Abstract
BACKGROUND: Decreasing the amount of iodinated contrast is an important safety aspect of percutaneous coronary interventions (PCI), particularly in patients with a high risk of contrast-induced acute kidney injury (CI-AKI). Dynamic Coronary Roadmap (DCR) is a PCI navigation support tool projecting a motion-compensated virtual coronary roadmap overlay on fluoroscopy, potentially limiting the need for contrast during PCI.
AIMS: This study investigates the contrast-sparing potential of DCR in PCI, compared to standard angiographic guidance.
METHODS: The Dynamic Coronary Roadmap for Contrast Reduction (DCR4Contrast) trial is a multicentre, international, prospective, unblinded, stratified 1:1 randomised controlled trial. Patients were randomised to either DCR-guided PCI or to conventional angiography-guided PCI. The primary endpoint was the total volume of iodinated contrast administered, and the secondary endpoint was the number of cineangiography runs during PCI.
RESULTS: The study population included 356 randomised patients (179 in DCR and 177 in control groups, respectively). There were no differences in patient demographics, angiographic characteristics or estimated glomerular filtration rate (eGFR) between the two groups. The total contrast volume used during PCI was significantly lower with DCR guidance compared with conventional angiographic guidance (64.6±44.4 ml vs 90.8±55.4 ml, respectively; p<0.001). The total number of cineangiography runs was also significantly reduced in the DCR group (8.7±4.7 vs 11.7±7.6 in the control group; p<0.001).
CONCLUSIONS: Compared to conventional angiography-guided PCI, DCR guidance was associated with a significant reduction in both contrast volume and the number of cineangiography runs during PCI. (ClinicalTrials.gov: NCT04085614)
The risk profile of patients undergoing percutaneous coronary intervention (PCI) has steadily increased over the last decade1. This shift is a result not only of a change in demographics, which includes more elderly patients, but also of a more frequent treatment of individuals with long-standing cardiac disease, more advanced atherosclerosis and prior coronary revascularisation, challenging anatomical scenarios, and concomitant systemic conditions, resulting in an increased risk of cardiac and non-cardiac complications of PCI. Part of the risk of PCI in these scenarios stems from the need to use iodinated contrast in patients who are highly susceptible of developing contrast-induced acute kidney injury (CI-AKI).
The occurrence of CI-AKI entails poorer clinical outcomes and increased economic burdens, and implementing measures for its prevention has been encouraged in clinical practice guidelines23456789. Whilst the development of CI-AKI is multifactorial, it is widely accepted that the amount of iodinated contrast administered during PCI is one of the most significant contributors to the development of CI-AKI4101112.
New software augmentation tools capable of displaying a coronary reference image superposed upon the fluoroscopic image used by the PCI operator have the potential to reduce contrast volume131415. Dynamic Coronary Roadmap (DCR; Philips Medical Systems) is a commercially available, proprietary software tool that facilitates navigation of PCI devices using a single contrast injection. The DCR system provides an automated, real-time and dynamic angiographic roadmap of the coronary arteries overlaid on live fluoroscopy (Figure 1, Moving image 1). In this context, DCR has the potential to reduce overall contrast burden by reducing the need for the additional contrast puffs normally required for the navigation and advancement of coronary wires, balloons and stents in the coronary arteries. The potential value of DCR in reducing the overall contrast burden during PCI has previously been supported by single-centre studies only131415. The Dynamic Coronary Roadmap for Contrast Reduction (DCR4Contrast) trial was designed to prospectively investigate the potential benefit of DCR in terms of a reduction in contrast administered as well as the number of cineangiography runs obtained during PCI procedures.
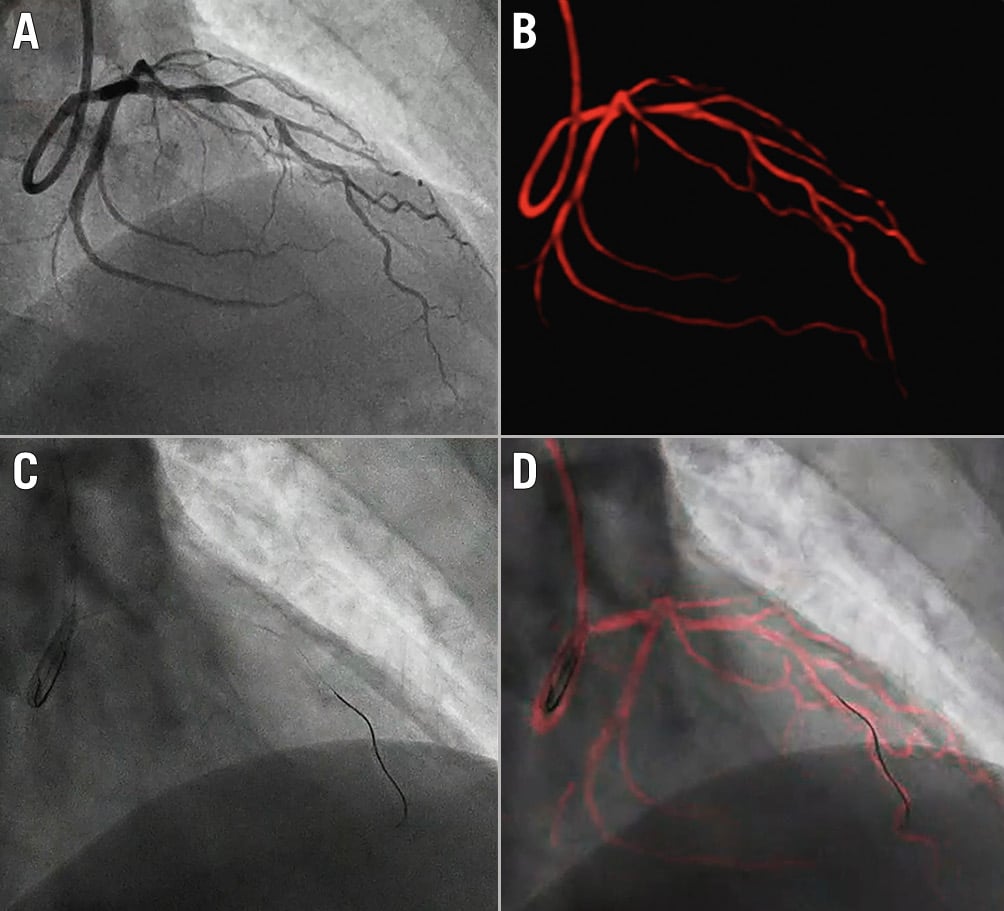
Figure 1. Philips Dynamic Coronary Roadmap navigational tool for vessel wiring and stent placement. A) A cineangiogram is obtained with a single contrast injection in the coronary arteries. B) Dynamic Coronary Roadmap (DCR) automatically converts this angiogram into a heart cycle of roadmap masks. C) For the subsequent live fluoroscopy image, DCR finds the best-matching roadmap mask and projects it as a real-time, motion-compensated dynamic overlay of the coronary tree (in red) on fluoroscopy to assist device navigation during PCI (D). PCI: percutaneous coronary intervention
