Published online Jul 25, 2022. doi: 10.5501/wjv.v11.i4.186
Peer-review started: December 28, 2021
First decision: February 8, 2022
Revised: February 19, 2022
Accepted: June 26, 2022
Article in press: June 26, 2022
Published online: July 25, 2022
The coronavirus disease 2019 (COVID-19) pandemic has brought fundamental changes to our problems and priorities, especially those related to the healthcare sector. India was one of the countries severely affected by the harsh consequences of the COVID-19 pandemic.
To understand the challenges faced by the healthcare system during a pandemic.
The literature search for this review was conducted using PubMed, EMBASE, Scopus, Web of Science, and Google Scholar. We also used Reference Citation Analysis (RCA) to search and improve the results. We focused on the published scientific articles concerned with two major vital areas: (1) The Indian healthcare system; and (2) COVID-19 pandemic effects on the Indian healthcare system.
The Indian healthcare system was suffering even before the pandemic. The pandemic has further stretched the healthcare services in India. The main obstacle in the healthcare system was to combat the rising number of communicable as well as noncommunicable diseases. Besides the pandemic measures, there was a diversion of focus of the already established healthcare services away from the chronic conditions and vaccinations. The disruption of the vaccination services may have more severe short and long-term consequences than the pandemic’s adverse effects.
Severely restricted resources limited the interaction of the Indian healthcare system with the COVID-19 pandemic. Re-establishment of primary healthcare services, maternal and child health services, noncommunicable diseases programs, National Tuberculosis Elimination Program, etc. are important to prevent serious long-term consequences of this pandemic.
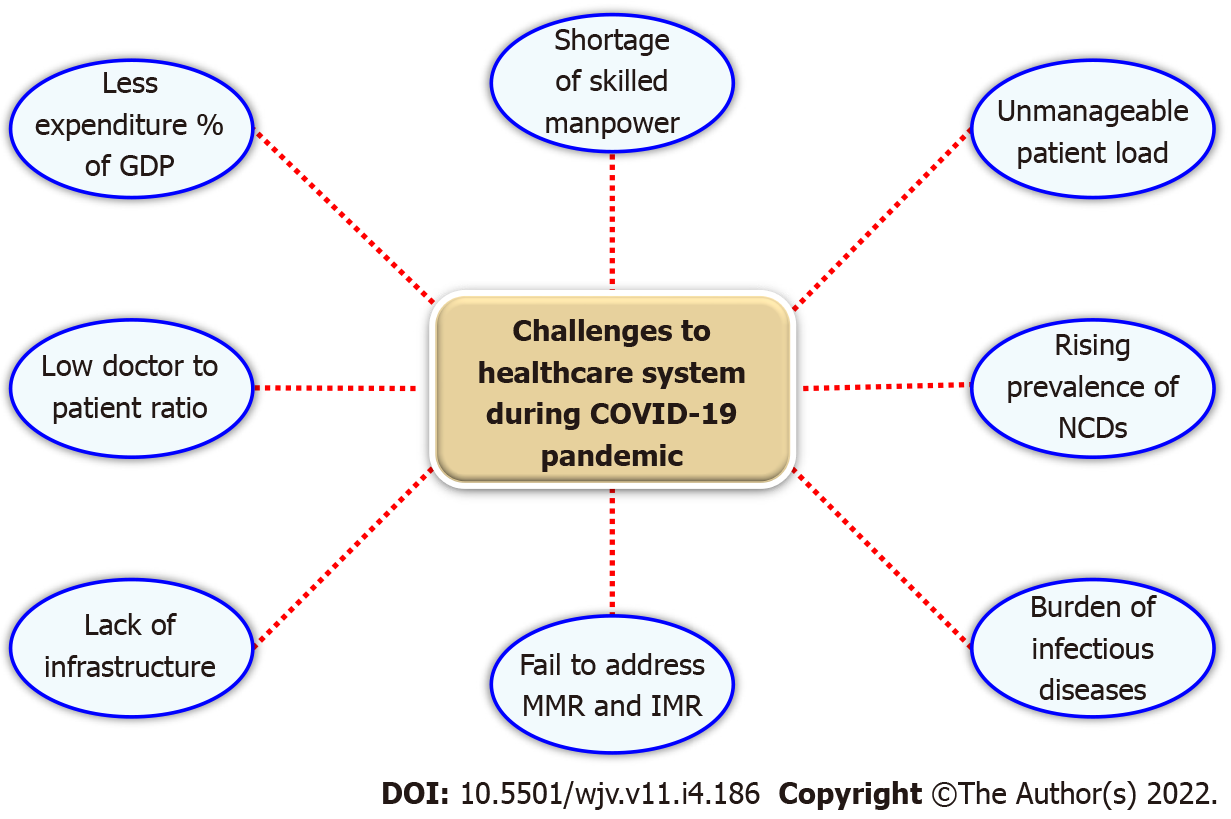
Core Tip: The interaction of the Indian healthcare system with the coronavirus disease 2019 pandemic was limited by restricted resources. Lack of infrastructure, low percentage of gross domestic product expenditure on health, and deficiency of skilled manpower play a critical role in the healthcare system to manage infectious diseases, noncommunicable diseases and maternal and child health services.
- Citation: Nimavat N, Hasan MM, Charmode S, Mandala G, Parmar GR, Bhangu R, Khan I, Singh S, Agrawal A, Shah A, Sachdeva V. COVID-19 pandemic effects on the distribution of healthcare services in India: A systematic review. World J Virol 2022; 11(4): 186-197
- URL: https://www.wjgnet.com/2220-3249/full/v11/i4/186.htm
- DOI: https://dx.doi.org/10.5501/wjv.v11.i4.186
The coronavirus disease 2019 (COVID-19) pandemic, since its start at the end of 2019 in Wuhan, China, has changed the face of our planet. The pandemic affects almost every detail in our daily life, from dietary consumption to education and obviously to healthcare utilization, the primary sector affected by the pandemic[1]. The evolution of the pandemic has created extra challenges to the different healthcare sectors across the world, either those dealing with patients directly or those responsible for logistic supplies to the healthcare facilities[2]. The healthcare sectors in the developing countries were especially affected, suffering from the limited public health infrastructure and medical supplies even before the pandemic[3-5]. In India alone, COVID-19 infected > 10 million citizens, and > 45000 had died by the end of September 2021, and the number is increasing every day[6].
