Published online May 26, 2014. doi: 10.4330/wjc.v6.i5.345
Revised: February 10, 2014
Accepted: March 13, 2014
Published online: May 26, 2014
M Ebstein is usually diagnosed in early childhood or adolescence. The young woman in our case complainted of fatigue and shortness of breath, on physical examination she showed signs of heart failure with raised central venous pressure, palpable liver, an a cardiac murmer. Based on these findings she should have been referred to a cardiologist in an early stage after which transthoracic echocardiography resulted in the correct diagnosis. In this case the anomaly was missed for many years by different specialists and the patient was treated for liver disease, while she was suffering from liver congestion due to right-sided heart failure.
Core tip: The young woman in our case complainted of fatigue and shortness of breath, on physical examination she showed signs of heart failure with raised central venous pressure, palpable liver, an a cardiac murmer. Based on these findings she should have been referred to a cardiologist in an early stage after which transthoracic echocardiography resulted in the correct diagnosis.
- Citation: Vette LC, Brugts JJ, McGhie JS, Roos-Hesselink JW. Long-lasting symptoms and diagnostics in a patient with unrecognized right sided heart failure: Why listening to the heart is so important. World J Cardiol 2014; 6(5): 345-348
- URL: https://www.wjgnet.com/1949-8462/full/v6/i5/345.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i5.345
The anamnesis and physical examination have an essential role in the work-up of patients. The current case shows clearly that with thorough examination of the patients’story and physical examination, the majority of medical tests could have been prevented and the correct diagnosis been found earlier.
Our patient was born in 1978 after an uncomplicated pregnancy. In childhood, she was seen by a paediatrician because of recurrent tonsillitis and iron deficient anaemia and at the age of seven she experienced an episode of jaundice with urobilinogen in her urine with no clear explanation at that time.
At the age of 13, she complained of headaches and fatigue which were correlated to sinusitis. For pain relief she took paracetamol (acetaminophen) and ibuprofen in high dosages. At age 22, she was analysed at the department of internal medicine because of jaundice. She still complained of fatigue and anorexia now. Thorough screening revealed a solitary raised bilirubine, no serological evidence of viral infection, and no echographic abnormalities of the liver, gallbladder or biliary ducts. Two years later evaluation was repeated because of persisting elevated bilirubin levels. Due to headaches, she still used 3 g of paracetamol a day for years. The hyperbilirubinemia was now diagnosed as a toxic effect of this medication. After withdrawal of paracetamol, laboratory results did not improve and a liver biopsy was performed. This showed periportal fibrosis without cause. She was referred to the hepatologist for a second opinion and he found an irregular heart rate and referred her for cardiac consultation for the first time.
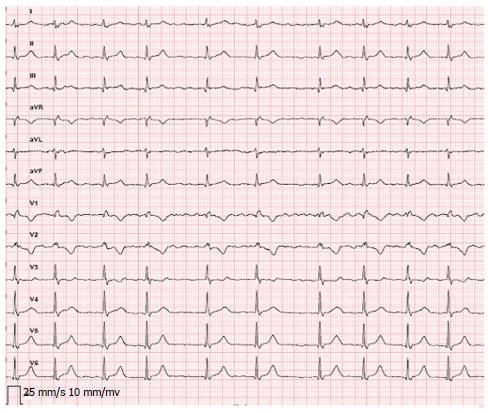
We saw a young woman with fatigue, shortness of breath and palpitations on minimal exercise. She could not work due to complaints. Additionally, several attempts to become pregnant were unsuccessful, which was severely stressful for her. Physical examination showed an icteric woman, irregular heart rate of 80 bpm with raised central venous pressure and 4 cm palpable liver. On cardiac auscultation a systolic murmur grade 2 out of 6 at the fourth intercostal space left and a soft diastolic murmur were heard. The electrocardiography (Figure 1) revealed atrial fibrillation with slow ventricular response and a QRS-complex with right bundle branch block configuration. Chest X-ray showed cardiomegaly (Figure 2). Echocardiography revealed an enlarged right heart with apical displacement of the tricuspid valve (Figure 3). A large part of the right ventricle (RV) was atrialized and in the enlarged RA a large mural thrombus was found (Figure 4). The interatrial septum bulged out towards the compressed left atrium consistent with high RA pressures. Low velocity antegrade flow was found in the main pulmonary artery, in systole and diastole, indicating the RV was functioning as a conduit.