Methods
The rationale and design of the DCR4Contrast trial has been previously published16. In brief, DCR4Contrast was an international, multicentre, prospective, unblinded, stratified 1:1 randomised controlled trial. The study was conducted in six tertiary referral centres in Europe (N=3), Israel (N=1) and the USA (N=2). Patients undergoing non-emergent PCI (either ad hoc or planned) were randomised to undergo PCI performed either under DCR guidance (treatment group) or using conventional angiographic guidance (control group). Balanced randomisation was performed according to the type of procedure (ad hoc or planned) and the number of vessels scheduled to be treated.
PATIENT POPULATION
The study population included patients over 18 years of age, with a signed consent form, who were undergoing non-emergent PCI with a degree of complexity that anticipated the need for more than 25 ml of iodinated contrast volume (Supplementary Figure 1). Supplementary Table 1 contains the full list of inclusion and exclusion criteria. Patients with chronic kidney disease stage 5 (estimated glomerular filtration rate [eGFR] <15 ml/min/1.73 m2) were excluded. Patients who were randomised to the DCR group underwent PCI using the in-room DCR technology to aid in the advancement of coronary wires, balloons, stents and other PCI diagnostic or therapeutic hardware.
STUDY OBJECTIVES AND ENDPOINTS
The primary objective of this trial was to assess whether using DCR reduces the amount of total iodinated contrast volume required per PCI procedure (primary endpoint), compared to the control group without DCR. The secondary objective was to assess the total number of contrast-enhanced cineangiographic runs per PCI procedure (secondary endpoint) in the DCR and control arms. The study was powered to demonstrate the superiority of DCR versus standard angiographic guidance for both the primary and secondary objectives. The study also included several prespecified exploratory objectives as described in Supplementary Table 2.
PERCUTANEOUS CORONARY INTERVENTION AND DATA COLLECTION
Patients assigned to the standard angiography-guided arm underwent PCI without DCR. In both arms, the operator was expected to follow their normal clinical practice for PCI and the treatment of coronary artery disease (CAD). The SYNTAX score17 in PCI-treated vessels was calculated as a metric of anatomical vessel complexity. The steps required for PCI in both groups are outlined in Supplementary Table 3. All data were entered into the electronic Case Report Form (eCRF), which included patient demographics, relevant past medical history, specific target CAD data along with preprocedural/screening imaging details, PCI procedural data and follow-up data until patient discharge.
STATISTICAL ANALYSIS
Statistical analyses were performed using SAS (SAS Institute) and/or R statistical software (R Foundation for Statistical Computing). Standard statistical methods were used for summarisation and analysis. Data are presented as mean±standard deviation with 95% confidence intervals for continuous variables with a normal distribution, as median (interquartile range) for continuous variables with a non-normal distribution, and as frequency (%) for categorical variables.
Differences in the primary and continuous exploratory endpoints between the study arms were evaluated using a one-sided two-sample t-test. We tested for assumptions, e.g., normality and equal variances. If there were strong indications of non-normality, the data were log-transformed before we performed the t-test. If the variances differed, we performed an unequal variance t-test. The secondary endpoint (number of angiograms) was discrete and was likely to be not normally distributed, so differences in this endpoint between the study arms were evaluated using a one-sided Mann-Whitney U test (Supplementary Figure 2). When the p-value was lower than the significance level of 2.5% (alpha), the null hypothesis was rejected.
Differences in categorical exploratory endpoints were tested using a Chi-Square test or Fisher’s exact test, as appropriate. Baseline demographics and baseline clinical and procedural characteristics were tested using a t-test or Mann-Whitney U test for continuous variables and the Chi-Square test or Fisher’s exact test for categorical variables. A two-sided alpha level of 5% was used for these analyses.