The strain and fast changes created by the pandemic have put the Indian healthcare services in an impending collapse due to the destructive waves of the pandemic[7]. Before the pandemic, the Indian healthcare services were struggling to meet the primary healthcare (PHC) demands of the public affected by a variety of communicable diseases and noncommunicable diseases (NCDs)[8]. Besides COVID-19, other medical conditions with a public health concern like acquired immune deficiency syndrome, tuberculosis (TB), and malaria outbreaks continue to pose a strain on the healthcare services and continuous monitoring is required to detect and manage these conditions at an early stage[9]. Also, NCDs are now the leading cause of death in India, accounting for about 60% of all deaths across the country[10]. The emergence of the COVID-19 pandemic at the end of 2019 has forced many secondary and tertiary healthcare centers designated to receive millions of daily patients to be dedicated only for COVID-19 presumptive cases. These effects have created a huge gap in the provision of healthcare services in managing chronic cases[11].
A recent multicenter survey conducted by Raman et al[12] has demonstrated that the COVID-19 pandemic has a significant negative effect on healthcare providers with an exaggerated feeling of inadequacy: [odds ratio (OR) = 3.015], inappropriateness: (OR = 2.225), and discontinuity of care: (OR = 6.756) together with associated depression and social loneliness. India, which was already suffering from an unacceptably high maternal mortality rate of 41.4 per 1000 live births in 2013, developed a significant interruption in the maternal and child health services during the pandemic[13,14]. This negative effect has extended to almost all established maternal/child healthcare services, including antenatal care and immunization services. For instance, some regions have demonstrated a decrease in institutional deliveries by about 2.26%. Antenatal health services were badly affected, with a decline estimated to be 22.9%[15]. Prenatal care visits in China have dropped, healthcare infrastructure has been stretched, and possibly damaging practices have been introduced with insufficient proof[16]. Garg et al[15] has demonstrated that PHC services were severely disrupted. They have also surveyed the readiness of PHCs across India and demonstrated a severe shortage in infection control measures, i.e., infection prevention and control. Twenty-nine of 51 participating PHCs had inadequate ventilation in the workplace, while NK95 masks were available only in half of the centers[15,17]. During the pandemic in Australia, healthcare utilization fell by roughly a third, with significant variance, and with more considerable decreases among persons with less severe disease[18].
This narrative review discusses the different factors associated with the unavailability of resources in healthcare facilities during the COVID-19 pandemic in India. We also highlight how the deficiency of PHC services may contribute to the sustainability of the COVID-19 pandemic in India.
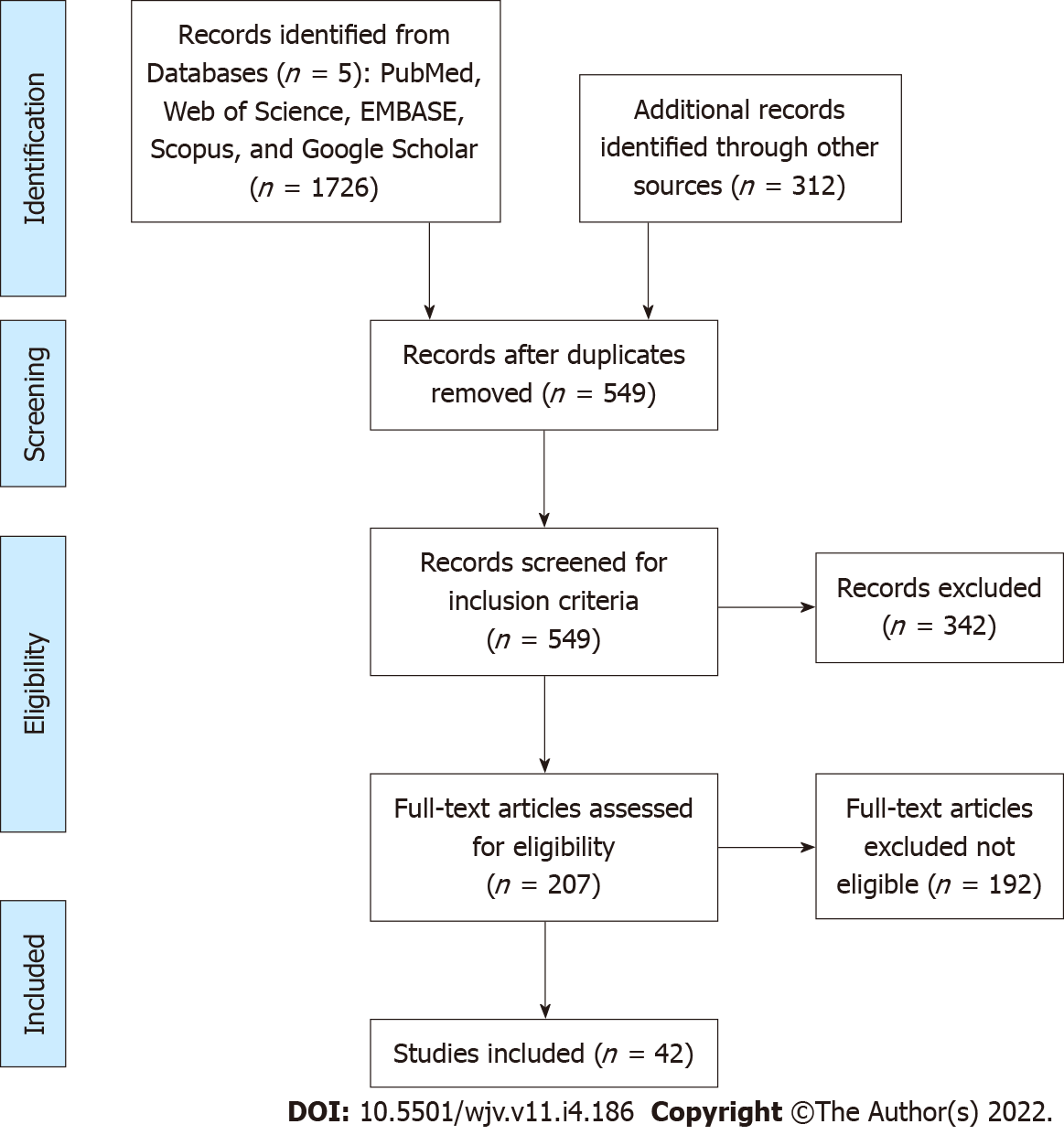
The review was carried out through the following methodological steps (Figure 1). Different search terms related to the Indian healthcare system formulated two health strategies. The first health strategy was used to target the characteristics of the Indian healthcare system before the pandemic together with its associated challenges, which include: (((("India"[Mesh]) AND "Delivery of Health Care"[Mesh]) OR "Community Health Planning"[Mesh]) OR "Health Services"[Mesh]) AND "Epidemiology"[Mesh]. The second health strategy was centered on the Indian healthcare system and health situation during the pandemic using the following terms ((("India"[Mesh]) OR ("COVID-19"[Mesh] OR "SARS-CoV-2"[Mesh])) AND "Delivery of Health Care"[Mesh]) OR "Delivery of Health Care, Integrated"[Mesh]. PubMed, EMBASE, Scopus, Reference Citation Analysis (RCA), Web of Science, and Google Scholar were used to search the related literature. We also employed Reference Citation Analysis, an open multiple disciplines citation analysis database powered by artificial intelligence technologies. All of the papers were stacked and screened initially by title to categorize the papers into eligible or noneligible. Eligible literature was further screened using full text to exclude any irrelevant information. References of the relevant studies were also screened to track any missed helpful literature. The above methodology was consistent with the previously reported methodology of narrative reviews studies.
