Abstract
Background:
Patients often complain about the esthetic problems of gingival pigmentation. The aim of this study was to compare the effectiveness and recurrence of diode laser 810 nm and cryosurgery for gingival depigmentation.Methods:
A total of 12 patients with physiologic gingival pigmentation were selected. The inclusion criterion was the presence of gingival pigmentation of maxillary incisors and the exclusion criteria was the presence of systemic diseases or use of any drugs associated with gingival pigmentation. For further evaluation, photographs were taken before and after treatment within the same position and light. Color analysis was done using the Adobe Photoshop software. Patients were treated by diode laser 810 nm - 2 w and on the opposite side cryosurgery was performed. Treatment was done under topical anesthesia if required. The laser beam was activated using the brush technique and in contact mode. Application period differed according to the degree of melanin pigmentation and epithelial thickness of the treated area. Cryosurgery was performed by a cotton swab. The swab was gently touched and rolled on the area for 10 to 15 seconds until the disappearance of gingival pigmentation. All patients were examined 1, 3, and 6 months after treatment.Results:
Data were analyzed using the SAS software version 19. The degree of pigmentation was considered as follows: score1: mild pigmentation, score 2: average pigmentation, and score 3: intense pigmentation. The treatment of gingival pigmentation with laser and cryosurgery showed marked improvement of gingival pigmentation in both methods as well as no significant difference between the 2 methods after 1, 3, and 6 months of treatment.Conclusions:
Both methods are appropriate for the treatment of gingival depigmentation and no significant recurrence was observed during the 6 months follow - up.Keywords
1. Background
Physiologic pigmentation is produced due to excessive production of melanin, which is symmetrical and stable. Oral pigmentation is caused by a whole range of internal and external factors. Many forms of pigmentation result from 5 primary pigments. These include melanin, melanoid, oxyhemoglobin, reduced hemoglobin, and carotene. Bilirubin and iron can also be the reason for pigmentation (1). Oral mucosal pigmentation can also be caused by a wide range of diseases and systemic conditions. Various stimuli, such as trauma, hormonal changes, medication, and radiation may result in an increased production of mucosal melanin.
Pigmentation can occur in any area of the mouth, yet the gingival is the most common location, and is also common in all races. Pigmentation can be classified to 2 color ranges from black to light brown. The number of melanin in the skin and mucous membranes is the same, yet less frequent and active in the mucous (2, 3). Melanocytes is initiated with the first step of tyrosine hydroxylation of tyrosine to Dihydroxyphenylalanine (DOPA) (4)
The prevalence of gingival physiologic pigmentation in Iran is 47.43% and according to the degree of pigmentation it could be mild (dark pink to light brown), average (dark brown to black), and intense (various colors, usually in average degree) (5). Melanin pigmentation is not considered a pathological lesion yet occasionally the lesion may be removed for cosmetic reasons. Appearance of teeth and the enhancement of a person’s smile are actually the most requested cosmetic service today (6).
For achieving the desired effects, surgical and non - surgical procedures, such as cryosurgery, electrosurgical, laser, chemical, abrasion, milling, different lasers, such as carbon dioxide (CO2) laser, Nd:YAG laser, and diode are used (6, 7). The best medication techniques can be used based on clinical experience and the practitioner preference (7). Cryosurgical depigmentation was applied through the use of a gas expansion system and the method is simple and effective and does not require any complex tools (8, 9). Other benefits of the cryosurgical technique, include the lack of bleeding, pain, scar, and very low incidence of secondary infection (10). In this method, abnormal tissue is destroyed by freezing with intense cold. The cytoplasm of the cell is frozen and the nature of the protein will be changed, causing cell death (11). Materials commonly used in cryosurgery, include liquid nitrogen (- 196°C), nitrous oxide (- 80°C), solid carbon dioxide (- 780°C), chlorodifluoromethane (- 410°C), diethyl ether (- 240°C), and propane (- 420°C). Oral mucosa, due to moisture and softness, is an appropriate tissue for this method. Cryosurgery includes 3 methods: probe systems, liquid nitrogen spray, and cotton swab. The probe system follows the principles of Joule - Thompson expansion, which enable substances to undergo a drop in temperature when moved from a high pressure area to a low pressure area. For instance, when nitrous oxide is released from a high pressure inside the cryoprobe to lower pressure cryotip, the drop in temperature allows freezing of the tissues (12). The cotton swab technique involves dipping a cotton swab into liquid nitrogen for 1 to 2 seconds and applying it on the lesion with little pressure for 30 seconds (10).