The diagnosis of the congenital defect, Morbus Ebstein, was made which was complicated by intracardiac thrombus. Anticoagulants were started and further analysis showed a perfusion defect in the right lung, consistent with recurrent small pulmonary emboli. After successful treatment of the cardiac thrombus, heart catheterisation was performed (pulmonary artery pressure 13/12; wedge 11 mmHg). As pulmonary hypertension was excluded, fortunately she could be referred for surgical correction. The tricuspid valve was repaired according to Chavaud, and a Carpentier ring was implanted. The atrialized RV was reduced and because of the small dimension of the remaining RV, a partial cavo-pulmonal shunt from superior caval vein to right pulmonary artery (Glenn shunt) was constructed. The post-operative course was uncomplicated and her condition improved considerably. Echocardiography post-operatively showed mild tricuspid-valve insufficiency. One year after surgery, she became pregnant gave birth to a healthy baby. Currently, seven years after surgery, our patient is doing reasonably well and is in NYHA class I-II.
Our patient experienced many complaints since childhood which could have been prevented if the correct diagnosis of a congenital heart disease was made earlier. Morbus Ebstein is a rare disorder with a prevalence of about 1 in 50000-200000 and was first described by Ebstein[1]. In 1866, he published post-mortem analyses of a nineteen-year-old man who presented with dyspnoea, palpitations, systolic murmur, cyanosis and eventually clinical features of heart failure. Obduction showed a deformation of the tricuspid valve with displacement of the effective tricuspid valve orifice towards the apex. Severity of this tricuspid anomaly can vary substantially and can be associated with other defects such as atrial septal defect or patent foramen ovale, which is present in 70%-80% of the patients[2]. Other associated defects are ventricular septal defects with or without pulmonary atresia, patent ductus arteriosus or aortic coarctation.
M Ebstein is usually diagnosed in early childhood or adolescence. In this case the anomaly was missed for many years by different specialists and the patient was treated for liver disease, while she was suffering from liver congestion due to right-sided heart failure. The frequent use of paracetamol had put the clinicians on the wrong trail in interpreting the elevated liver enzymes, also a liver biopt could have been prevented. All her symptoms, the fatigue, shortness of breath and her inability to become pregnant were due to her cardiac situation. The right tract was started after listening to the heart.
The young woman in this case complainted of fatigue and shortness of breath, on physical examination she showed signs of heart failure with raised central venous pressue, palpable liver, an a cardiac murmer.
Initially the differential diagnosis of fatigue, jaundice and elevated liver enzymes is broad with primarily related to liver disease, medication effects but should incorporate a cardiac evaluation. With the progressive signs of right heart failure on physical examination, the suspicion of a cardiac diagnosis should have become stronger.
The hyperbilirubinemia was now diagnosed as a toxic effect of this medication.
Echocardiography revealed an enlarged right heart with apical displacement of the tricuspid valv.
The tricuspid valve was repaired according to Chavaud, and a Carpentier ring was implanted and the atrialized RV was reduced with a partial cavo-pulmonal shunt from superior caval vein to right pulmonary artery (Glenn shunt)
Ebstein is the name of the doctor who first described the anomaly.
The current case underlines the importance of physical examination and maintaining a broad view to a patients’problem.
The case report is well written and adresses common poblmes with diagnostics of Ebstein anomaly.
P- Reviewers: Aggarwal A, JuergensKU S- Editor: Zhai HH L- Editor: A E- Editor: Wu HL
| 1. | Ebstein W. Ueber einen sehr seltenen Fall von Insufficienz der Valvula tricuspidalis, bedingt durch eine angeborene hochgradige Missbildung derselben. Arch Anat Physiol. 1966;238-255. [Cited in This Article: ] |
| 2. | Attenhofer Jost CH, Connolly HM, O’Leary PW, Warnes CA, Tajik AJ, Seward JB. Left heart lesions in patients with Ebstein anomaly. Mayo Clin Proc. 2005;80:361-368. [PubMed] [Cited in This Article: ] |