India has a large and diverse healthcare system that suits the cultural diversity of the community[5]. The healthcare system in India was initially built to ensure that all citizens have access to essential healthcare services regardless of their socioeconomic status[19]. However, the ambitious healthcare system plans were not associated with considerable funds from the governmental agencies. In 2015, India spent only 1.2% of its gross domestic product (GDP) on health, considered among the lowest in the world[20]. The inadequacy of government healthcare services has resulted in the simultaneous evolution of the private health sector[21]. Subsequently, India has one of the highest proportions of household out-of-pocket expenditures on health globally, estimated at 71.1% in 2008-2009[22]. In addition, India has the lowest doctor-patient ratios as it has one doctor for 1000 and a specialist for every 1445 people[23]. The low healthcare expenditure in India had a severe negative impact on health status even before the COVID-19 pandemic. The pandemic further stretched the fragile nonimmune Indian healthcare system, leading to a collapse in providing healthcare services in order to contain COVID-19.
Among its 1.3 billion citizens, NCDs are responsible for 5.78 million (60%) of all deaths in India each year. The significant NCD-related deaths are usually attributed to cardiovascular disease, cancer and diabetes[24]. The rising NCD trend is a common phenomenon seen in developing countries where rapid urbanization leads to an overall economic improvement and has considerable adverse effects on public health[25]. The Indian health system has adopted multiple changes aiming to bring down NCD-related mortality by < 25% by 2025[26]. Although some progress has been achieved in decreasing tobacco and alcohol consumption, an increasing trend was found for overweight and obesity among Indian adults aged 15-49 years[24]. Reddy and Kar[26] have demonstrated that the Indian Government’s efforts were insufficient to achieve its ambitious targets by 2025, even before the pandemic.
Since the start of the epidemiological transition in 1970, there have been significant changes in the pattern of different diseases across every state in India[27]. Omran’s theory[28,29] describes the epidemiological transition as a shift in the causes of morbidity and mortality, primarily from infectious diseases to NCDs. However, the situation was different in India, where the burden of NCDs has been added to the burden of infectious disease, resulting in a double burden on the undeveloped Indian healthcare system[27,30]. In India, the epidemiological transition has led to the development of a new theory based on the concept of the double burden of both infectious diseases and NCDs[31]. The burden of communicable diseases has declined from 47.7% to only 22.1% between 1970 to the mid-1990s[31].
Even after 40 years from the start of the epidemiological transition in 2011, infectious diseases still pose a challenge to the Indian health system and account for about 30% of the disease burden[32]. It was estimated that an Indian citizen had a 15 times greater burden of infectious diseases than United Kingdom citizens in 2004 and that about 30% of the disease burden in India is attributable to infections[32]. The lack of strong staple public healthcare infrastructure has contributed largely to stagnation of the infectious disease burden in addition to the burden of NCDs[30,32]. For instance, in 2009, India recorded about 2 million new cases of TB, which is considered one of the highest incidences globally[32]. After 10 years in 2019, India reported about 2.9 million new cases of TB, contributing to about 27% of all TB cases worldwide[33]. However, India started its TB control program early, in 1960, but failed to significantly reduce the incidence of new TB cases compared to other countries with similar epidemiological transitions[34,35]. Concerns have been raised about the spread of TB and NCDs, specifically, diabetes mellitus, which are associated with a more fulminant course of TB[36,37].
Besides TB, multiple endemic infections affect Indian cities and states, such as cutaneous anthrax, dengue fever, malaria, cholera and viral hepatitis (A and B)[38-43]. Some of these infections are substantially preventable by vaccines[44]. Unfortunately, India contributes to about 10% of 20 million unimmunized and partially immunized populations[45]. Additionally, India is considered to have one of the largest rates of endemic hepatitis B, with the second largest burden of chronic hepatitis B, with > 50 million cases[46]. Despite being integrated into the Indian National Immunization Program in 2011, about 23.2% of children aged 5–8 years were vaccinated against hepatitis B virus[47]. Different causes have been proposed behind the low vaccination coverage of hepatitis in India; for instance, major causes are related to the poor management of the available health resources such as poor record-keeping, improper management of vaccine stocks and lack of inventory control, lack of staff training, and use of multidose vials. Strikingly, healthcare workers have been reported to be reluctant to open a vial of the vaccine when there are a few children to be vaccinated for fear of wastage[48]. It is well noted that even before the COVID-19 pandemic, India’s healthcare system was strained between the pre-existing communicable disease challenges and the evolving NCD pattern created by the epidemiological transition. All of the above challenges are further aggravated by the limited Government funds allocated to developing the healthcare system (Figure 2).
The number of people infected with COVID-19 has exceeded 9 million since the report of the first cases in the state of Kerala on January 30, 2020[1,6]. Following this, the country has witnessed a drastic increase in the total number of reported cases. The recovery rate across India was 80.83% as of September 22, 2020, with a case fatality rate of 2.82% as of June 1, 2020[49]. The development of the pandemic has primarily affected the rapidly developing Indian economy with shrinkage of the GDP by about 23.9% in April-June 2020[50]. Today, Indian citizens continue to be frightened into compliance and are afraid to restart their lives normally. Although many states of India have flattened their COVID-19 infection curve, authorities across the nation are now in fear from the onset of other subsequent waves of the COVID-19 pandemic secondary to a decreased commitment of health directives of taking precautionary measures, i.e., social distancing and wearing face masks. Government authorities have advised citizens to take precautionary measures like social distancing and wearing masks during public gatherings. Furthermore, a few states, such as Maharashtra, Rajasthan and Gujarat, have introduced new restrictions such as travel restrictions and night curfew to battle the subsequent waves of the COVID-19 pandemic[50].