In the recent years, laser has been used for the treatment of basal epithelial cells. Pigmented tissue can absorb light of specific wavelengths and can be removed without harming other cells. Laser has been widely used for removal of gingival pigmentation and many clinicians prefer laser treatment instead of a surgical procedure. The benefits of using laser involve less bleeding, reduced postoperative problems, and less bone loss in the treatment area (12). Various studies indicate that there is no significant difference in healing among various techniques of surgery (13-15). Laser pigmentation removal treatment is an effective method for removing pigmentation. Different types of laser include carbon dioxide (10.600 nm), diode (810 nm), Neodymium: Yttrium, aluminum garnet (1.064 nm), and Erbium: YAG. (2.940 nm). In the recent years, laser dentistry has superseded many traditional dentistry practices. The diode laser is a solid - state semiconductor laser that typically uses a combination of Gallium (Ga), Arsenide (Ar), and other elements, such as Aluminum (Al) and Indium (In), to change electrical energy into light energy. Diode laser can be delivered through a flexible quartz fiber optic hand piece. Diode wavelengths range from 810 to 819 nm. The level of energy is highly absorbed by the pigmented tissue and clinical result of this penetration is good hemostasis. The power level (typically 2 to 10 Watts) can be continuous or pulsed and the contact mode may be used in pigmented tissue to directly deliver the laser energy to the tissue (7). The non-contact method for focusing photons emitted by the tissue is used to create greater diameter, lower power, and lower frequencies, and can be used for coagulation of superficial lesions, for example in removing vascular tissues (16-18). The most common concern in post - treatment pigmentation is recurrence or failure to respond (19-21). The mechanism of recurrence is not known, however, according to the theory of migration, active melanocytes of pigmented area migrate to the adjacent area of treatment, which may be the cause for recurrence (22).
2. Methods
The present study was a clinical trial study. Samples included 12 patients with gingival melanin pigmentation in the anterior maxilla and the treatment area was maxillary incisors. Patients were informed that the treatment does not affect their systemic health. Samples that had at least a slight degree of physiological pigmentation in the maxillary anterior region were included in the study.
The exclusion criteria included presence of any kind of disease or systemic conditions that cause pigmentation as well as factors, such as smoking and medication that are involved in pigmentation. Informed consent form was signed by candidates of pigmentation removal.
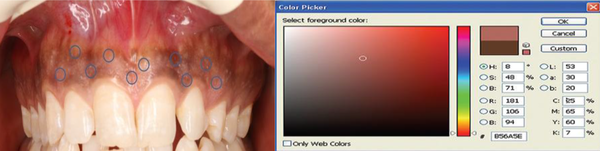
Four photos were taken from each patient, the first before the operation, and then after 1 month, 3 months, and 6 months after treatment. Photos were taken by the same camera and with the same zoom and the same programmed chair position to ensure standardization. The distance from the camera was also standardized at 3 feet by placing the camera over its tripod stand.
The degrees of gingival pigmentation before and after treatment were determined by the Photoshop CS4 software with colors of CMYK and RGB as follow: Mild (dark pink to pale brown), average (dark brown to black), and intense (various colors). An average color was considered for each area. Each patient was treated on one side by 810 nm diode laser with output power reaching 2 watts and the other side was treated by cryosurgery.