It was prespecified that the primary analysis was to be performed upon patients undergoing PCI; we therefore excluded patients who did not undergo a PCI following randomisation from the full analysis set. Furthermore, in order to ensure the homogeneity of the study population, we prespecified that for cases in which optical coherence tomography (OCT) and/or rotational or orbital atherectomy were used in enrolled patients, these subjects were to be replaced. Each of these patients remained part of the safety population, and an additional patient was randomised to preserve power for the full analysis population. A sensitivity analysis of all randomised patients (irrespective of whether PCI, OCT, or atherectomy was performed) was analysed according to the treatment group.
The study was approved by the institutional review board or medical ethics committee of the participating hospitals. All enrolled eligible patients provided written informed consent. The trial was funded by Philips Medical Systems (Best, the Netherlands). This trial is registered at ClinicalTrials.gov: NCT04085614.
Results
Between November 2019 and February 2023, a total of 371 patients were enrolled and randomised in six centres. Figure 2 summarises patient flow within the study. In total, 15 patients were excluded from the study due to various reasons (Figure 2). The final study population who were eligible for analysis included 356 patients randomised to either the DCR-guided PCI group (179 patients) or the angiography-guided PCI group (177 patients). There were no significant differences in patient demographics or clinical characteristics between the two groups (Table 1).
Table 2 shows the procedural details for both study arms. Overall, there was a small preponderance of ad hoc (226/356, 63%) over planned PCI procedures (130/356, 37%) but there were no other differences between the study arms. Most interventions were single-vessel disease PCI (303/356, 85%). Of note, intravascular ultrasound (IVUS) was used in 37% of PCI cases (133/356), without differences between the study arms.
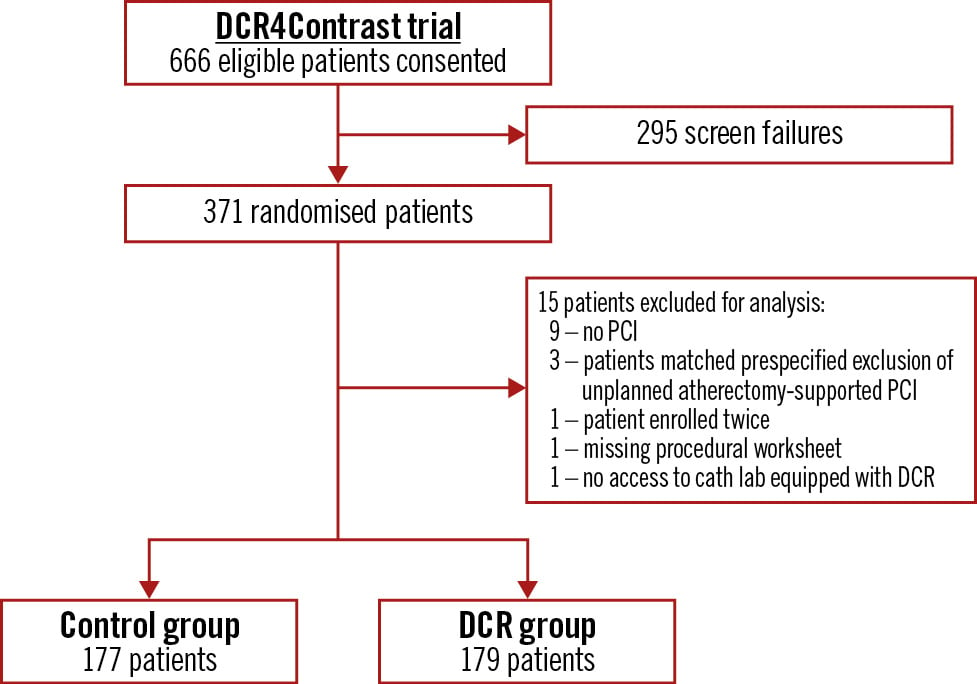
Figure 2. Study flow of the DCR4Contrast randomised controlled trial. DCR: Dynamic Coronary Roadmap; PCI: percutaneous coronary intervention
Table 1. Baseline demographics and clinical procedural characteristics of PCI patients randomised to the DCR and control arms.
| DCR (n=179) | Control (n=177) | p-value | |
|---|---|---|---|
| Age, years | 65.8±10.8 | 65.9±10.9 | 0.958 |
| Male | 143 (79.9) | 139 (78.5) | 0.752 |
| Weight, kg | 85.1±20.0 | 83.1±15.6 | 0.283 |
| Body mass index, kg/m2 | 28.9±5.7 | 28.5±4.8 | 0.538 |
| Diabetes mellitus | 66 (36.9) | 68 (38.4) | 0.859 |
| Hypertension (>140/90 mmHg) | 135 (75.4) | 124 (70.1) | 0.158 |
| Chronic kidney disease | 18 (10.1) | 26 (14.7) | 0.204 |
| Prior revascularisation | 62 (34.6) | 60 (33.9) | 0.793 |
| Coronary artery bypass graft | 12 (6.7) | 15 (8.5) | 0.558 |
| Prior myocardial infarction | 55 (30.7) | 54 (30.5) | 0.880 |
| Severe left ventricular ejection fraction (<30%) | 2 (1.1) | 6 (3.4) | 0.160* |
| eGFR, ml/min/1.73 m2 | 77.5±19.7 | 75.5±19.9 | 0.244 |
| Data given as number (%) or mean±standard deviation. The Chi-Square test or Fisher’s exact test were used for categorical variables. *Fisher’s exact test, the t-test or Mann-Whitney U test were used for continuous variables. DCR: Dynamic Coronary Roadmap; eGFR: estimated glomerular filtration rate; PCI: percutaneous coronary intervention | |||
Table 2. Procedural characteristics of PCI patients randomised to the DCR and control arms.