In India, besides the chronic shortage of healthcare workers, there were significant deficiencies in different domains of healthcare services and their logistic determinants[51]. For instance, healthcare facilities have severe deficiencies in infection control measures, i.e., advance infection prevention and control facilities to contain infected patients and prevent the spread of COVID-19. In 2010, the Indian Government adopted national guidelines on airborne infection control in healthcare facilities with a special focus on preventing TB transmission[52]. Five years later, a baseline survey of healthcare facilities has demonstrated poor adherence to infection control measures aimed to control airborne infection[53]. Multiple studies have demonstrated several loopholes in the infection control policy, including insufficient training of staff, unavailability of protective masks, poor compliance to personal protective practices by health workers, i.e., proper use and disposal of personal protective equipment (PPE) and other control measures, inadequate disinfection, and sterilization of equipment, lack of health workers surveillance, lack of counseling of cough etiquette and sputum disposal at registration of hospitals[54-56].
In 2020, Indian health authorities recently updated the comprehensive national guidelines for infection control[51]. However, infection control measures across different PHC centers in Indian districts were grossly deficient, especially related to airborne infection[15]. The shortage was limited to the infection control measures, but it further extended to the PPE intended to protect the workforce from infection during the COVID-19 pandemic. It is reported that there is a persistent dearth of PPE in two private hospitals in Mumbai[57]. Reports from different areas across India have reported that doctors treat patients suspected of severe acute respiratory syndrome coronavirus 2 infection without masks or with less-protective surgical masks instead of recommended NK95 masks for healthcare providers[58]. Unfortunately, the shortage of PPE and high demands have forced healthcare workers to reuse or extend the use of PPE, which increases their risk of COVID-19[59]. The above behavior, despite being expected, highlights a lack of proper knowledge and training regarding infection control measures, usage of PPE, and their proper disposal. In fact, it is one of the rights of healthcare workers to be adequately trained before exposure to COVID-19 patients[60]. The lack of essential training of healthcare workers has been reported in several South Asian countries, including India[61]. Multiple studies have highlighted suboptimal knowledge and practice regarding infection control measures across Indian health workers[62,63]. Raj et al[54] have reported that only less than half of the healthcare workers of Kerala, India, were trained on proper infection control practices.
The growing distribution of the pandemic across different countries has delayed or even stopped the basic childhood vaccination programs as a response to the lockdown or the stretching of the healthcare resources as a response to the COVID-19 pandemic[64]. The World Health Organization (WHO) has reported that > 80 million children did not receive routine vaccination globally[65]. This may have serious long-term consequences even more than COVID-19 itself. For instance, the evolution of the Ebola outbreak in Africa resulted in halting multiple essential healthcare services, which increased mortality related to several other infections, including TB, human immunodeficiency virus, and measles which have exceeded the mortality rate from Ebola[66].
In India, the evolution of the pandemic has initially enforced complete stoppage of the whole childhood vaccination programs secondary to the major lockdown. It was estimated that about 27 million children missed diphtheria tetanus pertussis, resulting in a 40% increase in mortality in the next year. It has also been estimated that there is an expected 49000 child deaths and 2300 maternal deaths within a month if the PHC services continue to be disrupted[67,68]. As a response, the Indian Government has approved the continuation of the vaccination services and consider it an essential health service[69]. The resumption of the immunization activities was based on the WHO guidelines to minimize both morbidity and mortality from other diseases[70,71].
Maternal healthcare services have also been severely affected by the development of the pandemic. Globally, healthcare services have restricted pregnant women’s access to healthcare facilities for fear of virus transmission and the unknown adverse effects on the newborn, considering the Zika virus in the background[72,73]. The Health and Family Welfare Ministry has declared pregnant women as high risk during the COVID-19 pandemic and provides guidelines to provide essential maternal healthcare services to pregnant women, including the suspected and confirmed cases of COVID-19[74]. Goyal et al[75] have demonstrated a 45.1% decline in deliveries during the pandemic at their center. They have also noticed a surge in the number of high-risk pregnancies to about 7.2%. Additionally, more than one-third of women had no or inadequate prenatal visits, with more than half of them mentioning the lockdown as a cause of inadequacy of antenatal care.
Since reporting the first case of COVID-19, patients with chronic disease have had significant difficulties accessing their routine healthcare services worldwide[76]. The presence of chronic conditions like chronic kidney disease, cardiovascular disease, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, and malignancy in a patient with COVID-19 has been tied to poorer outcome with about 10-fold higher risk than those without associated comorbidity[77,78]. WHO has reported that half of 163 countries have attempted partial or complete disruption of healthcare services for hypertension, diabetes mellitus, and related complications during the pandemic. Additionally, one-third of the countries have reported disruption of healthcare services designated for cardiovascular emergencies[79].
Low- and middle-income countries have sustained considerable difficulty in assuring access to healthcare services to patients with chronic conditions compared with western countries[80]. Pati et al[81] conducted a community-based study in Odisha, India, and found that 43% of the patients with comorbid conditions have reported difficulty in accessing healthcare services. They have also reported that the most challenging problem was the physician consultation, accounting for 43% of cases. Another telephone-based survey targeting more than 1000 chronic patients reported that > 80% of the participants found it challenging to access healthcare services, and 17% of the participants found it difficult to obtain their medications. The same study also reported that > 50% of the participants reported a loss of income, and 38% had completely lost their jobs[82]. These clear negative impacts have forced health authorities to search for more cost-effective approaches to continue healthcare services to those patients with chronic medical conditions.
Telemedicine is defined by the WHO as the delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment and prevention of disease and injuries, research, and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities[83]. Before the COVID-19 pandemic, India had a few worthy examples of telemedicine models, including mammography services at Sri Ganga Ram Hospital, Delhi, and oncology at Regional Cancer Center, Trivandrum[84,85]. During the COVID-19 pandemic, the contribution of telemedicine in healthcare management has been highlighted. Kumar et al[86] reported that 71.43% of the orthopedic patients were managed without needing any physical visits to the outpatient clinics. Additionally, they have reported that 92% of the patients were satisfied with the telemedicine intervention.