Cryosurgery Depigmentation Treatment
Laser technique: A diode laser device (CHEESE ™ type made by GIGGA laser CO, UK) with a wavelength of 810 nm was used. Laser therapy was started without local anesthesia and if needed, local anesthesia was considered. It should be noted that 10 patients expressed the need for anesthesia and local anesthesia was applied. The laser beam was irradiated in continuous and contact mode. Working time zone was considered based on the degree of melanin pigmentation and epithelial thickness of the area of treatment. The movement direction of the beam from mucogingival junction to gingival margin was free. To prevent gingival deformity, gingival margin and papilla remained intact.
Cryosurgery technique: Treatment was started without local anesthesia and, if needed, local anesthesia was considered. The patients did not insist on local anesthesia. The maxillary labial surface was isolated by cotton rolls, and suction and cryosurgery was performed by a cotton swab. For this type of therapy, the cotton swab was soaked in liquid nitrogen and was placed on the diseased area. The swab was gently rotated back and forth for 10 to 15 seconds until the disappearance of pigmented areas and the emergence of snowy white facade in contact with the tissue. The snowy white facade appeared after approximately 20 seconds. This process was repeated 4 to 5 times for each area. Patients were recommended to use Gelofen capsule (400 mg) for managing their pain. All patients were regularly followed up, at 1 month, 3 months, and 6 months.
3. Results
Data were analyzed by the SAS software version 19. The degree of pigmentation was considered as follow: score 1: mild pigmentation, score 2: average pigmentation, and score 3: intense pigmentation.
Comparison of Oral Pigmentation Removal by the Laser and Cryosurgery Method (P < 0.01)
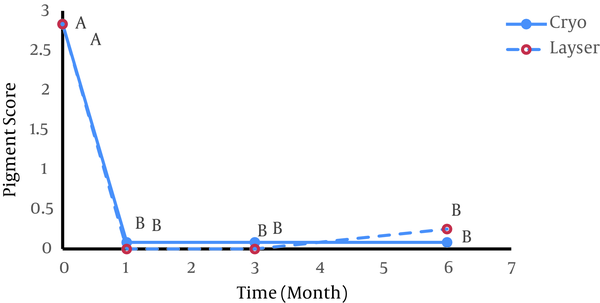
Figure 2 represents the pigmentation removal score by the laser and cryosurgery method. At the time of the intervention, pigmented patients had a score of 3. After a month of treatment and in the first follow - up, the laser depigmentation score decreased from 3 to 0 and the cryosurgery depigmentation score decreased from 3 to 0.08. This decline was significant compared to the day of the intervention for both methods and there was no statistical difference between the 2 methods. In the second follow - up (3 months after the initial intervention) the difference was significant compared to the day of the intervention and no change was observed compared to the first follow up. In the third follow up (6 months after the intervention), the impact of treatment was consistent and no significant change was observed compared to the first month and third month follow up. Therefore, the effect of depigmentation of the 2 methods in removing pigments was significant and identical with each other.
Prevalence of Treatment and Visiting Time in the Two Methods of Gingival Depigmentation
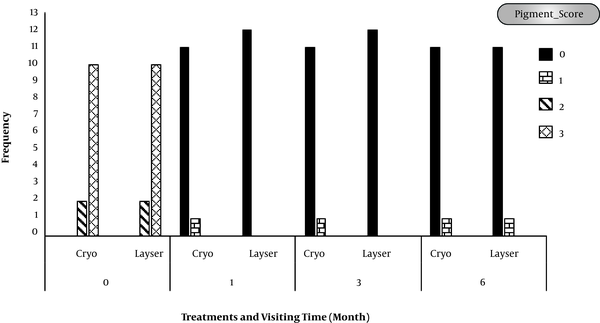
Figure 3 shows that 2 patients had a score of 2 and the rest had a score of 3 at the interval time zero. In the first follow - up, after the cryosurgery treatment, one patient had a score of 1 and 11 patients had a score of 0, while the score of all patients in the laser therapy treatments at the same interval time was 0. The same trend was observed in the 3 months following the treatment. Six months after treatment in both groups, one patient had the score of 1 and the other had a score of zero.