| DCR (n=179) | Control (n=177) | p-value | ||
|---|---|---|---|---|
| Type of PCI | Ad hoc PCI | 110 (61.5) | 116 (65.5) | 0.424 |
| Planned PCI | 69 (38.5) | 61 (34.5) | ||
| Number of vessels treated with PCI | 1 | 157 (87.7) | 146 (82.5) | 0.263* |
| 2 | 18 (10.1) | 28 (15.8) | ||
| 3 | 4 (2.2) | 3 (1.7) | ||
| Treated vessel | Left main artery | 5 (2.8) | 4 (2.3) | >0.99* |
| Left anterior descending artery | 91 (50.8) | 89 (50.3) | 0.917 | |
| Left circumflex artery | 52 (29.1) | 58 (32.8) | 0.448 | |
| Right coronary artery | 49 (27.4) | 49 (27.7) | 0.948 | |
| Lesion complexity | Lesion length >20 mm | 100 (55.9) | 107 (60.5) | 0.346 |
| Heavy calcification | 30 (16.8) | 26 (14.7) | 0.608 | |
| Bifurcation lesion | 41 (22.9) | 53 (29.9) | 0.140 | |
| Trifurcation lesion | 2 (1.1) | 1 (0.6) | >0.99* | |
| Severe tortuosity | 12 (6.7) | 11 (6.2) | 0.862 | |
| Thrombotic lesion | 6 (3.4) | 6 (3.4) | 0.968 | |
| Aorto-ostial stenosis | 1 (0.6) | 1 (0.6) | >0.99* | |
| Diffusely diseased and narrowed lesion | 29 (16.2) | 39 (22.0) | 0.161 | |
| PCI complexity score (SYNTAX score per PCI treated vessel, SSv) | 1st tertile (low) (n=116) | 2.2±0.9 | 2.3±0.7 | 0.946 |
| 2nd tertile (medium) (n=128) | 5.6±1.1 | 5.7±1.1 | ||
| 3rd tertile (high) (n=112) | 10.0±2.4 | 9.9±2.1 | ||
| Lesions treated per procedure | 1.2±0.4 | 1.2±0.4 | 0.183 | |
| Stents per procedure | 0 | 4 (2.2) | 1 (0.6) | 0.309* |
| 1 | 121 (67.6) | 111 (62.7) | ||
| 2 | 40 (22.3) | 44 (24.9) | ||
| 3 | 9 (5.0) | 18 (10.2) | ||
| 4 | 3 (1.7) | 2 (1.1) | ||
| 5 | 2 (1.1) | 1 (0.6) | ||
| Total stent length, mm | 31.9±21.1 | 35.1±21.2 | 0.088 | |
| IVUS use | 73 (40.8) | 60 (33.9) | 0.179 | |
| Physiology assessment (iFR/FFR) | 15 (8.4) | 11 (6.2) | 0.432 | |
| Data given as number (%) or mean±standard deviation. The Chi-Square test or Fisher’s exact test were used for categorical variables. *Fisher’s exact test, the t-test or Mann-Whitney U test were used for continuous variables. DCR: Dynamic Coronary Roadmap; FFR: fractional flow reserve; iFR: instantaneous wave-free ratio; IVUS: intravascular ultrasound; PCI: percutaneous coronary intervention; SSv: SYNTAX score per PCI-treated vessel | ||||
CONTRAST USE DURING PCI
Regarding the primary objective of the study, a significantly lower volume of iodinated contrast was used during PCI in the DCR-guided group (64.6±44.4 ml), compared with the conventional angiography-guided group (90.8±55.4 ml; p<0.001) (Central illustration, Figure 3, Table 3). With regard to the secondary objective, a significantly lower number of cineangiograms were performed in the DCR-guided group (8.7±4.7), compared with the conventional angiography-guided group (11.7±7.6; p<0.001) (Table 3, Figure 3).
In addition, the primary analysis was repeated using “worst case” imputation for missing values as a sensitivity analysis and showed a similar effect, as described and shown in Supplementary Table 4. The primary and secondary outcomes were also similar when considering all randomised patients (Supplementary Table 5). There was no centre-specific effect on the primary outcome (intraclass correlation coefficient of 0.06 for the log-transformed primary endpoint). For both the ad hoc PCI and planned PCI subgroups, the iodinated contrast volume was significantly lower in the DCR group, compared to the control group, and a greater difference was noted for the DCR group undergoing planned PCI (Supplementary Table 6).
A prespecified subgroup analysis was performed based on 1) the number of vessels in which PCI was performed and 2) the SYNTAX score of the treated vessel (SSv) (Table 3). The beneficial effect of DCR-guided over angiography-guided PCI regarding the primary endpoint (contrast volume) was consistent across different subgroups (Figure 4). Significantly less contrast volume per PCI was used in the DCR group, irrespective of whether it was a single-vessel (58.2±34.5 ml in DCR vs 82.4±52.7 ml in control arm; p<0.001) or a multivessel procedure (110.2±73.1 ml in DCR vs 130.4±51.4 ml in control arm; p=0.046) (Table 3). In terms of anatomical PCI complexity, a greater difference in contrast volume favouring the DCR arm was noted for the 2nd and 3rd tertile of the treated vessel SYNTAX score values (SSv ≥4 points), with no significant differences noted in treated vessels with a SSv <4 points (Table 3, Figure 4).