The catastrophic health expenditure of < 2% of GDP in India must be increased at least to meet the expenditures of the surrounding developing Asian countries[87]. The COVID-19 pandemic has indicated that dependence on the private healthcare sector, assuming that an increase in the overall income of the individuals can cover their health expenditures, cannot be a good approach to healthcare management[88]. India also needs to establish a national stock level of PPE and other essential medical supplies like ventilators together with an efficient network to monitor and deliver upon need[89]. Learning from other Asian neighbors, both Taiwan and Singapore have established a similar network of PPE management which proved to be critical and efficient in the PPE management during the pandemic[90,91].
Establishing national manufacturing units is also essential to maintain an adequate supply to the Indian hospitals and other healthcare facilities even at times of global catastrophes. The enhancement of local manufacturing on a mass scale should be essentially accompanied by maintaining the ban of PPE exportation[89,92]. Together with providing adequate equipment to fight the pandemic, there is an impending need to enhance and maintain the training of healthcare workers regarding critical topics like infection control practices[93]. Diwan et al[94] have reported that attending training sessions have significantly impacted and improved hand hygiene among healthcare workers in rural India. In adjacent countries/territory like Singapore, Japan and Hong Kong, a high level of readiness of healthcare workers has played a critical role in early controlling the pandemic[95].
Besides empowering the healthcare system, it is also essential to engage the healthcare professionals in decision-making to avoid collateral, sometimes fatal, damage of halting essential services like vaccination and maternal healthcare services even for a short period. Establishing and empowering telemedicine is another crucial lesson that should be considered in the future. Integration of telemedicine even after the pandemic should be encouraged and continue as it has proved to be effective in the diagnosis, management of chronic disease, and guiding the treatment for different medical conditions in a cost-effective way[96,97].
RCA was used in this manuscript to improve the results and highlights[98].
During the COVID-19 pandemic, India’s healthcare system is overstretched in terms of resources, with all essential healthcare services, including maternal and child healthcare services, jeopardized. India needs to increase the investment and proportion of GDP in developing and improving its universal healthcare system to accommodate future pandemics/disasters or outbreaks. Intersectorial coordination and partnership with private entities, at a fast pace, are needed to meet the demands of the healthcare delivery system and provide universal standard healthcare to every citizen of India.
India was one of the countries worst hit by the devastating effects of the coronavirus disease 2019 (COVID-19) pandemic. The healthcare system was unable to manage the situation.
The underperformed healthcare system during the pandemic exposed the crisis.
To identify the challenges faced by the Indian healthcare system during the pandemic.
The review was conducted using a literature search from the database of PubMed, Web of Science, EMBASE, Scopus, etc. The main focus was on the Indian healthcare system and the impact of a pandemic.
The Indian healthcare system was already under pressure before the pandemic. The overburden of patients and essential health services were not handled efficiently. Many healthcare facilities were lacking the basic standards of patient care. The vaccination and chronic disease services were hampered due to the shifting of focus to COVID-19.
Universal Health Coverage should be provided to each person. Increase in percentage expenditure of gross domestic product for the health sector, escalate infrastructure development, and increment of skilled manpower required.
To meet the incremental demand in health care services during and after the pandemic, India needs to invest more in this sector with a goal of Universal Health Coverage.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Virology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Munteanu C, Romania; Papadopoulos K, Thailand; Wang TJ, China; Wang TJ, China A-Editor: Wang MK, China S-Editor: Gao CC L-Editor: Kerr C P-Editor: Gao CC
| 1. | Kumar SU, Kumar DT, Christopher BP, Doss CGP. The Rise and Impact of COVID-19 in India. Front Med (Lausanne). 2020;7:250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 2. | Barach P, Fisher SD, Adams MJ, Burstein GR, Brophy PD, Kuo DZ, Lipshultz SE. Disruption of healthcare: Will the COVID pandemic worsen non-COVID outcomes and disease outbreaks? Prog Pediatr Cardiol. 2020;59:101254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 91] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 3. | Blanchet K, Alwan A, Antoine C, Cros MJ, Feroz F, Amsalu Guracha T, Haaland O, Hailu A, Hangoma P, Jamison D, Memirie ST, Miljeteig I, Jan Naeem A, Nam SL, Norheim OF, Verguet S, Watkins D, Johansson KA. Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the COVID-19 pandemic. BMJ Glob Health. 2020;5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Gilbert M, Pullano G, Pinotti F, Valdano E, Poletto C, Boëlle PY, D'Ortenzio E, Yazdanpanah Y, Eholie SP, Altmann M, Gutierrez B, Kraemer MUG, Colizza V. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871-877. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 754] [Cited by in F6Publishing: 612] [Article Influence: 153.0] [Reference Citation Analysis (0)] |
| 5. | Zodpey SP, Negandhi HN. Training in clinical research in India: potential and challenges. Indian J Community Med. 2009;34:173-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard. [cited 17 Jan 2022]. In: World Health Organization [Internet]. Available from: https://covid19.who.int/. [Cited in This Article: ] |
| 7. | Williams OD. COVID-19 and Private Health: Market and Governance Failure. Development (Rome). 2020;63:181-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Dikid T, Jain SK, Sharma A, Kumar A, Narain JP. Emerging & re-emerging infections in India: an overview. Indian J Med Res. 2013;138:19-31. [PubMed] [Cited in This Article: ] |
| 9. | Narain JP. Public Health Challenges in India: Seizing the Opportunities. Indian J Community Med. 2016;41:85-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Narain JP, Kumar R. Textbook of chronic noncommunicable diseases: the health challenge of 21st century. [cited 17 Jan 2022]. In: Jaypee Digital [Internet]. Available from: https://www.jaypeedigital.com/book/9789352500437. [Cited in This Article: ] |