Cryosurgery Depigmentation Treatment

Laser Depigmentation Treatment

Pre - Operative View

Postoperative View After 1 Month

Postoperative View After 3 Month

Postoperative View After 6 Month

4. Discussion
Given the increasing prevalence of pigmentation and the increasing desire for a beautiful smile, the present study compared the effectiveness of 2 methods of depigmentation, including 810 - nm diode laser and the cryosurgery method. Furthermore, the diagnostic method with lower recurrence interval was evaluated. The results indicated that 810 - nm diode laser and cryosurgery methods are effective and safe means for removal of hyperpigmentation from the gingiva (Figure 2).
Simose et al., 2007, in a study conducted on 5 patients with melanin pigmentation found that using the laser Er: YAG (Pd: 38.5 mj, RR: 10 Hz) successfully destroyed the epithelial tissue and gingival pigmentation (23). Lee et al.’s study in 2011 suggested that Er:YAG laser could effectively remove the pigmentation from gingiva (24). Similarly, Simsekkaya et al.’s study in 2012 confirmed the efficacy of 808 nm diode laser and Er:YAG (2940 nm) laser for depigmentation of gingiva (25). Amin et al., 2013, in their study determined the effectiveness of swab and probe cryosurgery methods in gingival pigmentation removal (26). Kumar et al., 2013, in their study showed that cryosurgery is an effective method for gingival depigmentation (27) The result of Farahmand et al.’s study in 2014 revealed that Er:YAG laser and cryosurgery were the most efficient methods in gingival depigmentation (28). Rahmati et al., 2014, in their study confirmed the effectiveness of cryosurgery in pigmentation removal. The efficacy of cryosurgery in gingival depigmentation of 10 patients was reported (29). In another study by Basha et al. in 2015 the effect of Nd: YAG laser in removing gingival pigmentation was emphasized (30). Patil et al.’s study in 2015 announced that cryosurgery was an effective pigmentation removal method (31).
According to the findings of the present study, no significant difference was found between the 2 pigmentation removal methods. Farahmand et al., 2014, in their study conducted in Iran, investigating Er:YAG laser (Pd: 120 mj, RR:120 Hz) and cryosurgery methods, found no significant difference between the 2 methods and both were announced effective methods (28).
In the present study, recurrence after 6 months in the laser method occurred in one case and in the cryosurgery method recurrence was found in one case after the first month of treatment, which was not statistically significant. Simose et al., 2007, in their study showed that the use of Er:YaG laser (38 mJ, 5 Hz, 10 J/cm2) in pigmentation removal after 3 months does not lead to gingival deformation or abrasion; however, in one case, a slight recurrence of gingival pigmentation was observed (23). Simsekkaya et al., 2012, examined the effect of diode laser and Er:YAG laser in gingival depigmentation at the interval time of 14 months for diode laser and 11 months for Er:YAG laser. No evidence of recurrence was reported (25). Farahmand et al., 2014, examined the application of Er:YAG laser (PD:120 mj , RR:120 Hz) and cryosurgery at specific interval time of 1, 2, and 4 weeks and 3, 6, and 12 months after treatment. No evidence of recurrence after 12 months of treatment was observed (28). Similarly, Basha et al.’s study in 2015 did not show recurrence after 6 months application of ND: YAG laser (30). Kumar et al., 2015, examined cryosurgical treatment of gingival melanin pigmentation with tetrafluoroethane. The result of this study confirmed the efficacy of cryosurgery method after 90 days, 180 days, and 2 months of treatment (27).
4.1. Conclusion
In conclusion, the results of present study showed that 810 nm diode laser and cryosurgery are safe and effective treatment methods for gingival depigmentation, and during the 6 months follow - up no recurrence was observed.
References
-
1.
Ozbayrak S, Dumlu A, Ercalik-Yalcinkaya S. Treatment of melanin-pigmented gingiva and oral mucosa by CO2 laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(1):14-5. [PubMed ID: 10884629].
