beck K, Yeager J, Altamura LA, Biryukov J, Yolitz J, Schuit M, Wahl V, Hevey M, Dabisch P. Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. J Infect Dis, 2020; 222(2):214–22. CrossRef
Rattanakul S, Oguma K. Inactivation kinetics and efficiencies of UV-LEDs against Pseudomonas aeruginosa, Legionella pneumophila, and surrogate microorganisms. Water Res, 2018; 130:31–7. CrossRef
Ray C, Jain R. Low-cost emergency water purification technologies: integrated water security series. Butterworth-Heinemann, Oxford, UK, 2014. Available via https://www.researchgate.net/publication/286070705_Low_Cost_Emergency_Water_Purification_Technologies_Integrated_Water_Security_Series (Accessed July 2021).
Reichardt C, Königer D, Bunte-Schönberger K, van der Linden P, Mönch N, Schwab F, Behnke M, Gastmeier P. Three years of national hand hygiene campaign in Germany: what are the key conclusions for clinical practice? J Hosp Infect, 2013; 83(Suppl 1):S11–6. CrossRef
Ren SY, Wang WB, Hao YG, Zhang HR, Wang ZC, Chen YL, Gao RD. Stability and infectivity of coronaviruses in inanimate environments. World J Clin Cases, 2020; 8(8):1391–9. CrossRef
Ríos-Castillo AG, González-Rivas F, Rodríguez-Jerez JJ. Bactericidal efficacy of hydrogen peroxide-based disinfectants against Gram-positive and Gram-negative bacteria on stainless steel surfaces. J Food Sci, 2017; 82(10):2351–6. CrossRef
Rodrigo C, Fernando SD, Rajapakse S. Clinical evidence for repurposing chloroquine and hydroxychloroquine as antiviral agents: a systematic review. Clin Microbiol Infect, 2020; 26(8):979–87. CrossRef
Roy D, Wong PK, Engelbrecht RS, Chian ES. Mechanism of enteroviral inactivation by ozone. Appl Environ Microbiol. 1981;41(3):718-723. CrossRef
Rume T, Islam SMD. Environmental effects of COVID-19 pandemic and potential strategies of sustainability. Heliyon, 2020;6(9):e04965. CrossRef
Rutala WA, Barbee SL, Aguiar NC, Sobsey MD, Weber DJ. Antimicrobial activity of home disinfectants and natural products against potential human pathogens. Infect Control Hosp Epidemiol, 2000; 21(1):33–8. CrossRef
Rutala WA, Cole EC, Wannamaker NS, Weber DJ. Inactivation of Mycobacterium tuberculosis and Mycobacterium bovis by 14 hospital disinfectants. Am J Med, 1991; 91(3b):267s–71s. CrossRef
Rutala WA, Weber DJ, Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for disinfection and sterilization in healthcare facilities, 2008. Available via https://stacks.cdc.gov/view/cdc/47378 (Accessed 30 July 2021).
Rutala WA, Weber DJ. Disinfection and sterilization in health care facilities: an overview and current issues. Infect Dis Clin North Am, 2016; 30(3):609–37. CrossRef
Rutala WA, Weber DJ. Disinfection and sterilization: an overview. Am J Infect Control, 2013; 41(5 Suppl):S2–5. CrossRef
Rutala WA, Weber DJ. Disinfection of endoscopes: review of new chemical sterilants used for high-level disinfection. Infect Control Hosp Epidemiol, 1999; 20(1):69–76. CrossRef
Rutala WA, Weber DJ. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin Microbiol Rev, 1997; 10(4):597–610. CrossRef
Saadatpour F, Mohammadipanah F. Physicochemical susceptibility of SARS-CoV-2 to disinfection and physical approach of prophylaxis. Health Sci Rep, 2020; 3(4):e213. CrossRef
Sabino CP, Ball AR, Baptista MS, Dai T, Hamblin MR, Ribeiro MS, Santos AL, Sellera FP, Tegos GP, Wainwright M. Light-based technologies for management of COVID-19 pandemic crisis. J Photochem Photobiol B, 2020; 212:111999. CrossRef
Safapour N, Metcalf RH. Enhancement of solar water pasteurization with reflectors. Appl Environ Microbiol, 1999; 65(2):859–61. CrossRef
Saif LJ, Wang Q, Vlasova AN, Jung K, Xiao S. Coronaviruses. Dis Swine, 2019:488–523. CrossRef
Saknimit M, Inatsuki I, Sugiyama Y, Yagami K. Virucidal efficacy of physico-chemical treatments against coronaviruses and parvoviruses of laboratory animals. Jikken Dobutsu, 1988; 37(3):341–5. CrossRef
Sale AJ, Hamilton WA. Effects of high electric fields on micro-organisms. 3. Lysis of erythrocytes and protoplasts. Biochim Biophys Acta, 1968; 163(1):37–43. CrossRef
Sanderson DC, Carmichael LA, Fisk S. Thermoluminescence detection of irradiated fruits and vegetables: international interlaboratory trial. J AOAC Int, 2003; 86(5):971–5. CrossRef
Sattar SA, Springthorpe VS, Karim Y, Loro P. Chemical disinfection of non-porous inanimate surfaces experimentally contaminated with four human pathogenic viruses. Epidemiol Infect, 1989; 102(3):493–505. CrossRef
Sawalha AF. Storage and utilization patterns of cleaning products in the home: toxicity implications. Accid Anal Prev, 2007; 39(6):1186–91. CrossRef
Scarano A, Inchingolo F, Lorusso F. Environmental disinfection of a dental clinic during the COVID-19 pandemic: a narrative insight. Biomed Res Int, 2020; 2020:8896812. CrossRef
Schmid S, Geffers C, Wagenpfeil G, Simon A. Preventive bundles to reduce catheter-associated bloodstream infections in neonatal intensive care. GMS Hyg Infect Control, 2018; 13:Doc10.