| 11. | Basu S. Non-communicable disease management in vulnerable patients during Covid-19. Indian J Med Ethics. 2020;V:103-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 12. | Raman R, Rajalakshmi R, Surya J, Ramakrishnan R, Sivaprasad S, Conroy D, Thethi JP, Mohan V, Netuveli G. Impact on health and provision of healthcare services during the COVID-19 Lockdown in India: a multicentre cross-sectional study. BMJ Open. 2021;11:e043590. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 13. | Singh AK, Jain PK, Singh NP, Kumar S, Bajpai PK, Singh S, Jha M. Impact of COVID-19 pandemic on maternal and child health services in Uttar Pradesh, India. J Family Med Prim Care. 2021;10:509-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | World Health Organization. World Health Statistics. [cited 14 Oct 2021]. In: World Health Organization [Internet]. Available from: https://www.who.int/data/gho/publications/world-health-statistics. [Cited in This Article: ] |
| 15. | Garg S, Basu S, Rustagi R, Borle A. Primary Health Care Facility Preparedness for Outpatient Service Provision During the COVID-19 Pandemic in India: Cross-Sectional Study. JMIR Public Health Surveill. 2020;6:e19927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 16. | Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 2021;18:10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 175] [Cited by in F6Publishing: 302] [Article Influence: 100.7] [Reference Citation Analysis (0)] |
| 17. | Poojary SA, Bagadia JD. Reviewing literature for research: Doing it the right way. Indian J Sex Transm Dis AIDS. 2014;35:85-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott I, Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11:e045343. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 663] [Cited by in F6Publishing: 541] [Article Influence: 180.3] [Reference Citation Analysis (1)] |
| 19. | Chokshi M, Patil B, Khanna R, Neogi SB, Sharma J, Paul VK, Zodpey S. Health systems in India. J Perinatol. 2016;36:S9-S12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 141] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 20. | Golechha M. Healthcare agenda for the Indian government. Indian J Med Res. 2015;141:151-153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Peters DH, Rao KS, Fryatt R. Lumping and splitting: the health policy agenda in India. Health Policy Plan. 2003;18:249-260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011;377:505-515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 575] [Cited by in F6Publishing: 446] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 23. | Sageena G, Sharma M, Kapur A. Evolution of Smart Healthcare: Telemedicine During COVID-19 Pandemic. J Inst Eng Ser B. 2021;102:1319-1324. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Nethan S, Sinha D, Mehrotra R. Non Communicable Disease Risk Factors and their Trends in India. Asian Pac J Cancer Prev. 2017;18:2005-2010. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 38] [Reference Citation Analysis (0)] |
| 25. | Chakma JK, Gupta S. Lifestyle and Non-Communicable Diseases: A double edged sword for future India. Ind J Comm Heal. 2014;26:325-332. [DOI] [Cited in This Article: ] |
| 26. | Reddy MM, Kar SS. Unconditional probability of dying and age-specific mortality rate because of major non-communicable diseases in India: Time trends from 2001 to 2013. J Postgrad Med. 2019;65:11-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Yadav S, Arokiasamy P. Understanding epidemiological transition in India. Glob Health Action. 2014;7:23248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 28. | Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. 1971. Milbank Q. 2005;83:731-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 450] [Cited by in F6Publishing: 404] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 29. | Omran AR. The epidemiologic transition theory. A preliminary update. J Trop Pediatr. 1983;29:305-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 93] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Banerjee K, Dwivedi LK. The burden of infectious and cardiovascular diseases in India from 2004 to 2014. Epidemiol Health. 2016;38:e2016057. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Dyson T. India’s population - the future. In: Dyson T, Cassen R, Visaria L. Twenty-First Century India: Population, Economy, Human Development, and the Environment. RePEc, 2004: 74-107. [Cited in This Article: ] |
| 32. | John TJ, Dandona L, Sharma VP, Kakkar M. Continuing challenge of infectious diseases in India. Lancet. 2011;377:252-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 33. | Wares DF. Report on the review of Programmatic management of drug-resistant tuberculosis (PMDT) component of the Revised. Natl TB Control Program. 2017;. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Mahadev B, Kumar P. History of tuberculosis control in India. J Indian Med Assoc. 2003;101:142-143. [PubMed] [Cited in This Article: ] |
| 35. | Pai M, Bhaumik S, Bhuyan SS. India's plan to eliminate tuberculosis by 2025: converting rhetoric into reality. BMJ Glob Health. 2016;2:e000326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Restrepo BI. Diabetes and Tuberculosis. Microbiol Spectr. 2016;4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 37. | Martinez N, Kornfeld H. Tuberculosis and diabetes: from bench to bedside and back. Int J Tuberc Lung Dis. 2019;23:669-677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | Bhavsar A, Tam CC, Garg S, Jammy GR, Taurel AF, Chong SN, Nealon J. Estimated dengue force of infection and burden of primary infections among Indian children. BMC Public Health. 2019;19:1116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Meeting of the Strategic Advisory Group of Experts on immunization, October 2009 - conclusions and recommendations. Wkly Epidemiol Rec. 2009;84:517-532. [PubMed] [Cited in This Article: ] |
| 40. | Nayak P, Sodha SV, Laserson KF, Padhi AK, Swain BK, Hossain SS, Shrivastava A, Khasnobis P, Venkatesh SR, Patnaik B, Dash KC. A cutaneous Anthrax outbreak in Koraput District of Odisha-India 2015. BMC Public Health. 2019;19:470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 41. | Sarkar S, Singh P, Lingala MAL, Verma P, Dhiman RC. Malaria risk map for India based on climate, ecology and geographical modelling. Geospat Health. 2019;14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Agrawal A, Singh S, Kolhapure S, Hoet B, Arankalle V, Mitra M. Increasing Burden of Hepatitis A in Adolescents and Adults and the Need for Long-Term Protection: A Review from the Indian Subcontinent. Infect Dis Ther. 2019;8:483-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 43. | Mourya DT, Yadav PD, Ullas PT, Bhardwaj SD, Sahay RR, Chadha MS, Shete AM, Jadhav S, Gupta N, Gangakhedkar RR, Khasnobis P, Singh SK. Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian J Med Res. 2019;149:447-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 44. | Orenstein WA, Ahmed R. Simply put: Vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114:4031-4033. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 165] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 45. | World Health Organization. Progress and Challenges with Achieving Universal Immunization Coverage. [cited 14 Oct 2021]. In: World Health Organization [Internet]. Available from: https://www.who.int/publications/m/item/progress-and-challenges-with-achievinguniversal-immunization-coverage. [Cited in This Article: ] |
| 46. | Komatsu H. Hepatitis B virus: where do we stand and what is the next step for eradication? World J Gastroenterol. 2014;20:8998-9016. [PubMed] [Cited in This Article: ] |