-
2.
Gorsky M, Buchner A, Fundoianu-Dayan D, Aviv I. Physiologic pigmentation of the gingiva in Israeli Jews of different ethnic origin. Oral Surg Oral Med Oral Pathol. 1984;58(4):506-9. [PubMed ID: 6593682].
-
3.
Amir E, Gorsky M, Buchner A, Sarnat H, Gat H. Physiologic pigmentation of the oral mucosa in Israeli children. Oral Surg Oral Med Oral Pathol. 1991;71(3):396-8. [PubMed ID: 2011372].
-
4.
Dummett CO, Barens G. Oromucosal pigmentation: an updated literary review. J Periodontol. 1971;42(11):726-36. [PubMed ID: 4944004]. https://doi.org/10.1902/jop.1971.42.11.726.
-
5.
Rabiei M, Nasrin R. Frequency of oral mucosal pigmentation among patients referred to the faculty of dentistry, Guilan University of Medical Sciences. J Indian Dent Assoc. 2005;17:95-100.
-
6.
Newman M, Takei H, Klokkevold P, Carranza F. Clinical features of gingivitis. In: Fiorellini JP, Kim DM, editors. Carranza's clinical periodontology. Philadelphia: WB saunder; 2000. p. 366-7.
-
7.
Prabhuji ML, Madhupreetha SS, Archana V. Treatment of gingival hyperpigmentation for aesthetic purposes using the diode laser. Int Mag Laser Dent. 2011;3(2):30-2.
-
8.
Tal H, Landsburg J, Kozlovsky A. Cryosurgical depigmentation of the gingiva. J Clin Periodontal. 1987;57:48-50. https://doi.org/10.1111/j.1600-051X.1987.tb01525.x.
-
9.
Yeh CJ. Cryosurgical treatment of melanin-pigmented gingiva. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(6):660-3. [PubMed ID: 9868720].
-
10.
Yu CH, Chen HM, Chang CC, Hung HY, Hsiao CK, Chiang CP. Cotton-swab cryotherapy for oral leukoplakia. Head Neck. 2009;31(8):983-8. [PubMed ID: 19283844]. https://doi.org/10.1002/hed.21055.
-
11.
Talebi M, Farmanbar N, Abolfazli S, Sarraf Shirazi A. Management of physiological hyperpigmentation of oral mucosa by cryosurgical treatment: a case report. J Dent Res Dent Clin Dent Prospects. 2012;6(4):148-51. [PubMed ID: 23277862]. https://doi.org/10.5681/joddd.2012.030.
-
12.
Sunitha J. Cryotherapy–A review. J Clin Diagn Res. 2010;4(2):2325-9.
-
13.
Berk G, Atici K, Berk N. Treatment of gingival pigmentation with Er, Cr: YSGG laser. J Oral Laser Applications. 2005;5(4):249-53.
-
14.
Rizoiu IM, Eversole LR, Kimmel AI. Effects of an erbium, chromium: yttrium, scandium, gallium, garnet laser on mucocutanous soft tissues. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(4):386-95. https://doi.org/10.1016/s1079-2104(96)80302-7.
-
15.
Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd:YAG laser: report of 4 cases. J Periodontol. 2000;71(2):315-21. [PubMed ID: 10711623]. https://doi.org/10.1902/jop.2000.71.2.315.
-
16.
Romanos G, Nentwig GH. Diode laser (980 nm) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. J Clin Laser Med Surg. 1999;17(5):193-7. [PubMed ID: 11199822]. https://doi.org/10.1089/clm.1999.17.193.
-
17.
Coluzzi D. Fundamental of lasers in dentistry: Basic science, tissue interaction, and instrumentation. J Laser Dent. 2008;16:4-10.
-
18.
Desiate A, Cantore S, Tullo D, Profeta G, Grassi FR, Ballini A. 980 nm diode lasers in oral and facial practice: current state of the science and art. Int J Med Sci. 2009;6(6):358-64. [PubMed ID: 19960121].