Schrank CL, Minbiole KPC, Wuest WM. Are quaternary ammonium compounds, the workhorse disinfectants, effective against severe acute respiratory syndrome-coronavirus-2? ACS Infect Dis, 2020;6(7):1553–7. CrossRef
Sefah IA, Ogunleye OO, Essah DO, Opanga SA, Butt N, Wamaitha A, Guantai AN, Chikowe I, Khuluza F, Kibuule D, Nambahu L, Abubakar AR, Sani IH, Saleem Z, Kalungia AC, Thi Phuong TN, Haque M, Islam S, Kumar S, Sneddon J, Wamboga J, Wale J, Miljkovi? N, Kurdi A, Martin AP, Godman B. Rapid assessment of the potential paucity and price increases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on Africa and the implications. Front Pharmacol, 2021; 11:588106. CrossRef
Sehmi SK, Allan E, MacRobert AJ, Parkin I. The bactericidal activity of glutaraldehyde-impregnated polyurethane. Microbiol Open, 2016; 5(5):891–7. CrossRef
Sharafi SM, Ebrahimpour K, Nafez A. Environmental disinfection against COVID-19 in different areas of health care facilities: a review. Rev Environ Health. Available via 2020:/j/reveh.ahead-of-print/reveh-2020-0075/reveh-2020-0075.xml
Shetty R, Jayadev C, Chabra A, Maheshwari S, D’Souza S, Khamar P, Sethu S, Honavar SG. Sanitizer aerosol-driven ocular surface disease (SADOSD)-A COVID-19 repercussion? Indian J Ophthalmol, 2020; 68(6):981–3. CrossRef
Siddharta A, Pfaender S, Vielle NJ, Dijkman R, Friesland M, Becker B, Yang J, Engelmann M, Todt D, Windisch MP, Brill FH, Steinmann J, Steinmann J, Becker S, Alves MP, Pietschmann T, Eickmann M, Thiel V, Steinmann E. Virucidal activity of World Health Organization—recommended formulations against enveloped viruses, including zika, ebola, and emerging coronaviruses. J Infect Dis, 2017; 215(6):902–6. CrossRef
Sidwell RW, Dixon GJ, McNeil E. Quantitative studies on fabrics as disseminators of viruses. I. Persistence of vaccinia virus on cotton and wool fabrics. Applied Microb, 1966; 14(1):55–9. CrossRef
Silvany RE, Dougherty JM, McCulley JP, Wood TS, Bowman RW, Moore MB. The effect of currently available contact lens disinfection systems on Acanthamoeba castellanii and Acanthamoeba polyphaga. Ophthalmology, 1990; 97(3):286–90. CrossRef
Simons C, Walsh SE, Maillard JY, Russell AD. A note: ortho-phthalaldehyde: proposed mechanism of action of a new antimicrobial agent. Let Appl Microbiol, 2000; 31(4):299–302. CrossRef
Smith PW, Watkins K, Hewlett A. Infection control through the ages. Am J Infect Control, 2012; 40(1):35–42. CrossRef
Songur A, Ozen OA, Sarsilmaz M. The toxic effects of formaldehyde on the nervous system. Rev Environ Contam Toxicol, 2010; 203:105–18.