| 47. | Murhekar MV, Santhosh Kumar M, Kamaraj P, Khan SA, Allam RR, Barde P, Dwibedi B, Kanungo S, Mohan U, Mohanty SS, Roy S, Sagar V, Savargaonkar D, Tandale BV, Topno RK, Girish Kumar CP, Sabarinathan R, Bitragunta S, Grover GS, Lakshmi PVM, Mishra CM, Sadhukhan P, Sahoo PK, Singh SK, Yadav CP, Kumar R, Dutta S, Toteja GS, Gupta N, Mehendale SM; ICMR – Serosurvey group. Hepatitis-B virus infection in India: Findings from a nationally representative serosurvey, 2017-18. Int J Infect Dis. 2020;100:455-460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Lahariya C, Subramanya BP, Sosler S. An assessment of hepatitis B vaccine introduction in India: Lessons for roll out and scale up of new vaccines in immunization programs. Indian J Public Health. 2013;57:8-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 49. | Z Ansari AA, Desai HD, Sharma K, Jadeja DM, Patel R, Patel Y, Desai HM. Prevalence and cross states comparison of case fatality rate and recovery rate of COVID 19/SARS-COV-2 in India. J Family Med Prim Care. 2021;10:475-480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Jabaris S SL, V A. The current situation of COVID-19 in India. Brain Behav Immun Health. 2021;11:100200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 51. | Behera D, Praveen D, Behera MR. Protecting Indian health workforce during the COVID-19 pandemic. J Family Med Prim Care. 2020;9:4541-4546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 52. | Central TB Division. Guidelines_on_Airborne_Infection_Control: Ministry of Health and Family Welfare. [cited 14 Oct 2021]. In: Central TB Division [Internet]. Available from: https://tbcindia.gov.in/showfile.php?lid=2858. [Cited in This Article: ] |
| 53. | Parmar MM, Sachdeva KS, Rade K, Ghedia M, Bansal A, Nagaraja SB, Willis MD, Misquitta DP, Nair SA, Moonan PK, Dewan PK. Airborne infection control in India: Baseline assessment of health facilities. Indian J Tuberc. 2015;62:211-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Raj A, Ramakrishnan D, Thomas CRMT, Mavila AD, Rajiv M, Suseela RPB. Assessment of Health Facilities for Airborne Infection Control Practices and Adherence to National Airborne Infection Control Guidelines: A Study from Kerala, Southern India. Indian J Community Med. 2019;44:S23-S26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 55. | Sachdeva KS, Deshmukh RD, Seguy NS, Nair SA, Rewari BB, Ramchandran R, Parmar M, Vohra V, Singh S, Ghedia M, Agarwal R, Shah AN, Balasubramanian D, Bamrotiya M, Sikhamani R, Gupta RS, Khaparde SD. Tuberculosis infection control measures at health care facilities offering HIV and tuberculosis services in India: A baseline assessment. Indian J Tuberc. 2018;65:280-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 56. | Akshaya KM, Shewade HD, Aslesh OP, Nagaraja SB, Nirgude AS, Singarajipura A, Jacob AG. "Who has to do it at the end of the day?" Airborne infection control at drug resistant tuberculosis (DR-TB) centres of Karnataka, India: a mixed-methods study. Antimicrob Resist Infect Control. 2017;6:111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 57. | Rada AG. Covid-19: Almost 100 ICU staff from Malaga hospital test positive after Christmas lunch. BMJ. 2021;375:n3085. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Bhanot D, Singh T, Verma SK, Sharad S. Stigma and Discrimination During COVID-19 Pandemic. Front Public Health. 2020;8:577018. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 203] [Cited by in F6Publishing: 148] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 59. | Chughtai AA, Seale H, Islam MS, Owais M, Macintyre CR. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud. 2020;105:103567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 60. | International Council of Nurses. More than 600 nurses die from COVID-19 worldwide | ICN - International Council of Nurses. [cited 14 Oct 2021]. In: International Council of Nurses [Internet]. Available from: https://www.icn.ch/news/more-600-nurses-die-covid-19-worldwide. [Cited in This Article: ] |
| 61. | Gupta SK, Siddharth V, Belagere MR, Stewardson AJ, Kant S, Singh S, Singh N. National survey of infection control programmes in South Asian association for Regional Cooperation countries in the era of patient safety. Indian J Med Microbiol. 2018;36:577-581. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 62. | Lobo D, Sams L, Fernandez S. Correlation between health professionals knowledge, attitude and practice about infection control measures. J Med Allied Sci. 2019;9:26. [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Vinodhini K, Bhoomadevi A. Study On Infection Control Practices Among Healthcare Workers In A Speciality Hospital, Chennai. Pollut Res. 2016;35:549-555. [Cited in This Article: ] |
| 64. | McNally VV, Bernstein HH. The Effect of the COVID-19 Pandemic on Childhood Immunizations: Ways to Strengthen Routine Vaccination. Pediatr Ann. 2020;49:e516-e522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 65. | The United Nations Children's Fund. At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF. [cited 14 Oct 2021]. In: The United Nations Children's Fund [Internet]. Available from: https://www.unicef.org/press-releases/least-80-million-children-under-one-risk-diseases-such-diphtheria-measles-and-polio. [Cited in This Article: ] |
| 66. | Takahashi S, Metcalf CJ, Ferrari MJ, Moss WJ, Truelove SA, Tatem AJ, Grenfell BT, Lessler J. Reduced vaccination and the risk of measles and other childhood infections post-Ebola. Science. 2015;347:1240-1242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 139] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 67. | Shet A, Dhaliwal B, Banerjee P, DeLuca A, Carr K, Britto C, Seth R, Parekh B, Basavaraj GV, Shastri D, Gupta P. Childhood immunisations in India during the COVID-19 pandemic. BMJ Paediatr Open. 2021;5:e001061. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 68. | Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, Sawadogo-Lewis T, Walker N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e901-e908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 859] [Cited by in F6Publishing: 736] [Article Influence: 184.0] [Reference Citation Analysis (0)] |
| 69. | Indira Gandhi Government General Hospital And Post Graduation Institute. Immunization Services during and post COVID-19 Outbreak. [cited 14 Oct 2021]. In: Indira Gandhi Government General Hospital And Post Graduation Institute [Internet]. Available from: https://ghp.py.gov.in/immunization-services-during-and-post-covid-19-outbreak. [Cited in This Article: ] |
| 70. | World Health Organization. Maintaining essential health services: operational guidance for the COVID-19 context, interim guidance, 1 June 2020. [cited 14 Oct 2021]. In: World Health Organization [Internet]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2. [Cited in This Article: ] |