-
19.
Holtzclaw D, Toscano NJ, Tal H. Spontaneous pigmentation of non-pigmented palatal tissue after periodontal surgery. J Periodontol. 2010;81(1):172-6. [PubMed ID: 20059430]. https://doi.org/10.1902/jop.2009.090289.
-
20.
Dummett CO, Bolden TE. Postsurgical clinical repigmentation of the cingivae. Oral Surg Oral Med Oral Pathol. 1963;16(3):353-65. https://doi.org/10.1016/0030-4220(63)90299-8.
-
21.
Bergamaschi O, Kon S, Doine AI, Ruben MP. Melanin repigmentation after gingivectomy: a 5-year clinical and transmission electron microscopic study in humans. Int J Periodontics Restorative Dent. 1993;13(1):85-92. [PubMed ID: 8330948].
-
22.
Kaur H, Jain S, Sharma RL. Duration of reappearance of gingival melanin pigmentation after surgical removal - A clinical study. J Indian Soc Periodontol. 2010;14(2):101-5. [PubMed ID: 21691546]. https://doi.org/10.4103/0972-124X.70828.
-
23.
Simose A, Helfield S, Ruben S. Using Er:YAG laser in gingival depigmentation. J Laser Med Surg. 2007;17(5):103-7.
-
24.
Lee KM, Lee DY, Shin SI, Kwon YH, Chung JH, Herr Y. A comparison of different gingival depigmentation techniques: ablation by erbium:yttrium-aluminum-garnet laser and abrasion by rotary instruments. J Periodontal Implant Sci. 2011;41(4):201-7. [PubMed ID: 21954425]. https://doi.org/10.5051/jpis.2011.41.4.201.
-
25.
Simsek Kaya G, Yavuz YG, Sumbullu M, Dayi, A. A comparison of diode laser and Er:YAG lasers in the treatment of gingival melanin pigmentation. J Oral Maxillofac Surg. 2012;113(3):293-9.
-
26.
Sedeh SA, Badihi S, Esfahaniyan V. Comparison of recurrent rate of gingival pigmentation after treatment by liquid nitrogen and cryoprob in 18 months follows-up. Dent Res J (Isfahan). 2014;11(5):592-8. [PubMed ID: 25426152].
-
27.
Kumar S, Bhat GS, Bhat KM. Comparative Evaluation of Gingival Depigmentation using Tetrafluoroethane Cryosurgery and Gingival Abrasion Technique: Two Years Follow Up. J Clin Diagn Res. 2013;7(2):389-94. [PubMed ID: 23543863]. https://doi.org/10.7860/JCDR/2013/4454.2779.
-
28.
Farahmand A, Moghareh Abed A, Mansouri Y. Clinical application of Er:YAG laser and cryosurgery in gingival depigmentation. World J Dent. 2014;5(2):102-8. https://doi.org/10.5005/jp-journals-10015-1268.
-
29.
Rahmati S, Darijani M, Nourelahi M. Comparison of surgical blade and cryosurgery with liquid nitrogen techniques in treatment of physiologic gingival pigmentation: short term results. J Dent (Shiraz). 2014;15(4):161-6. [PubMed ID: 25469354].
-
30.
Basha MI, Hegde RV, Sumanth S, Sayyed S, Tiwari A, Muglikar S. Comparison of Nd:YAG Laser and Surgical Stripping for Treatment of Gingival Hyperpigmentation: A Clinical Trial. Photomed Laser Surg. 2015;33(8):424-36. [PubMed ID: 26226173]. https://doi.org/10.1089/pho.2014.3855.
-
31.
Patil KP, Joshi V, Waghmode V, Kanakdande V. Gingival depigmentation: A split mouth comparative study between scalpel and cryosurgery. Contemp Clin Dent. 2015;6(Suppl 1):S97-S101. [PubMed ID: 25821386]. https://doi.org/10.4103/0976-237X.152964.