Srivastav AL, Patel N, Chaudhary VK. Disinfection by-products in drinking water: occurrence, toxicity, and abatement. Environ Pollut, 2020; 267:115474. CrossRef
Steger-Hartmann T, Länge R, Schweinfurth H, Tschampel M, Rehmann I. Investigations into the environmental fate and effects of iopromide (ultravist), a widely used iodinated X-ray contrast medium. Water Res, 2002; 36(1):266–74. CrossRef
Stratton GR, Bellona CL, Dai F, Holsen TM, Thagard SM. Plasma-based water treatment: Conception and application of a new general principle for reactor design. Chem Engin J, 2015; 273:543–50. CrossRef
Suslick KS, Didenko Y, Fang MM, Hyeon T, Kolbeck KJ, McNamara WB, Mdleleni MM, Wong M. Acoustic cavitation and its chemical consequences. Philos Transact R Soc Lond Ser A: Math Phys Engin Sci, 1999; 357(1751):335–53. CrossRef
Sweatt L. US Department of Labor Occupational Safety and Health Administration directive number: CPL 02-00-164 effective date: 04/14/2020. Available via https://www.osha.gov/ (Accessed July 2021).
Szeto W, Yam WC, Huang H, Leung DYC. The efficacy of vacuum-ultraviolet light disinfection of some common environmental pathogens. BMC Infect Dis, 2020; 20(1):127. CrossRef
Tandiono, Ohl SW, Ow DS, Klaseboer E, Wong VV, Dumke R, Ohl CD. Sonochemistry and sonoluminescence in microfluidics. Proc Natl Acad Sci USA, 2011; 108(15):5996–8. CrossRef
Todd EC, Michaels BS, Holah J, Smith D, Greig JD, Bartleson CA. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 10. Alcohol-based antiseptics for hand disinfection and a comparison of their effectiveness with soaps. J Food Prot, 2010; 73(11):2128–40. CrossRef
Tortorici MA, Walls AC, Lang Y, Wang C, Li Z, Koerhuis D, Boons GJ, Bosch BJ, Rey FA, de Groot RJ, Veesler D. Structural basis for human coronavirus attachment to sialic acid receptors. Nat Struct Mol Biol, 2019; 26(6):481–9. CrossRef
Tulchinsky TH, Varavikova EA. A history of public health. The new public health. 3rd edition, Academic Press, Elsevier, London, UK, 2014.
Tuuli MG, Liu J, Stout MJ, Martin S, Cahill AG, Odibo AO, Colditz GA, Macones GA. A Randomized trial comparing skin antiseptic agents at cesarean delivery. N Engl J Med, 2016; 374(7):647–55. CrossRef
Tyagi U, Barwal KC. Ignac Semmelweis-Father of Hand Hygiene. Indian J Surg, 2020:1–2.
Tyan K, Kang J, Jin K, Kyle AM. Evaluation of the antimicrobial efficacy and skin safety of a novel color additive in combination with chlorine disinfectants. Am J Infect Control, 2018; 46(11):1254–61. CrossRef
Tyler R, Ayliffe GA, Bradley C. Virucidal activity of disinfectants: studies with the poliovirus. J Hosp Infect, 1990; 15(4):339–45. CrossRef
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med, 2020; 382(16):1564–7. CrossRef
Vaskina IV, Roi IO, Pliatsuk LD, Vaskin RA, Yakhnenko OM. Study of the magnetic water treatment mechanism. J Ecol Engin, 2020; 21(2):251–60. CrossRef
Vesley D, Norlien KG, Nelson B, Ott B, Streifel AJ. Significant factors in the disinfection and sterilization of flexible endoscopes. Am J Infect Control, 1992; 20(6):291–300. CrossRef
V’kovski P, Kratzel A, Steiner S, Stalder H, Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat Rev Microbiol, 2021; 19(3):155–70. CrossRef
Wagh A, Sinha A. Prevention of healthcare-associated infections in the pediatric intensive care unit. Childs Nerv Syst, 2018; 34(10):1865–70. CrossRef
Wales AD, Davies RH. Co-selection of resistance to antibiotics, biocides, and heavy metals, and its relevance to foodborne pathogens. Antibiotics (Basel, Switzerland), 2015; 4(4):567–604. CrossRef
Walsh DJ, Livinghouse T, Goeres DM, Mettler M, Stewart PS. Antimicrobial activity of naturally occurring phenols and derivatives against biofilm and planktonic bacteria. Front Chem, 2019; 7:653. CrossRef
Walsh SE, Maillard JY, Simons C, Russell AD. Studies on the mechanisms of the antibacterial action of ortho-phthalaldehyde. J Appl Microbiol, 1999; 87(5):702–10. CrossRef
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 2020a; 323(11):1061–9. CrossRef
Wang J, Shen J, Ye D, Yan X, Zhang Y, Yang W, Li X, Wang J, Zhang L, Pan L. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ Pollut, 2020b; 262:114665. CrossRef
Weinmann T, Forster F, von Mutius E, Vogelberg C, Genuneit J, Windstetter D, Nowak D, Radon K, Gerlich J. Association between occupational exposure to disinfectants and asthma in young adults working in cleaning or health services: results from a cross-sectional analysis in Germany. J Occup Environ Med, 2019; 61(9):754–9. CrossRef
Wilson NM, Norton A, Young FP, Collins DW. Airborne transmission of severe acute respiratory syndrome coronavirus-2 to healthcare workers: a narrative review. Anesthesia, 2020; 75(8):1086–95. CrossRef
Wood A, Payne D. The action of three antiseptics/disinfectants against enveloped and non-enveloped viruses. J Hosp Infect, 1998; 38(4):283–95. CrossRef
Worboys M. Joseph Lister and the performance of antiseptic surgery. Notes Rec R Soc Lond, 2013; 67(3):199–209. CrossRef
World Health Organization. Cleaning and disinfection of environmental surfaces in the context of COVID-19, 2020. Available via https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19 (Accessed 23 June 2021).