There were no significant differences in fluoroscopy time (12.6±11.1 min in DCR vs 12.9±11.6 min in control arm; p=0.568), procedural time (33.7±25.9 min in DCR vs 36.1±30.5 min in control arm; p=0.286), X-ray radiation dose (air kerma 535.3±396.2 mGy in DCR vs 629.0±649.5 mGy in control arm; p=0.206; dose area product 44.3±57.6 Gy*cm2 in DCR vs 45.5±63.1 Gy*cm2 in control arm; p=0.689), procedural success (99.4% in DCR vs 100% in control arm;p>0.99). In addition, the rates of in-hospital acute kidney injury (1.7% in DCR vs 2.3% in control arm; p=0.723) and in-hospital peri-/postinterventional major adverse cardiovascular and cerebral events (MACCE) (0.6% in DCR vs 0% in control arm;p>0.99) were similarly low in both groups.
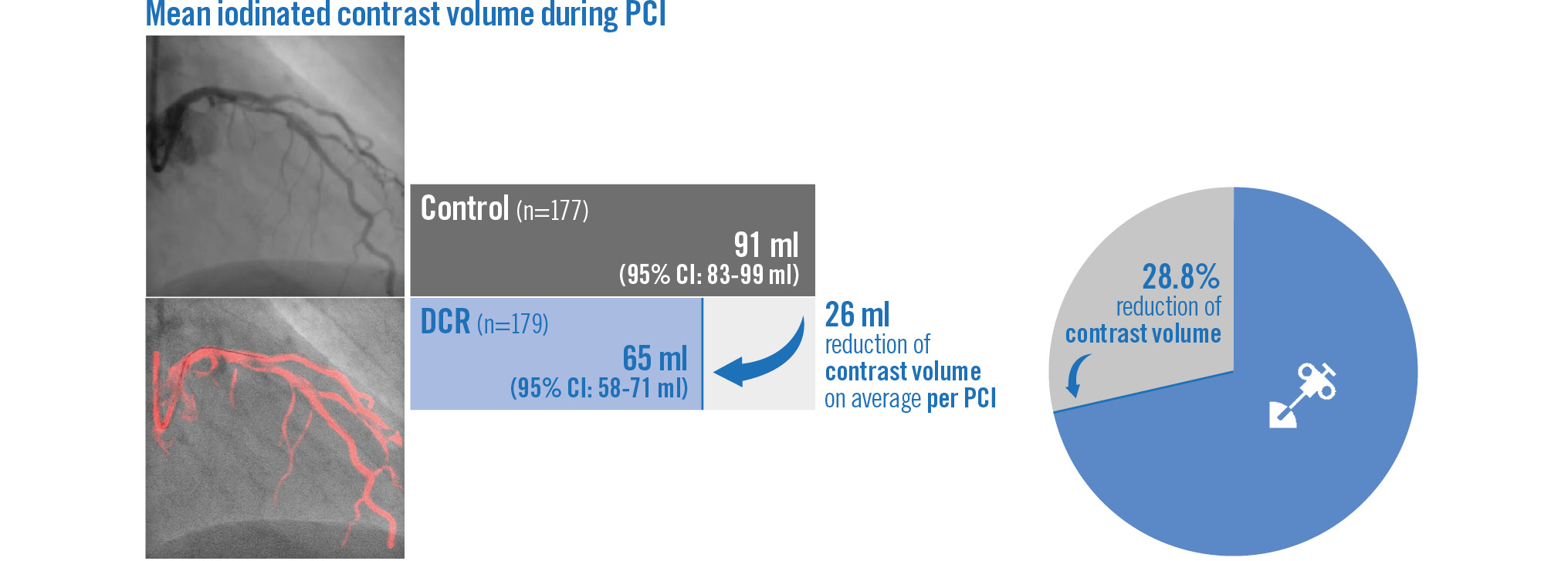
Central illustration. Iodinated contrast volume utilisation in Dynamic Coronary Roadmap versus standard angiography-guided percutaneous coronary intervention: the randomised, multicentre DCR4Contrast trial. DCR: Dynamic Coronary Roadmap; PCI: percutaneous coronary intervention
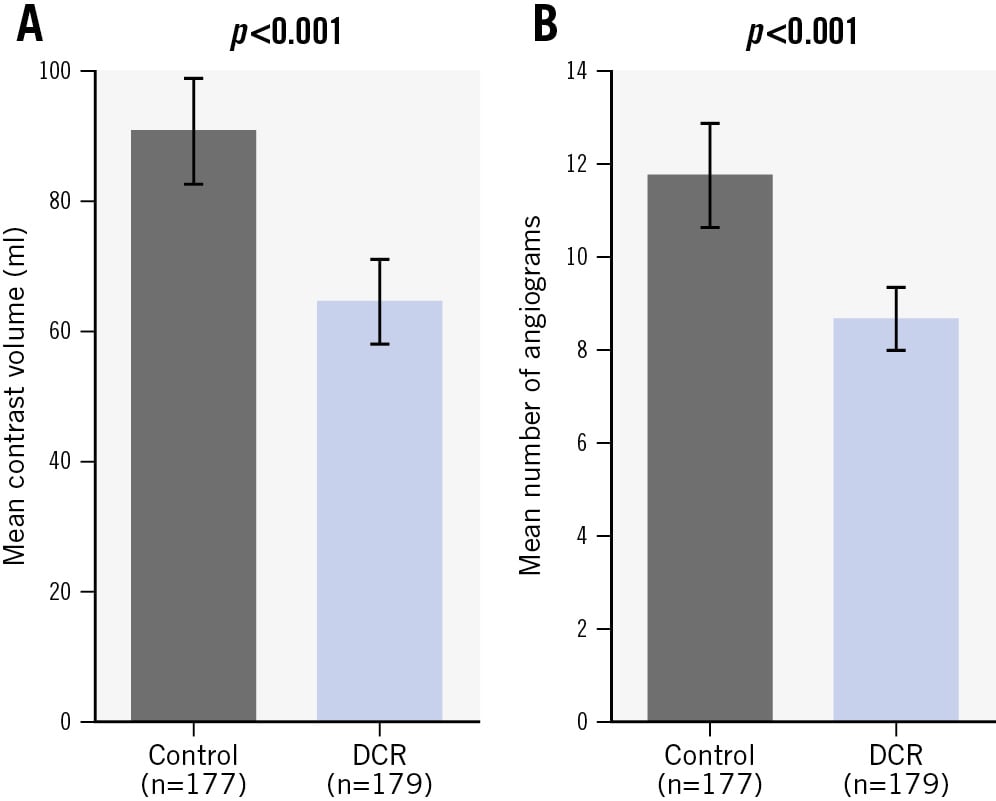
Figure 3. Primary and secondary outcomes of the DCR4Contrast randomised controlled trial. A) Mean contrast volume used per PCI (primary objective) and B) mean number of cineangiograms obtained per PCI (secondary objective) in the DCR and control groups. The error bars represent the 95% confidence interval of the mean, and the p-value is based on log-transformed data. DCR: Dynamic Coronary Roadmap; PCI: percutaneous coronary intervention
Table 3. Primary, secondary and exploratory outcomes of the DCR4Contrast trial.