| 71. | Bharadwaj J, Sharma SK, Darbari A, Patil P. Immunization and vaccination of children during current COVID-19 pandemic: Impact and recommendation guidelines for India. J Family Med Prim Care. 2020;9:5411-5412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 72. | Montagnoli C, Zanconato G, Ruggeri S, Cinelli G, Tozzi AE. Restructuring maternal services during the covid-19 pandemic: Early results of a scoping review for non-infected women. Midwifery. 2021;94:102916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 73. | Reale SC, Fields KG, Lumbreras-Marquez MI, King CH, Burns SL, Huybrechts KF, Bateman BT. Association Between Number of In-Person Health Care Visits and SARS-CoV-2 Infection in Obstetrical Patients. JAMA. 2020;324:1210-1212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 74. | Chawla D, Chirla D, Dalwai S, Deorari AK, Ganatra A, Gandhi A, Kabra NS, Kumar P, Mittal P, Parekh BJ, Sankar MJ, Singhal T, Sivanandan S, Tank P; Federation of Obstetric and Gynaecological Societies of India (FOGSI), National Neonatology Forum of India (NNF) and Indian Academy of Pediatrics (IAP). Perinatal-Neonatal Management of COVID-19 Infection - Guidelines of the Federation of Obstetric and Gynaecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics (IAP). Indian Pediatr. 2020;57:536-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 75. | Goyal M, Singh P, Singh K, Shekhar S, Agrawal N, Misra S. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: Experience from a tertiary center. Int J Gynaecol Obstet. 2021;152:231-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 118] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 76. | Kendzerska T, Zhu DT, Gershon AS, Edwards JD, Peixoto C, Robillard R, Kendall CE. The Effects of the Health System Response to the COVID-19 Pandemic on Chronic Disease Management: A Narrative Review. Risk Manag Healthc Policy. 2021;14:575-584. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 105] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 77. | Sinclair AJ, Abdelhafiz AH. Age, frailty and diabetes - triple jeopardy for vulnerability to COVID-19 infection. EClinicalMedicine. 2020;22:100343. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 78. | Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med. 2020;8:e35. [PubMed] [Cited in This Article: ] |
| 79. | World Health Organization. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. [cited 14 Oct 2021]. In: World Health Organization [Internet]. Available from: https://www.who.int/publications/i/item/9789240010291. [Cited in This Article: ] |
| 80. | Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, Khunti K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14:965-967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 341] [Cited by in F6Publishing: 323] [Article Influence: 80.8] [Reference Citation Analysis (0)] |
| 81. | Pati S, Mahapatra P, Kanungo S, Uddin A, Sahoo KC. Managing Multimorbidity (Multiple Chronic Diseases) Amid COVID-19 Pandemic: A Community Based Study From Odisha, India. Front Public Health. 2020;8:584408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 82. | Singh K, Kondal D, Mohan S, Jaganathan S, Deepa M, Venkateshmurthy NS, Jarhyan P, Anjana RM, Narayan KMV, Mohan V, Tandon N, Ali MK, Prabhakaran D, Eggleston K. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021;21:685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 59] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 83. | World Health Organization. Opportunities and developments Report on the second global survey on eHealth Global Observatory for eHealth series-Volume 2 Telemedicine in Member States. 2010. [cited 14 Oct 2021]. In: World Health Organization [Internet]. Available from: https://apps.who.int/iris/handle/10665/44497. [Cited in This Article: ] |
| 84. | Sudhamony S, Nandakumar K, Binu PJ, Issac Niwas S. Telemedicine and tele-health services for cancer-care delivery in India. IET Commun. 2008;2:231. [DOI] [Cited in This Article: ] |
| 85. | Agarwal N, Jain P, Pathak R, Gupta R. Telemedicine in India: A tool for transforming health care in the era of COVID-19 pandemic. J Educ Health Promot. 2020;9:190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 86. | Kumar S, Kumar A, Kumar M, Arora R, Sehrawat R. Feasibility of telemedicine in maintaining follow-up of orthopaedic patients and their satisfaction: A preliminary study. J Clin Orthop Trauma. 2020;11:S704-S710. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 87. | Swetha NB, Shobha S, Sriram S. Prevalence of catastrophic health expenditure and its associated factors, due to out-of-pocket health care expenses among households with and without chronic illness in Bangalore, India: a longitudinal study. J Prev Med Hyg. 2020;61:E92-E97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 88. | Bhaduri SD. Post-COVID healthcare reform in India: What to expect? J Family Med Prim Care. 2020;9:5427-5431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 89. | Hindustan Time. India must act now to protect its health workers | Opinion - Hindustan Times. [cited 14 Nov 2021]. In: Hindustan Time [Internet]. Available from: https://www.hindustantimes.com/analysis/india-must-act-now-to-protect-its-health-workers/story-idWQ1uyMrnARHc3PH7W86J.html. [Cited in This Article: ] |
| 90. | Gan WH, Lim JW, Koh D. Preventing Intra-hospital Infection and Transmission of Coronavirus Disease 2019 in Health-care Workers. Saf Health Work. 2020;11:241-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 143] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 91. | Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8:434-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 728] [Cited by in F6Publishing: 677] [Article Influence: 169.3] [Reference Citation Analysis (0)] |
| 92. | Zhou P, Huang Z, Xiao Y, Huang X, Fan XG. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect Control Hosp Epidemiol. 2020;41:745-746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 91] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 93. | Sodhi K, Shrivastava A, Arya M, Kumar M. Knowledge of infection control practices among intensive care nurses in a tertiary care hospital. J Infect Public Health. 2013;6:269-275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 94. | Diwan V, Gustafsson C, Rosales Klintz S, Joshi SC, Joshi R, Sharma M, Shah H, Pathak A, Tamhankar AJ, Stålsby Lundborg C. Understanding Healthcare Workers Self-Reported Practices, Knowledge and Attitude about Hand Hygiene in a Medical Setting in Rural India. PLoS One. 2016;11:e0163347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 95. | Legido-Quigley H, Asgari N, Teo YY, Leung GM, Oshitani H, Fukuda K, Cook AR, Hsu LY, Shibuya K, Heymann D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395:848-850. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 295] [Cited by in F6Publishing: 258] [Article Influence: 64.5] [Reference Citation Analysis (0)] |
| 96. | Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J Med Internet Res. 2019;21:e11330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 196] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 97. | Snoswell CL, Taylor ML, Comans TA, Smith AC, Gray LC, Caffery LJ. Determining if Telehealth Can Reduce Health System Costs: Scoping Review. J Med Internet Res. 2020;22:e17298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 134] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 98. | Baishideng Publishing Group. Reference Citation Analysis. [cited 24 May 2022]. In: Baishideng Publishing Group [Internet]. Available from: https://www.referencecitationanalysis.com/. [Cited in This Article: ] |