World Health Organization. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. World Health Organization, Geneva, Switzerland, 2009. 1, Definition of terms. Pp 2 Available via https://www.ncbi.nlm.nih.gov/books/NBK144046/ (Accesseed 24 June 2021).
Worth LJ, Daley AJ, Spelman T, Bull AL, Brett JA, Richards MJ. Central and peripheral line-associated bloodstream infections in Australian neonatal and pediatric intensive care units: findings from a comprehensive Victorian surveillance network, 2008–2016. J Hosp Infect, 2018; 99(1):55–61. CrossRef
Xia T, Kleinheksel A, Lee EM, Qiao Z, Wigginton KR, Clack HL. Inactivation of airborne viruses using a packed bed non-thermal plasma reactor. J Phys D Appl Phys, 2019; 52(25):255201. CrossRef
Xiling G, Yin C, Ling W, Xiaosong W, Jingjing F, Fang L, Xiaoyan Z, Yiyue G, Ying C, Lunbiao C, Liubo Z, Hong S, Yan X. In vitro inactivation of SARS-CoV-2 by commonly used disinfection products and methods. Sci Rep, 2021; 11(1):2418. CrossRef
Xu S, Li Y. Beware of the second wave of COVID-19. Lancet (London, England), 2020a; 395(10233):1321–22; doi:10.1016/S0140-6736(20)30845-X
Xu Z. Can common coronavirus compete with novel coronavirus?. OSF Preprints, 2020b; doi:10.31219/osf.io/drtgp CrossRef
Yadollahpour A, Rashidi S, Ghotbeddin Z, Jalilifar M, Rezaee Z. Electromagnetic fields for the treatments of wastewater: a review of applications and future opportunities. J Pure Appl Microbiol, 2014; 8(5):3711–9.
Yeargin T, Buckley D, Fraser A, Jiang X. The survival and inactivation of enteric viruses on soft surfaces: a systematic review of the literature. Am J Infect Control, 2016; 44(11):1365–73. CrossRef
Yip L, Bixler D, Brooks DE, Clarke KR, Datta SD, Dudley S Jr, Komatsu KK, Lind JN, Mayette A, Melgar M, Pindyck T, Schmit KM, Seifert SA, Shirazi FM, Smolinske SC, Warrick BJ, Chang A. Serious adverse health events, including death, associated with ingesting alcohol-based hand sanitizers containing methanol—Arizona and New Mexico, May–June 2020. MMWR Morb Mortal Wkly Rep, 2020; 69(32):1070–3. CrossRef
Zacher B, Haller S, Willrich N, Walter J, Abu Sin M, Cassini A, Plachouras D, Suetens C, Behnke M, Gastmeier P, Wieler LH, Eckmanns T. Application of a new methodology and R package reveals a high burden of healthcare-associated infections (HAI) in Germany compared to the average in the European Union/European Economic Area, 2011 to 2012. Euro Surveill, 2019; 24(46):1900135. CrossRef
Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med, 2020; 46(4):586–90. CrossRef
Zhou Q, Fan L, Lai X, Tan L, Zhang X. Estimating extra length of stay and risk factors of mortality attributable to healthcare-associated infection at a Chinese university hospital: a multi-state model. BMC Infect Dis, 2019; 19(1):975. CrossRef
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med, 2020; 382(8):727–33. CrossRef
Zimmermann M, Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg, 2020; 48(5):521–6. CrossRef