| Per PCI procedure | DCR (n=179) | Control (n=177) | p-value |
|---|---|---|---|
| Primary endpoint: iodinated contrast volume, ml | <0.001# | ||
| Mean±SD | 64.6±44.4 | 90.8±55.4 | |
| 95% CI of mean | 58.0-71.1 | 82.5-99.0 | |
| Median [IQR] | 55.0 [33.0-88.0] | 77.4 [50.4-119.0] | |
| Secondary endpoint: number of contrast-enhanced cineangiographic X-ray runs | <0.001† | ||
| Mean±SD | 8.7±4.7 | 11.7±7.6 | |
| 95% CI of mean | 8.0-9.4 | 10.6-12.9 | |
| Median [IQR] | 8 [5-11] | 10 [7-14] | |
| Exploratory endpoints | |||
| Contrast volume, ml, per | |||
| Single-vessel PCI | 58.2±34.5 | 82.4±52.7 | <0.001# |
| 52.0 [33.0-74.0] | 66.0 [48.0-107.3] | ||
| Multivessel PCI | 110.2±73.1 | 130.4±51.4 | 0.046# |
| 91.5 [63.0-143.0] | 119.0 [96.0-167.7] | ||
| Contrast volume, ml, per PCI complexity (SYNTAX score per PCI-treated vessel) | |||
| 1st tertile (low; SSv <4) | 60.9±34.1 | 64.9±41.7 | 0.365# |
| 55.0 [35.8-79.0] | 54.5 [37.0-83.0] | ||
| 2nd tertile (medium; 4≤ SSv <8) | 62.9±47.8 | 92.9±51.7 | <0.001# |
| 49.0 [30.0-75.0] | 78.5 [52.8-122.0] | ||
| 3rd tertile (high; SSv ≥8) | 70.4±49.6 | 115.2±60.7 | <0.001# |
| 62.0 [34.3-90.0] | 109.4 [75.0-144.7] | ||
| Acute kidney injury | 3 (1.7) | 4 (2.3) | 0.723* |
| Fluoroscopy time, min | 12.6±11.1 | 12.9±11.6 | 0.568# |
| 9.2 [5.6-15.8] | 9.3 [5.2-16.3] | ||
| PCI procedure time, min | 33.7±25.9 | 36.1±30.5 | 0.286# |
| 28 [16-42] | 28 [15-45] | ||
| Air kerma, mGy | 535.3±396.2 | 629.0±649.5 | 0.206# |
| 437.0 [263.0-675.0] | 425.0 [241.0-779.9] | ||
| Dose area product, Gy*cm2 | 44.3±57.6 | 45.5±63.1 | 0.689# |
| 30.7 [16.8-52.9] | 28.0 [13.7-53.6] | ||
| Procedural success | 178 (99.4) | 177 (100) | >0.99* |
| In-hospital MACCE | |||
| Peri-interventional | 0 (0) | 0 (0) | >0.99* |
| Postinterventional | 1 (0.6) | 0 (0) | >0.99* |
| Data given as number (%), mean±SD or median [IQR]. The Chi-Square test or Fisher’s exact test were used for categorical variables; *Fisher’s exact test, #one-sided p-value t-test on log-transformed data, or †one-sided p-value Mann-Whitney U test were used for continuous variables. CI: confidence interval; DCR: Dynamic Coronary Roadmap; IQR: interquartile range; MACCE: major adverse cardiovascular and cerebral events; PCI: percutaneous coronary intervention; SD: standard deviation; SSv: SYNTAX score per PCI-treated vessel | |||
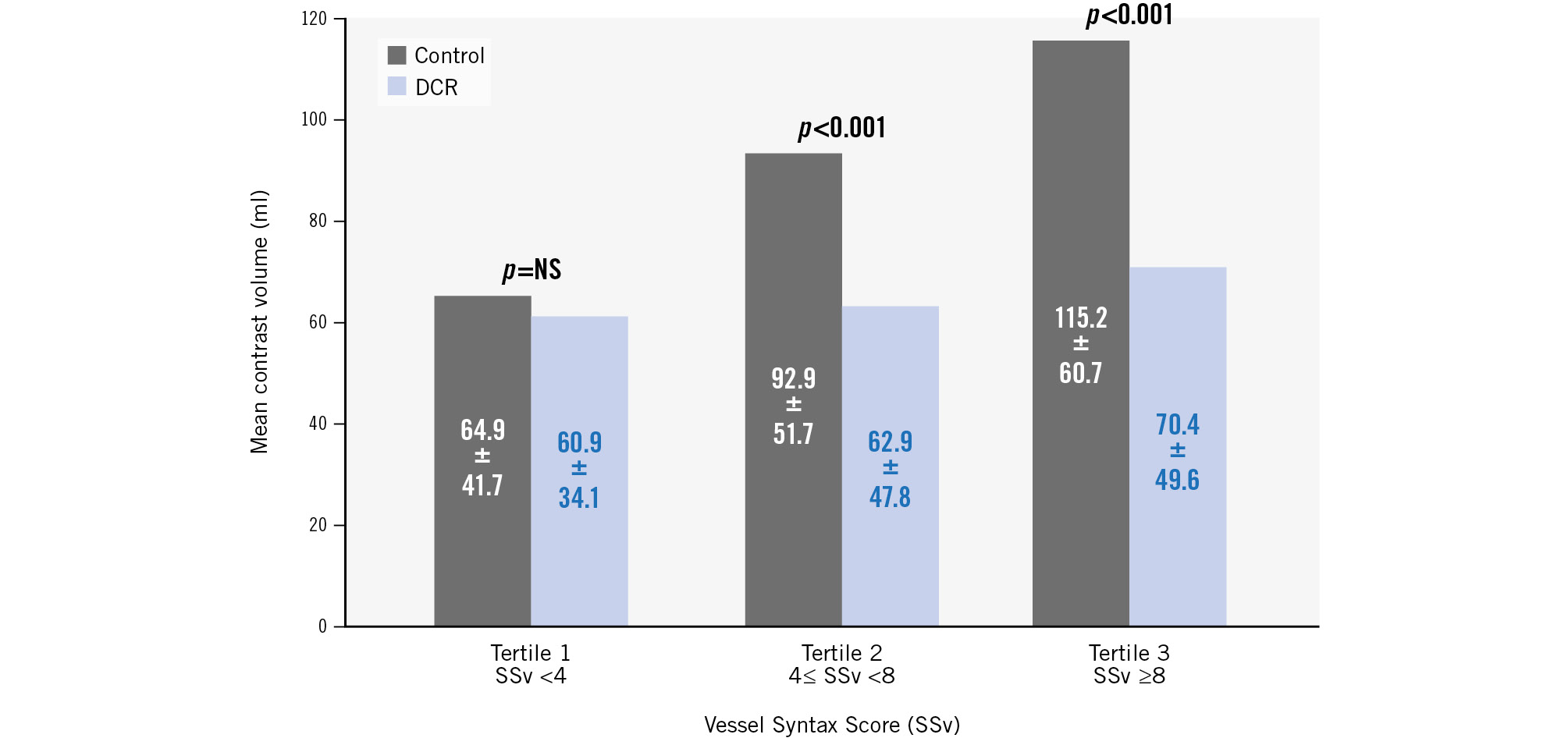
Figure 4. Contrast volume outcomes for treated vessels’ SYNTAX score (SSv) subgroups. Contrast volume used according to tertiles of SSv, showing an increasingly greater difference in contrast volume between randomised arms among procedures with higher SSv. DCR: Dynamic Coronary Roadmap; NS: not significant; PCI: percutaneous coronary intervention
Discussion
The results of the DCR4Contrast trial show that PCI guided with the Dynamic Coronary Roadmap system was associated with a significant reduction in the amount of iodinated contrast and the number of cineangiograms utilised to perform the intervention, compared to standard angiography-guided PCI.
In the context of increasing complexity and risk profile of patients undergoing PCI, a reduction in contrast volume and cineangiography runs may contribute not only to improved safety of the PCI procedure (i.e., by reducing the chances of CI-AKI) but also may allow completion of complex interventions without being hampered by reaching contrast volume limits and radiation that might necessitate termination or staging of the procedure. Ultra-low contrast and complex high-risk indicated PCI (CHIP) indications have gained significant traction in recent years, and DCR has the potential to become an important part of this toolbox.
The DCR4Contrast trial was preceded by smaller studies whose findings were, overall, concordant with ours in showing a reduction of contrast volume associated with DCR1314151819. Of these studies, it is worth highlighting a single small, randomised controlled trial by Piayda et al in patients with type A or B lesions, which demonstrated lower contrast volume for PCI in the DCR arm (36.8±19.2 ml), compared to the angiography-guided arm (69.4±27.3 ml; p<0.001)1819. In contrast with that study, our trial included a more complex profile of lesions (i.e., length of >20 mm, bifurcations or heavy calcification, or multivessel disease) (Table 2), which probably explains the higher contrast volumes used both in the DCR and control arms. This was the result of including PCI procedures with a degree of complexity that anticipated the need for more than 25 ml of iodinated contrast volume in the trial, i.e., excluding very straightforward PCI that did not require any navigational guidance. By enrolling patients with more challenging anatomies representative of real-world practice, we were able to detect a link between procedural complexity, as measured with the treated vessel SYNTAX score, and the benefit of DCR regarding the primary outcome. All this provides an additional argument in favour of its use in complex PCI cases.
Our trial also demonstrated the value of DCR in reducing the number of cineangiograms during PCI. This may be due to the fact that, over the course of a PCI procedure, DCR is used for purposes other than just navigating guidewires, such as positioning balloons and stents or correlating IVUS and physiology with coronary anatomy (Supplementary Figure 3). We did not observe a reduction in fluoroscopy times (12.6±11.1 min in DCR vs 12.9±11.6 min in control arm; p=0.568), but this can be explained by the fact that fluoroscopy is still required to display the Dynamic Coronary Roadmap overlay for navigation guidance. Along the same lines, it was also noted that the procedural time was similar in both groups (33.7±25.9 min in DCR vs 36.1±30.5 min in control arm; p=0.286).
Our study was not powered to detect differences in procedural success or clinical outcomes. As expected, procedural success was very high (99.4% in DCR group vs 100% in the standard angiography-guided arm), and the incidence of MACCE during the postinterventional in-hospital stay was very low, with one case of in-hospital death unrelated to the PCI procedure. In the same way, the study was not designed to detect the potential protective effect of DCR against CI-AKI. In addition to this, we excluded patients with chronic kidney disease stage 5 (eGFR <15 ml/min/1.73 m2).
Limitations
Our trial was inherently unblinded, since DCR is a visualisation tool; this may constitute a cause of bias. The benefits of DCR have not been demonstrated in the PCI subsets that were excluded from the study: ST-elevation myocardial infarction, chronic total occlusion, isolated ostial lesions and heavily calcified cases in which atherectomy was planned. The trial excluded patients with end-stage renal disease (stage 5; eGFR <15 ml/min/1.73 m2), which is precisely the group of patients who would likely benefit from a reduced contrast volume. These patients were excluded because of ethical reasons, since these patients should all undergo ultra-low contrast PCI. The study population had a relatively low CI-AKI risk (eGFR 77.5±19.7 in DCR vs 75.5±19.9 ml/min/1.73 m2 in control arm), which is also reflected by the low occurrence of AKI (1.7% in DCR vs 2.3% in control arm). Underdetection of CI-AKI may have occurred given that the majority of patients were discharged within 24 hours, in keeping with institutional standard practices, and therefore, serial measurements of serum creatinine levels over at least 48 hours might not have been performed.
Recalculation of the study population size was performed during the trial. During the design phase of this trial, it was initially calculated that 394 patients would be required for the study, based on a sample size calculation for the primary and secondary endpoints, including applying an attrition rate of 10%. The attrition rate was found to be much lower in practice; therefore, inclusion was stopped once the required 177 patients per arm (full analysis population) were included in both arms.
Conclusions
In conclusion, amongst patients undergoing non-emergent PCI, DCR was associated with both significantly less total iodinated contrast volume and a reduced number of contrast-enhanced cineangiograms per PCI, compared to standard angiographic procedural guidance. It is anticipated that DCR may play a valuable role in complex PCI cases, contributing to an increase in procedural safety and to complete revascularisation.
Impact on daily practice
The multicentre, international, randomised controlled DCR4Contrast trial has demonstrated the contrast-sparing effect of the DCR navigation support tool in patients undergoing PCI compared to standard angiographic guidance. This study shows that the DCR technology can be applied to varied clinical settings and PCI complexities. By reducing iodinated contrast administration, DCR may become an important part of the PCI toolbox and could contribute to reduced risk of contrast-induced acute kidney injury in higher-risk patients, thus increasing PCI safety.
Acknowledgements
The authors would like to acknowledge Iris ter Horst (Philips Medical Systems, Best, the Netherlands), for her input in the study design and early study support, and Petra Koopmans and Lieke Egbers (both Philips Medical Systems, Best, the Netherlands), for their statistical support in the study.
Funding
Philips Medical Systems (Best, the Netherlands) was the sponsor of this trial.
Conflict of interest statement
B. Hennessey is a speaker at educational events for Philips. H. Danenberg is a proctor for Medtronic and Edwards Lifesciences; and has received an institutional grant from Abbott. F. De Vroey is a speaker at educational events for Abbott. A.J. Kirtane has received institutional funding to Columbia University and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott, Amgen, CSI, Philips, ReCor Medical, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, Shockwave Medical, and Merck; is a consultant for IMDS; and received travel expenses/meals from Amgen, Medtronic, Biotronik, Boston Scientific, Abbott, CathWorks, Edwards Lifesciences, CSI, Novartis, Philips, Abiomed, Merck, ReCor Medical, Chiesi, Zoll, Shockwave Medical, and Regeneron in addition to research grants, institutional funding received includes fees paid to Columbia University and/or Cardiovascular Research Foundation for consulting and/or speaking engagements in which Dr Kirtane controlled the content. M. Parikh has served on advisory boards for Medtronic, Boston Scientific, and Abbott. D. Karmpaliotis has received honoraria from Boston Scientific, Abbott, Teleflex, and Abiomed; and has equity in Saranas, Soundbite, Traverse Vascular, and Nanowear. J.C. Messenger has received institutional grant support from Philips Medical Systems. M.S. van Mourik is an employee of Philips Medical Systems. P. Eshuis is an employee of Philips Medical Systems. J. Escaned is an advisory board member and speaker at educational events for Philips. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Dynamic Coronary Roadmap – a navigational tool for PCI: the Dynamic Coronary Roadmap technology automatically analyses a coronary angiogram for contrast and converts the angiogram into a series of masks spanning one heart cycle. The subsequent live fluoroscopy imaging is analysed for the catheter curve and wire shape to find the best matching angiographic roadmap mask from this series and update the red-coloured roadmap overlay in real time.